
|
|
Lecture notes, cheat sheets
Hospital therapy. Cheat sheet: briefly, the most important
Directory / Lecture notes, cheat sheets Table of contents
1. Rheumatism. Etiology and pathogenesis Rheumatism (Sokolsky-Buyo disease) is a systemic inflammatory disease of the connective tissue with a predominant localization of the process in the cardiovascular system, which develops in persons predisposed to it (as a rule, these are young people) due to an acute infection with group b-hemolytic streptococcus BUT. This definition of the disease was given in 1989 by V. A. Nasonov. The defeat of other organs and systems in rheumatism is of secondary importance and does not determine its severity and subsequent prognosis. Etiology. Group A beta-hemolytic streptococci cause upper respiratory infections. That is why the onset of rheumatism, as a rule, is preceded by angina, exacerbation of chronic tonsillitis, and in the blood of patients an increased amount of streptococcal antigen and anti-streptococcal antibodies (ASL-O, ASG, ASA, antideoxyribonuclease B (anti-DNase B)) are detected. In the development of rheumatism, age and social factors (adverse living conditions, malnutrition) play a role, and genetic predisposition also matters (rheumatism is a polygenically inherited disease, the existence of "rheumatic" families is well known), which consists in a hyperimmune response to streptococcus antigens, the propensity of patients to autoimmune and immunocomplex processes. Pathogenesis. In rheumatism, a complex and diverse immune response (hypersensitivity reactions of immediate and delayed types) to numerous streptococcal antigens occurs. When an infection enters the body, antistreptococcal antibodies are produced and immune complexes are formed (streptococcus antigens + antibodies to them + complement), which circulate in the blood and settle in the microcirculatory bed. Streptococcus toxins and enzymes also have a damaging effect on the myocardium and connective tissue. Due to a genetically determined defect in the immune system, streptococcal antigens and immune complexes are not completely and quickly eliminated from the body of patients. As a result, autoimmune processes develop according to the type of delayed-type hypersensitivity, and lymphocytes reacting with cardiac tissue are found in the blood of patients. These cells are of great importance in the origin of organ lesions (mainly the heart). In the connective tissue with rheumatism, phase changes occur: mucoid swelling - fibrinoid changes - fibrinoid necrosis. The morphological expression of immune disorders are cellular reactions - infiltration by lymphocytes and plasmocytes, the formation of rheumatic, or Ashofftalalaevskaya, granuloma. The pathological process ends with sclerosis. When the heart is affected, the inflammatory process can spread to all the membranes of the heart (pancarditis) or in isolation to each of the membranes. 2. Clinical picture of rheumatism All manifestations of the disease can be divided into cardiac and extracardiac. It is possible to describe the clinical picture of the disease from these positions. Stage I: the connection of the disease with the transferred infection is revealed. In typical cases, 1-2 weeks after a sore throat or acute respiratory illness, body temperature rises, sometimes up to 38-4 ° C, with fluctuations during the day within 1-2 C and strong sweat (usually without chills). The most common manifestation of rheumatism is heart damage - rheumatic heart disease: simultaneous damage to the myocardium and endocardium. Patients complain of mild pain or discomfort in the region of the heart, slight shortness of breath during exercise, interruptions or palpitations are much less common. Rheumocarditis in young patients, as a rule, is severe: from the very beginning of the disease, severe shortness of breath during exercise and at rest, constant pain in the heart, and palpitations are noted. Pericarditis, as well as extracardiac manifestations of rheumatism, is rare. With the development of dry pericarditis, patients note only constant pain in the region of the heart. With exudative pericarditis, characterized by the accumulation of serous-fibrinous exudate in the heart sac, the pain disappears, as the inflamed pericardial layers are separated by the accumulating exudate. The most characteristic of rheumatism is the defeat of the musculoskeletal system in the form of rheumatic polyarthritis. Rheumatic lesions of the kidneys are also extremely rare, detected only in the study of urine. Abdominal syndrome (peritonitis) occurs almost exclusively in children and adolescents with acute primary rheumatism. At stage II of the diagnostic search, the detection of signs of heart damage is of little importance. In primary rheumatic heart disease, the heart is usually not enlarged. Auscultation reveals a muffled I tone, sometimes the appearance of a III tone, a soft systolic murmur at the apex. This symptomatology is due to changes in the myocardium. In case of damage to the aortic valve, a proto-diastolic murmur at the Botkin point may be heard, and the sonority of the II tone may be preserved. In patients with polyarthritis, joint deformity is noted due to inflammation of the synovial membrane and periarticular tissues, pain on palpation of the joint. Ring-shaped erythema (a sign that is almost pathognomonic for rheumatism) is extremely rare (in 1-2% of patients). At the III stage of the diagnostic search, the data of laboratory and instrumental studies allow us to establish the activity of the pathological process and clarify the damage to the heart and other organs. Acute-phase indicators: neutrophilia with a shift of the leukocyte blood count to the left; an increase in the content of 2-globulins, followed by an increase in the level of globulins; increased fibrinogen content; the appearance of C-reactive protein; ESR increases. Immunological parameters, increased titers of antistreptococcal antibodies (antihyaluronidase and antistreptokinase more than 1:300, anti-O-streptolysin more than 1:250). 3. Diagnosis of rheumatism With the gradual onset of rheumatism, the syndromic diagnosis proposed by AI Nesterov in 1973 (see Table 1) matters: clinical and epidemiological syndrome; cardiovascular syndrome (see Table 2). Table 1
Table 2
4. Differential diagnosis of rheumatism Rheumatic polyarthritis must be differentiated from non-rheumatic ones (see table). Table
5. Treatment of rheumatism The whole complex of treatment of rheumatism consists of antimicrobial and anti-inflammatory therapy, measures that are aimed at restoring immunological homeostasis. It is recommended to use a rational balanced diet, focus on adaptation to physical activity, preparation for work, timely surgical treatment of patients with complex heart defects. All patients during the active phase of rheumatism are shown penicillin (1-200 IU for 000 doses per day, every 1 hours), which has a bactericidal effect on all types of A-streptococcus. The course of treatment is 500 weeks during the active phase of rheumatism, in the future, a transfer to the prolonged drug bicillin-000 (6 units) is required. With intolerance to penicillin, erythromycin 4 mg 2 times a day can be prescribed. Drugs with anti-inflammatory effect, which are used in the modern treatment of the active phase of rheumatism, are glucocorticosteroids, salicylic, indole derivatives, derivatives of phenylacetic acid, etc. Prednisolone is used at 20-30 mg per day (for 2 weeks, then the dose is reduced by 2,5-5 mg every 5-7 days, for a total of 1,5-2 months) for primary and recurrent with III and II degree activity of the process of rheumatic heart disease, with polyserositis and chorea, with the development of heart failure due to active carditis. Corticoid agents affect water-salt metabolism, therefore, potassium chloride 3-4 g / day, panangin and others should be used in the treatment, with fluid retention - aldosterone antagonists (veroshpiron up to 6-8 tablets per day), diuretics (lasix 40 -80 mg / day, furosemide 40-80 mg / day, etc.), with euphoria - tranquilizers, etc. Non-steroidal anti-inflammatory drugs are also widely used for rheumatism: average doses of acetylsalicylic acid are 3-4 g per day, less often 5 g per day or more. Acetylsalicylic acid is used 1 g 3-4 times a day after meals for 1-3 months or more with normal tolerance and subject to control of side effects. The successful use of indolacetic acid derivative - indomethacin in rheumatism for more than 20 years. It has a pronounced therapeutic effect: subjective symptoms of carditis (cardialgia, palpitations, shortness of breath) disappear by the 8-10th day of therapy, and objective signs - by the 14-16th day. The disappearance of polyarthritis and polyserositis occurs even faster. In the treatment of rheumatism, a combination of three main stages is important: hospital - clinic - resort. At stage I, treatment is carried out with the drugs listed above. After reducing the activity of rheumatism and normalizing the patient's condition, they are transferred to stage II - treatment in a rheumatological sanatorium. The main goal of this stage is to continue treatment with non-steroidal anti-inflammatory drugs. Stage III includes dispensary observation and preventive treatment. 6. Classification of cardiomyopathies. Etiology of Dilated Cardiomyopathy (DCM) Cardiomyopathies are primary isolated myocardial lesions of a non-inflammatory nature of unknown etiology (idiopathic), they are not associated with valvular defects or intracardiac shunts, arterial or pulmonary hypertension, coronary heart disease or systemic diseases (such as collagenoses, amyloidosis, hemochromatosis, etc.), moreover, in the final stage of the disease, severe congestive heart failure and complex violations of the heart rhythm and patency develop. The classification of cardiomyopathies is as follows: 1) dilated cardiomyopathy: a) idiopathic; b) toxic; c) infectious; d) with collagenoses; 2) hypertrophic; 3) restrictive; 4) arrhythmic dysplasia of the right ventricle; 5) a combination of one of the 4 types of cardiomyopathies with arterial hypertension. Dilated cardiomyopathy (DCM) is a disease of the heart muscle characterized by a diffuse expansion of all chambers of the heart (mainly the left ventricle), in which the pathology of the pumping function of the heart is in the foreground and, as a result, chronic heart failure (hence the second name is congestive, when the heart is not able to fully pump blood and it "stagnates" in the tissues and organs of the body). The muscular wall of the heart remains either unchanged or hypertrophied to varying degrees. Diseases and factors that preceded the development of DCMP are described in the table below (see table). Table. Diseases and factors that preceded the development of DCM
This is the most common form of damage to the heart muscle. The incidence is 5-8 cases per 100 people per year. There is no clear family history for these patients. Men get sick 000-2 times more often than women. 7. Pathogenesis of dilated cardiomyopathy (DCM) Pathogenesis. As a result of the inflammatory process in the heart muscle (myocarditis), individual cells die in its various parts. Inflammation in this case is viral in nature, and the cells affected by the virus become foreign agents for the body. Accordingly, when antigens appear in the body, a complex of immune response reactions develops, aimed at their destruction. Gradually, the dead muscle cells are replaced by connective tissue, which does not have the ability to extensibility and contractility inherent in the myocardium. As a result of the loss of the main functions of the myocardium, the heart loses its ability to function as a pump. In response to this (as a compensatory reaction), the chambers of the heart expand (i.e., they dilate), and thickening and thickening occurs in the remaining part of the myocardium (i.e., its hypertrophy develops). To increase the delivery of oxygen to the organs and tissues of the body, a persistent increase in heart rate (sinus tachycardia) occurs. This compensatory response only temporarily improves the pumping function of the heart. However, the possibilities of myocardial dilatation and hypertrophy are limited by the amount of viable myocardium and are individual for each specific case of the disease. With the transition of the process to the stage of decompensation, chronic heart failure develops. However, at this stage, another compensatory mechanism comes into play: the tissues of the body increase the extraction of oxygen from the blood compared to a healthy body. But this mechanism is insufficient, since a decrease in the pumping function of the heart leads to a decrease in the supply of oxygen to organs and tissues, which is necessary for their normal functioning, while the amount of carbon dioxide in them increases. In 2/3 of patients in the cavities of the ventricles in the late stages of the disease, parietal thrombi form (due to a decrease in the pumping function of the heart, as well as uneven contraction of the myocardium in the chambers of the heart), followed by the development of embolism in the pulmonary or systemic circulation. Pathohistological and pathomorphological changes in the heart. The shape of the heart becomes spherical, its mass increases from 500 to 1000 g, mainly due to the left ventricle. The myocardium becomes flabby, dull, with noticeable whitish layers of connective tissue, there is a characteristic alternation of hypertrophied and atrophic cardiomyocytes. Microscopically, diffuse fibrosis is detected, it can be combined with both atrophy and hypertrophy of cardiomyocytes, in which there is a significant increase in the volume of nuclei, the number of mitochondria, hyperplasia of the Golgi apparatus, an increase in the number of myofibrils, free and associated with the endoplasmic reticulum ribosomes, an abundance of glycogen granules. 8. Clinical picture and diagnosis of dilated cardiomyopathy (DCM) There are no specific signs of the disease. The clinical picture is polymorphic and is determined by: 1) symptoms of heart failure; 2) rhythm and conduction disturbances; 3) thromboembolic syndrome. In most cases, the prognosis of the disease is determined by the defeat of the left ventricle of the heart. Before the onset of heart failure, DCM is latent. The most frequent complaints of already onset heart failure are complaints of decreased performance, increased fatigue, shortness of breath during exertion, and then at rest. At night, he has a dry cough (the equivalent of cardiac asthma), later - typical asthma attacks. Patients present with characteristic anginal pain. With the development of congestion in the systemic circulation, heaviness appears in the right hypochondrium (due to an enlarged liver), swelling of the legs. Diagnostics. When diagnosing the disease, an important sign is a significant increase in the heart (there are no signs of valvular heart disease or arterial hypertension). Cardiomegaly is manifested by the expansion of the heart in both directions, determined by percussion, as well as the displacement of the apex beat to the left and down. In severe cases, a gallop rhythm, tachycardia, murmurs of relative insufficiency of the mitral or tricuspid valves are heard. In 20% of cases, atrial fibrillation develops. Blood pressure is usually normal or slightly elevated (due to heart failure). Biochemical studies of blood and urine can detect various toxic substances, as well as vitamin deficiencies. Instrumental research methods make it possible to detect: 1) signs of cardiomegaly; 2) changes in indicators of central hemodynamics; 3) rhythm and conduction disturbances. Phonocardiogram confirms auscultatory data in the form of a gallop rhythm, a fairly common detection of systolic murmur. X-ray reveals a significant increase in the ventricles and stagnation of blood in the pulmonary (small) circulation. Echocardiography helps to detect dilatation of both ventricles, hypokinesia of the posterior wall of the left ventricle, paradoxical movement of the interventricular septum during systole. A radioisotope study of the heart (myocardial scintigraphy) is performed to clarify the state of the pumping function of the heart, as well as to determine the zones of the dead myocardium. Angiocardiographically, the same changes are detected as on the echocardiogram. Live myocardial biopsy is not informative for determining the etiology of cardiomyopathy. In some cases, a viral antigen or an increase in the content of LDH, as well as a decrease in energy production by mitochondria, can be detected in the biopsy. 9. Differential / diagnosis of dilated cardiomyopathy (DCM) It is produced primarily with myocarditis and myocardial dystrophies, i.e. with those conditions that are sometimes unreasonably called secondary cardiomyopathies. Myocardial biopsy provides significant assistance in the differential diagnosis of dilated cardiomyopathy and heart disease, occurring with a pronounced increase in it: 1) with severe diffuse myocarditis, cellular infiltration of the stroma is found in combination with dystrophic and necrotic changes in cardiomyocytes; 2) with primary amyloidosis occurring with heart damage (the so-called cardiopathic variant of primary amyloidosis), there is a significant deposition of amyloid in the interstitial tissue of the myocardium, combined with atrophy of muscle fibers; 3) with hemochromatosis (a disease caused by a violation of iron metabolism), deposits of iron-containing pigment are found in the myocardium, various degrees of dystrophy and atrophy of muscle fibers, and proliferation of connective tissue are observed. As a variant of DCM, drug-induced and toxic cardiomyopathies can be considered. Numerous agents can cause toxic damage to the myocardium: ethanol, emetine, lithium, cadmium, cobalt, arsenic, isproterenol and other poisons. Pathohistological changes in the tissues of the heart muscle manifest themselves in the form of focal dystrophies. The most striking example of toxic cardiomyopathy is the cardiomyopathy that occurs in people who drink excessive amounts of beer. In the acute stage of cobalt cardiomyopathy, the presence of hydropic and fatty degeneration, destruction of intracellular organelles, and focal necrosis of cardiomyocytes are noted. Alcoholic cardiomyopathy. Ethanol has a direct toxic effect on cardiomyocytes. Macroscopically, the myocardium is flabby, clay-like, sometimes small scars are observed. The coronary arteries are intact. Microscopic examination shows a combination of dystrophy (hydropic and fatty), atrophy and hypertrophy of cardiomyocytes, possibly the presence of foci of cardiomyocyte lysis and sclerosis. The affected areas of the myocardium contrast with unchanged ones. Electron microscopic examination of heart biopsy specimens shows cystic expansion of the sarcoplasmic reticulum and T-system of cardiomyocytes, which is characteristic of alcoholic cardiomyopathy. Complications of alcoholic cardiomyopathy - sudden death as a result of ventricular fibrillation or chronic heart failure, thromboembolic syndrome. 10. Treatment and prevention of dilated cardiomyopathy (DCM) The general principles for the treatment of DCM do not differ significantly from the treatment of chronic heart failure. In cases of secondary DCM, the treatment of the previous disease (valvular heart disease, etc.) is additionally carried out, and all measures are taken to eliminate the causes of DCM. Peripheral vasodilators are quite effective, especially with concomitant anginal syndrome (nitrong, sustak, nitrosorbide). With anginal syndrome, it becomes necessary to use antianginal drugs, preferably prolonged nitrates (sustak, nitrong, nitrosorbide). Adrenoblockers are effective (they are prescribed in the absence of signs of heart failure). Of the modern methods of surgical treatment of DCMP, the most effective is heart transplantation (transplantation). However, the possibilities of carrying out this operation are significantly limited. For this reason, as an alternative to heart transplantation in modern treatment, to increase the life expectancy of patients with DCMP, reconstructive surgeries have been developed and are being performed, which are aimed at eliminating insufficiency of the mitral and tricuspid heart valves. An alternative to heart transplantation in patients with DCM is partial removal of the left ventricle in order to reduce its size (Baptiste operation). Not so long ago, for the treatment of patients with DCMP, special models of pacemakers were developed, they allow you to make the work of the ventricles of the heart synchronous. This leads to an improvement in the filling of the ventricles of the heart with blood and an increase in the pumping function of the heart. DCM in children is 5-10 cases per 100 children per year. The greatest effect in the treatment of dilated cardiomyopathy in young children is achieved with a combination of corticosteroids and glycosides (prednisolone and digoxin). Against the background of monotherapy with prednisolone, a decrease in heart rate occurs. Monotherapy with digoxin leads to a decrease in tachycardia and dyspnea. Given the inadvisability of prescribing cytostatic drugs in young children, since a significant number of treatment complications were observed, it is more optimal in pediatrics to use long-acting cardiac glycosides in combination with corticosteroid hormones in dilated cardiomyopathy. Prevention. Prevention of DCMP consists in the exclusion of alcohol, cocaine, as well as careful monitoring of cardiac performance during tumor chemotherapy. It is useful to harden the body from an early age. Complete abstinence from alcohol in alcoholic DCM improves heart contractility and may eliminate the need for a heart transplant. 11. Classification of cardiomyopathies. Etiology of hypertrophic cardiomyopathy (HCM) Hypertrophic cardiomyopathy (HCM) is a non-coronary disease of the ventricular myocardium (mainly the left), characterized by massive hypertrophy of their walls with protrusion of the interventricular septum (IVS) into the cavity of the right ventricle, which can be significantly thickened, a decrease in the internal volume of the ventricles, normal or increased contractility of the ventricular myocardium and impaired relaxation (diastolic dysfunction). The most common is isolated hypertrophy of the interventricular septum (isolated hypertrophic subaortic stenosis - IHSS) or the apical part of the ventricles. Classification. Classification of HCM by localization of hypertrophy (ED Wigle et al., 1985 with additions). I. LV hypertrophy. 1. Asymmetric hypertrophy, in which myocardial hypertrophy of individual walls or segments of the ventricles occurs (including IVS hypertrophy - 90% with or without left ventricular outflow tract obstruction, midventricular hypertrophy - 1%, apical left ventricular hypertrophy - 3%, free wall hypertrophy left ventricle and posterior part of the IVS - 1%). 2. Symmetrical (concentric) hypertrophy of the left ventricle, when myocardial hypertrophy extends to all walls of the ventricles, occurs in 5% of cases. II. Hypertrophy of the pancreas. In the case when myocardial hypertrophy prevents the normal outflow of blood from the ventricles of the heart, they speak of an obstructive form of HCM. In other cases, HCM is non-obstructive. Etiology. The disease can be either congenital or acquired. Congenital HCM is inherited in an autosomal dominant fashion. Within the same family, various forms and variants of HCM can be observed. Most often, asymmetric hypertrophy of the interventricular septum is inherited. The acquired form of HCM occurs in elderly patients with a history of arterial hypertension. The prevalence is 0,02-0,05%. The reasons for the development of acquired HCM are not fully understood. According to one of the proposed hypotheses, individuals with acquired HCM in the prenatal period develop a defect in the adrenergic receptors of the heart involved in the regulation of cardiac activity, in particular heart rate. As a result, the sensitivity to norepinephrine and similar hormones, which increase the heart rate, is significantly increased, which affects the development of myocardial hypertrophy in them, and eventually HCM. pathological picture. Disoriented, irregular, chaotic arrangement of cardiomyocytes and myofibrils in cardiomyocytes, myocardial fibrosis is a violation of the architectonics of the heart muscle. 12. Clinical picture and diagnosis of hypertrophic cardiomyopathy (HCM) clinical picture. HCM is characterized by an extreme variety of symptoms, which is the cause of erroneous diagnosis. The presence and timing of the appearance of complaints in HCM are mainly determined by 2 factors: the form of HCM and the localization of the lesion. The most powerful chamber of the heart is the left ventricle, therefore, with hypertrophy of the myocardium of its walls, complaints may not appear for a long time. The isolated defeat of a right ventricle of heart meets extremely seldom. The clinical picture of HCM is: 1) signs of ventricular myocardial hypertrophy (mainly left); 2) a sign of insufficient diastolic ventricular function; 3) variable signs of left ventricular outflow tract obstruction. Diagnostics. In the process of diagnostic search, the most significant is the detection of systolic murmur, altered pulse and displaced apex beat. For the diagnosis of HCM, echocardiography data are of the greatest importance, allowing to clarify the anatomical features of the disease, the severity of myocardial hypertrophy, obstruction of the outflow tract of the left ventricle. The following signs are revealed: asymmetric hypertrophy of the IVS, more pronounced in the upper third, its hypokinesis; systolic movement of the anterior leaflet of the mitral valve in the anterior direction; contact of the anterior leaflet of the mitral valve with the IVS in diastole. Nonspecific signs are: hypertrophy of the left atrium, hypertrophy of the posterior wall of the left ventricle, a decrease in the average speed of the diastolic cover of the anterior leaflet of the mitral valve. On the ECG, any specific changes are found only with sufficiently developed left ventricular hypertrophy. X-ray diagnostics is important only in the advanced stage of the disease, when an increase in the left ventricle and left atrium, an expansion of the descending part of the aorta can be determined. On the phonocardiogram, the amplitudes of I and II tones are preserved, which is a differential sign of HCM from stenosis of the aortic orifice, and systolic murmur of varying severity is also detected. Invasive research methods (probing of the left parts of the heart, contrast angiography) are currently not mandatory, since echocardiography provides quite reliable information for making a diagnosis. Cardiac probing is used under X-ray television control. Technique for performing the method: by puncturing a large artery under local anesthesia with the further introduction of a special catheter into the heart cavity, the pressure gradient (difference) between the left ventricle and the aorta departing from it is measured. Normally, this gradient should not be. 13. Treatment and prevention of hypertrophic cardiomyopathy (HCM) Treatment. The basis of drug treatment of HCM is drugs that improve the blood supply to the ventricles of the heart in diastole. These drugs are a group of b-blockers (anaprilin, atenolol, metoprolol and propranolol, 160-320 mg / day, etc.) and a group of calcium ion antagonists (verapamil, but with caution). Novokinamide disopyramide also reduces heart rate and has an antiarrhythmic effect. At the very beginning of treatment, small doses of these drugs are used, then there is a gradual increase in dosage to the maximum tolerated by the patient. β-blockers are used with caution in diabetes mellitus, bronchial asthma and some other diseases. When treating with these drugs, constant monitoring of blood pressure and pulse rate is necessary. A decrease in pressure below 90/60 mm Hg is dangerous. Art. and heart rate below 55 per minute. If a patient has dangerous rhythm disturbances that cannot be treated with b-blockers or calcium ion antagonists, then other antiarrhythmic drugs are additionally used in the treatment of such patients. The appointment of anticoagulants is recommended for paroxysmal arrhythmias and atrial fibrillation, as well as in the presence of blood clots in the heart chambers (warfarin, etc.). During the period of treatment with these drugs, it is necessary to regularly monitor a number of indicators of the blood coagulation system. With a significant overdose of anticoagulants, external (nasal, uterine, etc.) and internal bleeding (hematomas, etc.) are possible. Surgical treatment is performed in patients with obstructive HCM when medical treatment is not effective or when the gradient between the left ventricle and aorta is more than 30 mm Hg. Art. (the operation of myotomy or myectomy is performed - excision or removal of a part of the hypertrophied myocardium of the left ventricle). Mitral valve replacement and non-surgical IVS ablation are also performed. Prevention. All patients with HCM, especially those with an obstructive form, are contraindicated in sports in which a pronounced increase in physical activity is possible in a short period of time (athletics, football, hockey). Prevention of the disease consists in early diagnosis, which makes it possible to begin early treatment of the disease and prevent the development of severe myocardial hypertrophy. An echocardiogram should be performed in the genetic relatives of the patient. Screening ECG and EchoCG, which are carried out during the annual medical examination, are also important for diagnosis. In patients with obstructive HCM, prophylaxis of infective endocarditis (antibiotic prophylaxis, etc.) should be carried out, since the presence of obstruction creates the conditions for the development of this life-threatening condition. 14. Causes of restrictive cardiomyopathy (RCMP) Restrictive cardiomyopathy (RCMP) - (from the Latin word restrictio - "restriction") - a group of diseases of the myocardium and endocardium, in which, as a result of pronounced fibrosis and loss of elasticity due to various reasons, there is a fixed limitation of filling the ventricles in diastole. RCMP includes: Lefler's parietal fibroplastic endocarditis (found in countries with a temperate climate, described by W. Loffler et al., 1936) and endomyocardial fibrosis (found in countries of tropical Africa, described by D. Bedford et E. Konstman). Causes of RCM. Primary RCM is very rare, and the only proven cause of its occurrence is the so-called hypereosinophilic syndrome (Leffler's disease, Leffler's parietal fibroplastic endocarditis). It occurs mainly in men aged 30-40 years. With hypereosinophilic syndrome, inflammation of the endocardium occurs, which over time culminates in significant compaction of the endocardium and its rough adhesion to the adjacent myocardium, which leads to a sharp decrease in the extensibility of the heart muscle. Lefler's syndrome is also characterized by persistent eosinophilia for 6 months or more (1500 eosinophils per 1 mm3), damage to internal organs (liver, kidneys, lungs, bone marrow). In the vast majority of cases, the origin of RCMP is secondary, due to other reasons, among which the most common are: 1) amyloidosis - a disease associated with a violation of protein metabolism in the body; at the same time, in the tissues of various organs, an abnormal protein (amyloid) is formed and deposited in large quantities; when the heart is damaged, amyloid causes a decrease in its contractility and extensibility; 2) hemochromatosis - a violation of iron metabolism in the body, accompanied by an increased content of iron in the blood, its excess is deposited in many organs and tissues, including the myocardium, thereby causing a decrease in its extensibility; 3) sarcoidosis - a disease of unknown etiology, characterized by the formation of cell clusters (granulomas) in organs and tissues; the lungs, liver, lymph nodes and spleen are most often affected; and developing granulomas in the myocardium lead to a decrease in its extensibility; 4) endocardial diseases (endocardial fibrosis, endocardial fibroelastosis, etc.), when there is a significant thickening and compaction of the endocardium, which also leads to a sharp limitation of myocardial extensibility. Fibroelastosis of the endocardium, in particular, can only occur in infants; this disease is not compatible with life due to the early development of severe heart failure. 15. Clinical picture and diagnosis of restrictive cardiomyopathy (RCMP) clinical picture. The manifestations of the disease are extremely polymorphic and are determined by the symptoms of circulatory disorders in the small or large circle (depending on the primary lesion of the right or left ventricles). Complaints may be absent or may be due to congestion in the pulmonary or systemic circulation. Patients usually complain of shortness of breath, which first appears during exercise, and as the disease progresses, shortness of breath is observed at rest. Due to a decrease in the pumping function of the heart, the patient complains of fatigue and poor tolerance to any load. Over time, swelling of the legs, an enlarged liver and dropsy of the abdomen join. Periodically, an irregular heartbeat appears, and with the development of persistent blockades, there may be fainting. The first stage of the development of the disease (necrotic) is characterized by the appearance of fever, weight loss, cough, skin rash and tachycardia. Diagnostics. Recognition of RCM is extremely difficult. It is possible to speak with confidence about this pathology only after the exclusion of a number of similarly occurring diseases (such as idiopathic myocarditis of the Abramov-Fiedler type, exudative pericarditis, valvular heart disease). When examining patients with RCMP, symptoms characteristic of congestive heart failure (edema, hepatomegaly and ascites), as well as pronounced pulsation of the neck veins, are found. During auscultation, the detection of an enlarged heart, a soft late systolic murmur and a loud early III tone is of great importance. An ECG study reveals moderate hypertrophy of the ventricular myocardium, as well as various disturbances in the rhythm and conduction of the heart impulse, and nonspecific changes in the T wave on the ECG. Echocardiography is one of the most informative methods for diagnosing the disease, with its help, thickening of the endocardium, a change in the nature of the filling of the ventricles of the heart, a decrease in the pumping function of the heart, a rapid movement of the anterior leaflet of the mitral valve during diastole and a rapid early movement of the posterior wall of the left ventricle outward are detected. Magnetic resonance imaging allows you to obtain information about the anatomy of the heart, determine pathological inclusions in the myocardium and measure the thickness of the endocardium. When examining the parameters of central hemodynamics, an increased filling pressure in both ventricles is determined, and the final pressure in the left exceeds that in the right ventricle. Ventriculography reveals increased contraction of the left ventricle, smooth contours of its walls, sometimes with a filling defect in the apex (evidence of obliteration). There are signs of valvular insufficiency, in particular the mitral or tricuspid valve. 16. Differential diagnosis, treatment and prevention of restrictive cardiomyopathy (RCMP) Differential diagnosis. In the differential diagnosis of RCMP, it is very important to take into account the similarity of the disease in external manifestations with constrictive pericarditis, but the treatment method for these diseases is diametrically opposed. Live biopsy of the myocardium and endocardium is usually used simultaneously with cardiac probing, which allows you to have more information to clarify the nature of the disease and further treatment. In extremely rare cases, when the above diagnostic methods do not allow distinguishing RCMP from constrictive pericarditis, a direct revision of the pericardium is performed on the operating table. All patients with RCMP need a comprehensive clinical, biochemical and additional examination to determine non-cardiac causes of the disease. Treatment. Treatment of the disease presents significant difficulties. Most drugs that are used to treat heart failure may not bring the desired results due to the fact that, due to the characteristics of the disease, it is impossible to obtain a significant improvement in myocardial compliance (in some cases, calcium ion antagonists are prescribed for this purpose). Diuretics (aldactone) are used to eliminate excess fluid in the body. To eliminate persistent conduction disorders, it may be necessary to set up (implant) a permanent pacemaker. This is caused by diseases such as sarcoidosis and hemochromatosis, leading to the development of secondary RCMP, they are subject to self-treatment. In the treatment of sarcoidosis, hormonal drugs (prednisolone, etc.) are used, and in hemochromatosis, regular bloodletting (to reduce the concentration of iron in the body). Treatment of myocardial amyloidosis is directly dependent on the causes of its occurrence. It is advisable to use anticoagulant drugs for thrombosis in the chambers of the heart. Surgical treatment is resorted to in cases of RCMP caused by endocardial damage. During the operation, if possible, the part of the endocardium that has undergone changes is excised. In some cases, if there is insufficiency of the atrioventricular valves, their prosthesis is performed. Some forms of amyloid myocardial damage are treated with a heart transplant. Prevention of RCM. Unfortunately, preventive measures for this disease are limited. Most importantly, early detection of potentially removable causes of amyloidosis, sarcoidosis, hemochromatosis, etc. is necessary. To achieve these goals, it is of great importance to conduct an annual medical examination of the population. 17. Etiology of infective endocarditis (IE) Infective endocarditis (IE) is a disease consisting in a polyposis-ulcerative lesion of the valvular apparatus of the heart (often with the development of valvular insufficiency) or parietal endocardium (less often, the endothelium of the aorta or the nearest large artery is affected). The disease is caused by various pathogenic microorganisms and is accompanied by a systemic lesion of the internal organs (kidneys, liver, spleen) against the background of an altered reactivity of the organism. Etiology. The pathogenic causative agents of the disease are most often the coccal group of microorganisms - streptococci (viridans streptococcus was previously isolated in 90% of cases), staphylococci (golden, white), enterococcus, pneumococcus. In recent years, due to the widespread use of antibiotics, the range of microbial pathogens has changed. The disease can be caused by gram-negative flora (Escherichia coli, Pseudomonas aeruginosa, Proteus, Klebsiella); evidence has emerged of the important role of pathogenic fungi, Sarcinus, Brucella and viruses. Diseases caused by these pathogens are more severe, especially endocarditis caused by a fungal infection (usually occurs due to irrational use of antibiotics). However, in some patients the true causative agent of the disease is not detected (negative blood culture rate 20-50%). Often, infection occurs at the site of a prosthetic valve - the so-called prosthetic IE, which develops mainly within 2 months after heart valve replacement surgery. In this case, the causative agent of the disease most often has a streptococcal nature. Thus, the sources of infection and bacteremia in IE are very diverse (oral surgery, surgery and diagnostic procedures in the urogenital area, surgery on the cardiovascular system (including valve replacement), prolonged stay of the catheter in a vein, frequent intravenous infusions and endoscopic methods studies, chronic hemodialysis (arteriovenous shunt), intravenous drug administration). There are so-called primary IE, which developed on intact valves, as well as IE against the background of congenital and acquired changes in the heart and its valvular apparatus - secondary endocarditis. These changes make it possible to distinguish patients into separate risk groups: heart defects (congenital and acquired), mitral valve prolapse, arteriovenous aneurysms, post-infarction aneurysms, shunts, condition after surgery on the heart and large vessels. 18. Pathogenesis and classification of infective endocarditis (IE) Pathogenesis. The mechanism of development of IE is complex and not well understood. In the development of the disease, 3 stages can be distinguished. Stage I (infectious-toxic) proceeds with varying degrees of severity of intoxication. There is a growth of bacteria, the destruction of valves, leading to the development of heart disease; at the same stage, a generalization of the process often occurs due to the hematogenous spread of infection - pieces of cusps or colonies of microorganisms can separate from the valve, the cusps can rupture. Stage II - immuno-inflammatory, in which microorganisms fixed on the valves cause prolonged autosensitization and hyperergic damage to the organs and tissues of the body (immune generalization of the process). Stage III - dystrophic - occurs with the progression of the pathological process: the functions of a number of organs are disturbed, heart and kidney failure occurs, further aggravating the course of the disease (see table). Table Classification of IE
A distinction is also made between active and inactive (healed) IE. There is also a surgical classification, in which they distinguish: 1) the lesion is limited to the valve leaflets; 2) the lesion extends beyond the valve. Acute IE (rapidly progressive, develops over 8-10 weeks) is rare, usually in individuals who have not previously had heart disease, and is clinically manifested by a picture of general sepsis. Subacute IE (most common) lasts 3-4 months, with adequate drug therapy, remission may occur. Protracted IE lasts for many months with periods of exacerbation and remission, it is characterized by mild clinical manifestations. With an unfavorable course, severe complications arise, and patients die from progressive heart failure, increasing septic intoxication. 19. Clinical picture and diagnosis of infective endocarditis (IE) clinical picture. The manifestations of IE are presented as syndromes. 1. Syndrome of inflammatory changes and septicemia. 2. Syndrome of general intoxication of the body. 3. Syndrome of valve damage. 4. Syndrome of "laboratory" immune disorders. 5. Syndrome of thromboembolic complications. 6. Syndrome of generalization of lesions. Diagnosis of IE is based primarily on early detection of the causative agent of the disease. For this purpose, the following laboratory and instrumental studies are used. 1. Obtaining a positive blood culture. 2. Carrying out NBT (nitrobluetetrazolium test). 3. A clinical blood test to detect acute phase indicators: an increase in ESR to 50 mm / h or more, leukocytosis with a shift of the leukocyte formula to the left or (in stage II) leukopenia and hypochromic anemia can be detected. 4. Identification of immunological changes. 5. Urinalysis is performed to clarify the lesions of various organs and systems, when glomerulonephritis is detected, manifested by proteinuria, cylindruria and hematuria. 6. A direct diagnostic sign of IE - the presence of vegetation on the heart valves - is detected by echocardiography. Thus, from the whole variety of symptoms, the main and additional ones should be distinguished. The main criteria for the diagnosis of IE: 1) fever with a temperature above 38 °C with chills; 2) Lukin spots; 3) Osler's nodules; 4) endocarditis on unchanged valves (primary) or against the background of rheumatic and congenital heart defects. infectious myocarditis; 5) multiple arterial thromboembolism, ruptures of mycotic aneurysms with hemorrhages; 6) splenomegaly; 7) positive blood culture; 8) a pronounced positive effect from the use of antibiotics. Additional criteria for the diagnosis of IE: 1) increased body temperature to 38 °C, chilling; 2) hemorrhages on the skin; 3) rapid weight loss; 4) asymmetric arthritis of small joints of hands, feet; 5) anemization; 6) ESR over 40 mm/h; 7) sharply positive SRV; 8) the presence of rheumatoid factor; 9) a-globulins above 25%; 10) increase in the content of immunoglobulins M, E and A. 20. Treatment and prevention of infective endocarditis (IE) Treatment. Treatment of IE should be as early and etiotropic as possible, taking into account bacteriological data. A combination of conservative and surgical treatment is advisable. For the treatment of IE in all age groups, antibiotics are primarily used, which have a bactericidal effect on microorganisms. The drug of first choice is still penicillin. The daily dose - up to 20 IU is administered intravenously and intramuscularly. However, one should not exclude the fact that in patients of elderly and senile age, when treated with penicillin and other antibiotics in high doses, a cardiotoxic effect is often observed. With an unknown etiology, treatment begins with high doses of benzylpenicillin intramuscularly or intravenously up to 18-000 units or more, a combination with streptomycin up to 000 g / m per day or aminoglycosides (gentamicin, tobramycin at a rate of 20-000 mg / day) is used. kg per day). Cephalosporins are also basic drugs used for the treatment of IE: the most commonly used are claforan, cefamisin (000-1 g/day, intramuscularly and intravenously), as well as zeporin (4-6 g/day) and kefzol (up to 4-10 g intravenously). and etc.). Fusidin has a good anti-staphylococcal effect, in some cases it is effective in the resistance of microorganisms to other antibiotics (10-16 g / day). Treatment with antibiotics is prescribed for a long time in a course of 1,5-2 months, until the infection is completely eliminated. With reduced immunoreactivity of the body, antibacterial agents are combined with passive immunotherapy using immunomodulators (thymalin, T-activin, etc.). To prevent thrombosis, for example, in case of endocarditis that has developed against the background of angiogenic sepsis, controlled hypocoagulation is created using heparin (20-000 units intravenously or subcutaneously). To inhibit proteolytic enzymes, contrical is used (up to 25-000 units intravenously). When valvular IE contributed to the formation of valvular heart disease or the manifestations of the disease do not disappear despite massive antibiotic therapy, it is advisable to perform surgical treatment. The main goal of the operation is to preserve the patient's own valve. Sometimes they are limited to removing vegetations, suturing ruptures of the valves, etc. If the valve is almost completely destroyed under the influence of infection, it is replaced with an artificial one (prosthesis) using mechanical and biological prostheses. Prevention. Prevention of IE consists in the timely sanitation of chronic foci of infection in the oral cavity, tonsils, nasopharynx, paranasal sinuses, the use of active antibiotic therapy for acute streptococcal and staphylococcal diseases (tonsillitis, etc.). Hardening of the body is recommended. 21. Etiology of bronchial asthma (BA) An exhaustive definition of asthma does not exist to date, however, the most complete definition of this disease was given by G. B. Fedoseev in 1982. Bronchial asthma (BA) is an independent, chronic, recurrent disease with a primary lesion of the respiratory tract, the main and obligatory pathogenetic mechanism of which is altered bronchial reactivity due to specific (immunological) and (or) non-specific, congenital or acquired mechanisms, and the main (mandatory) clinical sign is an asthma attack and (or) asthmatic condition (asthmatic status) due to spasm of bronchial smooth muscles, hypersecretion, dyscrinia and swelling of the bronchial mucosa. Etiology. A combination of several factors plays an important role in the occurrence of asthma. In this regard, there are 2 forms of asthma - atopic (from the Latin athopia - “hereditary predisposition”) and infectious-allergic. Hereditary predisposition is due to the connection of certain histocompatibility antigens (HCA) with the severity of asthma, and an increase in the severity of the disease is especially often observed in carriers of antigens B35 and B40. Internal factors in the development of the disease are biological defects in the immune, endocrine systems, autonomic nervous system, bronchial sensitivity and reactivity, mucociliary clearance, pulmonary vascular endothelium, rapid response system (mast cells, etc.), metabolism of arachidonic acid, etc. External factors include: 1) infectious allergens (viruses, bacteria, fungi, yeast, etc.); 2) non-infectious allergens (pollen, dust, industrial, medicinal, food; allergens of ticks, insects and animals); 3) mechanical and chemical irritants (metal, wood, silicate, cotton dust; vapors of acids, alkalis; fumes, etc.); 4) meteorological and physico-chemical factors (changes in air temperature and humidity, fluctuations in barometric pressure, the Earth's magnetic field, physical effort, etc.); 5) stressful, neuropsychic effects and physical activity. Infectious agents can have not only an allergenic effect, but also reduce the body's sensitivity threshold to non-infectious (atopic) allergens, increase the permeability of the respiratory mucosa for them; to form a change in the reactivity of target cells (mast cells, basophils, monocytes, etc.) and effector systems. 22. Pathogenesis of bronchial asthma (BA) Pathogenesis. Altered bronchial reactivity is the central link in the pathogenesis of the disease and can be primary and secondary. In the first case, the change in reactivity is congenital and acquired. Secondary changes in bronchial reactivity are a manifestation of changes in the reactivity of the immune, endocrine, and nervous systems of the body. Thus, speaking about the pathogenesis of AD, we can distinguish 2 groups of mechanisms: immunological and non-immunological. Type I (atopic, reaginic, or anaphylactic). In response to the ingestion of exoallergen antigens (pollen, animal and vegetable proteins, bacteria and drugs), an increased production (reagins) occurs, which are fixed and accumulated on mast cells (primary effector cells). This is the immunological stage of AD. Following this, the pathochemical stage of the process develops - degranulation of mast cells with the release of vasoactive, bronchospastic and chemotactic substances (histamine, serotonin, various chemotactic factors, etc.). Under the influence of biologically active substances, the pathophysiological stage of pathogenesis begins: the permeability of the microcirculatory bed increases, which leads to the development of edema, serous inflammation, and bronchospasm. Type III reaction (immunocomplex type, or Arthus phenomenon) develops under the influence of exoallergens and endoallergens. The reaction occurs in the zone of excess antigen with the participation of precipitating antibodies belonging to the immunoglobulins of classes O and M. The damaging effect of the formed antigen-antibody complex is realized through complement activation, the release of lysosomal enzymes. There is damage to the basal membranes, spasm of smooth muscles of the bronchi, vasodilation, and the permeability of the microvasculature increases. Type IV (cellular, delayed-type hypersensitivity) is characterized by the fact that sensitized lymphocytes have a damaging effect. In this case, the mediators of the allergic reaction are lymphokines (act on macrophages, epithelial cells), lysosomal enzymes, and an activated kinin system. Under the influence of these substances, edema develops, swelling of the mucous membrane, bronchospasm, hyperproduction of viscous bronchial secretions. Non-immunological mechanisms are the primary change in bronchial reactivity as a result of congenital and acquired biological defects. Non-immunological mechanisms act on primary or secondary effector cells or on the receptors of the smooth muscles of the bronchi, blood vessels, cells of the bronchial glands. This changes the reactivity of target cells and, above all, mast cells, which is accompanied by excessive production of biologically active substances (histamine, leukotrienes, etc.). Recently, there has been talk about the special role of glucocorticoid insufficiency and dysovarian disorders in the pathogenesis of bronchial obstruction disorders. Insufficiency of glucocorticosteroids leads to the development of hyperreactivity of mast cells, decreased synthesis of catecholamines, activation of prostaglandins F2a, as well as disruption of the immunocompetent system. 23. Classification of bronchial asthma (BA) Classification. The predominance of one or another mechanism in the pathogenesis of AD makes it possible to distinguish its various pathogenetic features. Currently, the classification proposed by G. B. Fedoseev (1982) is used. Stages of AD development. I - pre-asthma (conditions that threaten development: acute and chronic bronchitis, acute and chronic pneumonia with elements of bronchospasm in combination with vasomotor rhinitis, urticaria). II - clinically formed BA (considered as such after the first attack or immediately onset of status asthmaticus). BA forms: 1) immunological; 2) non-immunological. Pathogenetic mechanisms (clinical and pathogenetic variants) of AD: 1) atopic; 2) infection-dependent; 3) autoimmune; 4) dishormonal; 5) neuropsychic imbalance; 6) adrenergic imbalance; 7) cholinergic imbalance; 8) primary altered bronchial reactivity. Severity of BA: 1) mild course (exacerbations are rare, 2-3 times a year, short-term asthma attacks are stopped by taking various bronchodilator drugs inside); 2) moderate (more frequent exacerbations 3-4 times a year, asthma attacks are more severe and stopped by injections of drugs); 3) severe course (characterized by frequent and prolonged exacerbations, severe attacks, often turning into an asthmatic state). Phases of asthma progression: 1) exacerbation (the presence of recurrent attacks of asthma or asthmatic condition); 2) subsiding exacerbation (attacks become more rare and mild, physical and functional signs of the disease are less pronounced than in the exacerbation phase); 3) remission (typical manifestations of BA disappear: asthma attacks do not occur; bronchial patency is fully or partially restored). Complications: 1) pulmonary: emphysema, pulmonary insufficiency, atelectasis, pneumothorax, status asthmaticus, etc.; 2) extrapulmonary: cor pulmonale (compensated and decompensated with the development of right heart failure), myocardial dystrophy, etc. 24. Differential diagnosis of bronchial asthma (BA) Differential diagnosis. BA is differentiated from cardiac asthma (see Table 1). Table 1 Differential diagnosis of AD
25. Treatment and prevention of bronchial asthma (BA) Treatment. In the treatment of asthma, a stepwise approach is recommended, (step 1 - the least severity of asthma, step 4 - the greatest). Stage 1: A mild intermittent course in which asthma symptoms appear on exposure to a trigger (eg, pollen or animal hair) or due to exercise. Treatment consists of prophylactic medication if necessary (inhaled drugs are prescribed - agonists, cromoglycate, nedocromil or anticholinergics). If asthma manifests itself with more frequent symptoms, an increase in the need for bronchodilators, then it becomes necessary to move to the next stage. Stage 2. Slight persistent course. Primary therapy includes anti-inflammatory drugs, inhaled corticosteroids, sodium cromoglycate, or nedocromil sodium. For more severe and prolonged exacerbations, a short course of oral corticosteroids is given. Stage 3 is characterized by moderate severity of BA. Such patients require daily intake of prophylactic anti-inflammatory drugs. The dose of inhaled corticosteroids is 800-2000 mcg in combination with long-acting bronchodilators. Stage 4. Severe asthma, when it is not completely controlled. In this case, the goal of treatment is to achieve the best possible results. Primary treatment involves the appointment of inhaled corticosteroids in high doses. A more severe exacerbation may require a course of treatment with oral corticosteroids, which are prescribed in minimal doses or every other day. To prevent the development of side effects, high doses of inhaled corticosteroids are administered through a spacer. Step 5 involves reducing supportive medication. This is possible if the asthma remains under control for at least 3 months, which helps to reduce the risk of side effects and increases the patient's susceptibility to the planned treatment. "Reduction" of treatment is carried out under the constant control of symptoms, clinical manifestations and indicators of respiratory functions by gradually reducing (cancelling) the last dose or additional drugs. Prevention. Primary prevention of asthma includes the treatment of patients in a state of pre-asthma, the detection of biological defects in practically healthy individuals with a burdened heredity that pose a threat to the onset of asthma, the elimination of potentially dangerous allergens, irritants and other factors that can lead to the development of the disease from the patient's environment. In the treatment of patients in a state of preasthma, it is necessary to sanitize the foci of infection, treat allergic rhinosinusopathy, apply various methods of non-drug treatment, including acupuncture and psychotherapy, exercise therapy, barotherapy, spa treatment. Carrying out specific and nonspecific hyposensitization is shown. 26. Etiology and pathogenesis of chronic bronchitis (CB) Chronic obstructive bronchitis is a diffuse non-allergic inflammatory lesion of the bronchial tree, caused by prolonged irritating effects on the bronchi of various agents, which has a progressive course and is characterized by obstructive pulmonary ventilation, mucus formation and the draining function of the bronchial tree, which is manifested by cough, sputum and shortness of breath. Chronic bronchitis is divided into primary and secondary. Primary chronic bronchitis is an independent disease that is not associated with other bronchopulmonary processes or damage to other organs and systems, in which there is a diffuse lesion of the bronchial tree. Secondary HB develops against the background of other diseases - both pulmonary and extrapulmonary. Etiology. In the development of CB play a role as exogenous factors. Obstructive syndrome develops due to a combination of a number of factors: 1) spasm of smooth muscles of the bronchi as a result of irritating effects of exogenous factors and inflammatory changes in the mucous membrane; 2) hypersecretion of mucus, changes in its rheological properties, leading to disruption of mucociliary transport and blockage of the bronchi with a viscous secret; 3) epithelium metaplasia from cylindrical to stratified squamous and its hyperplasia; 4) violations of the production of surfactant; 5) inflammatory edema and mucosal infiltration; 6) collapse of small bronchi and obliteration of bronchioles; 7) allergic changes in the mucous membrane. Various ratios of changes in the mucous membrane cause the formation of a certain clinical form: 1) with catarrhal non-obstructive bronchitis, superficial changes in the structural and functional properties of the mucous membrane prevail; 2) with mucopurulent (purulent) bronchitis, the processes of infectious inflammation predominate. However, a situation is also possible when long-term catarrhal bronchitis due to the addition of an infection can become mucopurulent, etc. In the non-obstructive variant of all clinical forms of chronic bronchitis, ventilation disorders are slightly pronounced; 3) obstructive disorders initially appear only against the background of an exacerbation of the disease and are caused by inflammatory changes in the bronchi, hyper- and dyscrinia, bronchospasm (reversible components of obstruction), but then they persist constantly, while the obstructive syndrome grows slowly. 27. Clinical picture of chronic bronchitis (CB) clinical picture. The main symptoms of HB are cough, sputum production, shortness of breath. With an exacerbation of the disease or due to hypoxia with the development of pulmonary insufficiency and other complications, general symptoms (sweating, weakness, fever, fatigue, etc.) are revealed. Cough is the most typical manifestation of the disease. According to its nature and consistency of sputum, one can assume a variant of the course of the disease. With a non-obstructive variant of catarrhal bronchitis, the cough is accompanied by the release of a small amount of mucous watery sputum (more often in the morning, after exercise or due to increased breathing). At the beginning of the disease, cough does not bother the patient; the appearance of a paroxysmal cough indicates the development of bronchial obstruction. The cough acquires a barking shade and is paroxysmal in nature with a pronounced expiratory collapse of the trachea and large bronchi. With purulent and mucopurulent bronchitis, patients are more concerned about coughing up sputum. In the event of an exacerbation of the disease, sputum acquires a purulent character, its amount increases, sometimes sputum is excreted with difficulty (due to bronchial obstruction during exacerbation). In the obstructive variant of bronchitis, the cough is unproductive and hacking, accompanied by shortness of breath, with a small amount of sputum. Shortness of breath occurs in all patients with chronic bronchitis at various times. The appearance of shortness of breath in "long-term coughing" patients initially with significant physical exertion indicates the addition of bronchial obstruction. As the disease progresses, shortness of breath becomes more pronounced and constant, i.e., respiratory (pulmonary) insufficiency develops. In the non-obstructive variant, CB progresses slowly, shortness of breath usually appears 20-30 years after the onset of the disease. Such patients almost never fix the onset of the disease, but only indicate the appearance of complications or frequent exacerbations. There is a history of hypersensitivity to cold, and most patients report long-term smoking. In a number of patients, the disease is associated with occupational hazards at work. When analyzing a cough history, it is necessary to make sure that the patient has no other pathology of the bronchopulmonary apparatus (tuberculosis, tumors, bronchiectasis, pneumoconiosis, systemic diseases of the connective tissue, etc.), accompanied by the same symptoms. Sometimes a history indicates hemoptysis due to mild vulnerability of the bronchial mucosa. Recurrent hemoptysis indicates a hemorrhagic form of bronchitis. In addition, hemoptysis in chronic, long-term bronchitis may be the first symptom of lung cancer or bronchiectasis. 28. Diagnosis of chronic bronchitis (CB) Diagnostics. Auscultation reveals hard breathing (with the development of emphysema it can become weakened) and dry rales of a diffuse nature, the timbre of which depends on the caliber of the affected bronchi (wheezing wheezes well heard on exhalation are characteristic of lesions of small bronchi). With an exacerbation of obstructive bronchitis, shortness of breath increases, the phenomena of respiratory failure increase. In advanced cases of chronic bronchitis and with the addition of complications, signs of emphysema of the lungs, respiratory and cardiac (right ventricular) insufficiency - decompensated pulmonary heart appear: acrocyanosis, pastosity or swelling of the legs and feet, changes in the nails in the form of watch glasses, and the terminal phalanges of the hands and feet - in in the form of drumsticks, swelling of the cervical veins, pulsation in the epigastric region due to the right ventricle, accent of the II tone in the II intercostal space to the left of the sternum, liver enlargement. Laboratory and instrumental indicators have a different degree of significance depending on the stage of the process. X-ray examination of the chest organs is performed in all patients with chronic bronchitis, however, as a rule, there are no changes in the lungs on plain radiographs. There may be a mesh deformation of the lung pattern, due to the development of pneumosclerosis. X-ray examination plays an important role in the diagnosis of complications (acute pneumonia, bronchiectasis) and in the differential diagnosis with diseases with similar symptoms. Bronchography is used only to diagnose bronchiectasis. Bronchoscopy is of great importance in the diagnosis of chronic bronchitis and its differentiation from diseases that manifest a similar clinical picture. It confirms the presence of an inflammatory process; clarifies the nature of inflammation; reveals functional disorders of the tracheobronchial tree; helps in identifying organic lesions of the bronchial tree. The study of the function of external respiration is carried out to identify restrictive and obstructive disorders of pulmonary ventilation. According to the spirogram, the Tiffno index and the air velocity indicator - PSDV are calculated. The joint assessment of bronchial resistance and lung volumes also helps to determine the level of obstruction. Radiopulmonography using the radioactive isotope 133Xe is performed to detect uneven ventilation associated with obstruction of the small bronchi. Electrocardiography is necessary to detect hypertrophy of the right ventricle and right atrium developing in pulmonary hypertension. A clinical blood test reveals secondary erythrocytosis resulting from chronic hypoxia with the development of severe pulmonary insufficiency. "Acute phase" indicators are expressed moderately. Microbiological examination of sputum and bronchial contents is important to identify the etiology of exacerbation of chronic bronchitis and the choice of antimicrobial therapy. 29. Differential diagnosis of chronic bronchitis (CB) Table Differential diagnostic criteria for CB
30. Treatment of chronic bronchitis (CB) Treatment. It includes a set of measures that differ during the period of exacerbation and remission of the disease. During the exacerbation of chronic bronchitis, two directions of treatment are distinguished: etiotropic and pathogenetic. Etiotropic treatment is aimed at eliminating the inflammatory process in the bronchi: therapy with antibiotics, sulfanilamide drugs, antiseptics, phytoncides, etc. is indicated. Treatment is started with antibiotics of the penicillin series (penicillin, ampicillin) or a group of cephalosporins (cefamesin, tseporin), and in the absence of effect, antibiotics of the group are used reserve (gentamicin, etc.). The most preferred route of administration is intratracheal (aerosol or fill with a laryngeal syringe through a bronchoscope). Pathogenetic treatment is aimed at improving pulmonary ventilation; restoration of bronchial patency; control of pulmonary hypertension and right ventricular failure. The restoration of pulmonary ventilation, in addition to the elimination of the inflammatory process in the bronchi, is facilitated by oxygen therapy and exercise therapy. The main thing in the treatment of chronic bronchitis - the restoration of bronchial patency - is achieved by improving their drainage and eliminating bronchospasm. To improve bronchial drainage, expectorants are prescribed (hot alkaline drink, decoctions of herbs, mukaltin, etc.), mucolytic drugs (acetylcysteine, bromhexine; with purulent viscous secretion - aerosols of proteolytic enzymes - chymopsin, trypsin); therapeutic bronchoscopy is used. To eliminate bronchospasm, eufillin is used (intravenously, in suppositories, tablets), ephedrine, atropine; single appointments in an aerosol of sympathomimetic drugs are possible: fenoterol, orciprenaline sulfate (asthmopenta) and a new domestic drug "Soventol", anticholinergic drugs: atrovent, troventol. Effective preparations of prolonged aminophylline (teopec, teodur, theobelong, etc.) - 2 times a day. In the absence of the effect of such therapy, small doses of corticosteroids are administered orally (10-15 mg of prednisolone per day) or intratracheally (hydrocortisone suspension - 50 mg). As an additional therapy, appoint: 1) antitussive drugs: with an unproductive cough - libexin, tusuprex, bromhexine, with a hacking cough - codeine, dionin, stoptussin; 2) drugs that increase the body's resistance: vitamins A, C, group B, biogenic stimulants. Currently, in the treatment of chronic bronchitis, immunocorrective drugs are increasingly being used: T-activin or thymalin (100 mg subcutaneously for 3 days); inside - catergen, sodium nucleinate or pentoxyl (within 2 weeks), levamisole (decaris). Physiotherapy treatment: prescribe diathermy, calcium chloride electrophoresis, quartz on the chest area, chest massage and breathing exercises. 31. Pneumonia. Etiology, pathogenesis, classification Pneumonia is an acute infectious and inflammatory disease of a focal nature, in which the respiratory sections and interstitial connective tissue of the lungs are involved in the pathological process. Classification by E. V. Gembitsky (1983). By etiology: 1) bacterial (indicating the pathogen); 2) viral (indicating the pathogen); 3) cornitic; 4) rickettsial; 5) mycoplasma; 6) fungal; 7) mixed; 8) infectious-allergic; 9) unknown etiology. By pathogenesis: 1) primary; 2) secondary. Clinical and morphological characteristics: 1) parenchymal: croupous; focal; 2) interstitial. By localization and extent: unilateral; bilateral. By severity: extremely severe; heavy; moderate; mild and abortive. Downstream: sharp; protracted (radiological and clinical resolution of pneumonia). Etiology. Most pneumonia is of infectious origin. Pneumonia allergic and caused by the action of physical or chemical factors are rare. Bacterial pneumonias are diagnosed more often in middle-aged and elderly people; viral pneumonia - in young people. In the etiology of primary bacterial pneumonia, the leading role belongs to pneumococci. During an influenza epidemic, the role of viral-bacterial associations (usually staphylococci), as well as opportunistic microorganisms, increases. In secondary pneumonia, the leading etiological role is played by gram-negative bacteria (klebsiella pneumoniae and influenza bacillus); in the occurrence of aspiration pneumonia, the importance of anaerobic infection is great. Pathogenesis. The infectious agent enters from the outside into the respiratory sections of the lungs through the bronchi: inhalation and aspiration (from the nasopharynx or oropharynx). By hematogenous route, the pathogen enters the lungs mainly in secondary pneumonia or in the thrombotic genesis of pneumonia. Lymphogenic spread of infection with the onset of pneumonia is observed only with injuries to the chest. Significant importance in the pathogenesis of pneumonia is also attached to allergic and autoallergic reactions. 32. Diagnosis of pneumonia The most significant for the diagnosis is the presence of a syndrome of inflammatory changes in the lung tissue. This syndrome consists of the following symptoms: 1) lag in breathing of the affected side of the chest; 2) shortening of percussion sound in the area of the projection of the lesion over a greater or lesser extent; 3) increased voice trembling and bronchophony in the same area; 4) change in the nature of breathing (hard, bronchial, weakened, etc.); 5) the appearance of pathological respiratory noises (wet, voiced fine bubbling rales and crepitus). The nature of breathing can change in different ways. In the initial stage of croupous pneumonia, breathing can be weakened, with an extended exhalation; in the hepatization phase, along with an increase in the dullness of the percussion sound, bronchial breathing is heard; with the resolution of the pneumonic focus with a decrease in percussion dullness, breathing becomes hard. Symptoms help to make an etiological diagnosis: 1) the detection of a small-spotted, as with rubella, rash in combination with lymphadenopathy is characteristic of adenovirus infection; 2) local enlargement of the lymph nodes indicates perifocal pneumonia; 3) fungal pneumonia combined with lesions of the mucous membranes, skin and nails; 4) hepatolienal syndrome and slight jaundice are found in cornitic and Curickettsial pneumonias; 5) for typical croupous pneumonia, the appearance of the patient is characteristic: a pale face with a feverish blush on the side of the lesion, herpetic eruptions, swelling of the wings of the nose when breathing. The most important method to clarify the presence of pneumonia and the degree of involvement of the lung tissue in the process is large-frame fluorography and X-ray examination of the chest organs. Bronchography reveals decay cavities in the lung tissue, as well as the presence of bronchiectasis, around which infiltrative changes (perifocal pneumonia) are possible during exacerbation. Bacteriological examination of sputum (or bronchial washings) before the appointment of antibiotics helps to detect the pathogen and determine its sensitivity to antibiotics. The severity of the inflammatory process is judged by the severity of acute-phase blood parameters and their dynamics (leukocytosis with a shift in the leukocyte formula, an increase in ESR, an increased content of a2-globulins, fibrinogen, the appearance of SRV, an increase in the level of sialic acids). With a prolonged course of pneumonia and the development of complications, the immunological reactivity of the body is studied. 33. Treatment of pneumonia Treatment. Immediately after the diagnosis is made, it is necessary to start etiotropic therapy of pneumonia. Of great importance are empirical ideas about a possible pathogen, since bacteriological examination of sputum has been carried out for quite a long time and in most patients, even with a modern approach to this study, it gives uncertain and sometimes erroneous results. At the moment, penicillins have lost their importance as the drug of choice in the treatment of pneumonia. In connection with the foregoing, in the treatment of pneumonia, much attention is paid to macrolides, which have proven effective not only against pneumococcus, but also against Mycoplasma pneumoniae, Chlamydia pneumoniae. Dosing of antibiotics used in the treatment of pneumonia. 1. Penicillins: benzylpenicillin (500-000 units intravenously every 1-000 hours or 000-6 units intramuscularly every 8 hours), ampicillin (500-000-1 g intramuscularly every 000-000 hours or 4 g every 0,5 hours intravenously), amoxicillin (1,0-2,0 g every 6 hours orally or 8-0,5 g every 6-0,5 hours intramuscularly, intravenously), oxacillin ( 1,0 g every 8-0,5 hours orally, intramuscularly, intravenously). 2. Cephalosporins: I generation - cephalothin (keflin) (0,5-2,0 g every 4-6 hours intramuscularly, intravenously), cefazolin (kefzol) (0,5-2,0 g, every 8 hours intramuscularly, intravenously ), II generation - cefuroxime (zinacef, ketocef) (0,75-1,5 g every 6-8 hours intramuscularly, intravenously), III generation - cefotaxime (claforan) (1,0-2,0 g, maximum up to 12 g / day every 12 hours intramuscularly, intravenously), ceftriaxone (longacef, rocefin) (1,0-2,0-4,0 g every 24 hours intramuscularly, intravenously). 3. Aminoglycosides: Genetamycin (80 mg every 12 hours IM, IV), Amikacin (10-15 mg/kg every 12 hours IM, IV), Tobramycin (Brulamycin) (3-5 mg/kg every 8 hours IM, IV) . 4. Macrolides: erythromycin (0,5 g every 6-8 hours orally or 0,5-1,0 g every 6-8 hours intravenously), rovamycin (3,0 million IU every 8-12 hours orally or 1,5. 3,0-8 million IU every 12-XNUMX hours IV). 5. Fluoroquinolones: pefloxacin (leflacin) (400 mg every 12 hours orally, IV), ciprofloxacin (cyprobay) (500 mg every 12 hours orally or 200-400 mg every 12 hours intravenously), ofloxacin (zanocin, tarivid) (200 mg every 12 hours orally). 6. Tetracyclines: doxycycline (vibramycin) (200 mg on day 1, on subsequent days - 100 mg every 24 hours orally), minocycline (minocin) (200 mg on day 1, on subsequent days - 100 mg every 12 hours orally), aztreonam (azactam) (1,0-2,0 g every 8-12 hours), imipenem/cilstatin (thienam) (500 mg every 6-8 hours intramuscularly). 34. Etiology, pathogenesis, clinical picture of acute esophagitis Acute esophagitis is an inflammatory lesion of the mucous membrane of the esophagus lasting from several days to 2-3 months. Etiology and pathogenesis. Etiological factors: infectious diseases, injuries, burns, poisoning, allergic reactions, nutritional errors. Of the infectious agents, the most characteristic of acute esophagitis are diphtheria, scarlet fever, typhoid and typhus, influenza, parainfluenza, adenovirus infection, mumps. Physical and chemical damaging factors are represented by ionizing radiation, chemical burns, hot and very cold food, and spices. clinical picture. Catarrhal esophagitis is the most common form of acute esophagitis. It occurs against the background of errors in nutrition: when eating spicy, cold, hot dishes, with minor injuries, alcohol burns. It is clinically manifested by burning and pain behind the sternum, forcing patients to refuse food for several days. Endoscopically noted esophagitis I-II degree, x-ray - hyperkinesia of the esophagus. Erosive esophagitis occurs with infectious diseases and allergies. Clinical symptoms are similar to those of catarrhal esophagitis. Hemorrhagic esophagitis is a rare clinical form of erosive esophagitis. The etiology is the same as in erosive esophagitis. Intense pain syndrome and hematemesis are clinically typical. The clinic is dominated by dysphagia and intense pain, aggravated after eating, nausea, vomiting. With vomit, fibrin films are released, there may be hemoptysis. Membraneous (exfoliative) esophagitis by etiology is chemical (burns of the esophagus), infectious. In the clinic of severe membranous esophagitis, intoxication, dysphagia and pain syndrome prevail. Necrotizing esophagitis is a rare form of acute inflammation of the esophagus. Its development is facilitated by reduced immunity in such serious diseases as sepsis, typhoid fever, candidiasis, end-stage renal failure. The clinic is characterized by painful dysphagia, vomiting, general weakness, bleeding, frequent development of mediastinitis, pleurisy, pneumonia. Septic esophagitis is a rare local or diffuse inflammation of the walls of the esophagus of streptococcal etiology or occurs when the mucosa is damaged by a foreign body, with burns, ulcers, and can pass from neighboring organs. Sometimes acute phlegmonous esophagitis occurs as a complication of any form of acute esophagitis, leading to purulent fusion of the walls of the esophagus. The clinical picture is characterized by severe intoxication, high fever, pain behind the sternum and in the neck, vomiting. On examination, there is swelling in the neck, mobility in this part of the spine is limited. The position of the head is forced, with an inclination to one side. The disease often transforms into purulent mediastinitis. 35. Treatment and prognosis of acute esophagitis Treatment. Principles of treatment of acute esophagitis: etiotropic, pathogenetic and symptomatic. Etiotropic treatment - treatment of the underlying disease. In infectious diseases complicated by acute esophagitis, antibiotics are used (parenterally). With pronounced necrotic and hemorrhagic changes in the esophagus, it is recommended to refrain from eating for 2-3 weeks. During this period, parenteral nutrition, intravenous administration of protein hydrolysates, mixtures of amino acids, intralipid, vitamins, and detoxification therapy are indicated. After reducing inflammation, thermally and chemically sparing foods are prescribed: warm milk, cream, vegetable soups, liquid cereals. To reduce local symptoms of inflammation - inside solutions of tannin 1%, collargol - 2%, novocaine - 1-2% before meals. Astringents are taken in a horizontal position with the head of the bed lowered low. In the absence of the effect of local administration of astringent preparations, non-narcotic analgesics are prescribed parenterally. To reduce the effects of esophageal dyskinesia, prokinetic drugs (cerucal, raglan, cisapride) are used orally before meals. With multiple erosions, bismuth preparations (denol, vikair), injections of solcoseryl are indicated. With hemorrhagic esophagitis, complicated by bleeding, aminocaproic acid preparations, vikasol, dicynone are used. With massive bleeding, a blood or plasma transfusion is prescribed. With purulent, necrotic esophagitis, the patient should be on parenteral nutrition for a long time, massive therapy with several antibiotics is used, and the abscess is drained. Esophageal strictures are corrected by bougienage. In rare cases, a gastrostomy is placed. Forecast. The prognosis of catarrhal and erosive esophagitis is favorable. Spontaneous disappearance of symptoms of esophagitis is possible, provided that the underlying disease is adequately corrected. The prognosis of pseudomembranous, exfoliative, phlegmonous esophagitis is serious. In all cases, subject to recovery from the underlying disease, esophagitis ends with the formation of cicatricial strictures, which require further correction. Patients with severe forms of esophagitis complicated by strictures of the esophagus are unable to work. Prevention of acute esophagitis consists in adequate and timely diagnosis and treatment of the underlying disease. 36. Etiology, pathogenesis, clinical picture of chronic esophagitis Chronic esophagitis is a chronic inflammation of the mucous membrane of the esophagus lasting up to 6 months. The most common variant is peptic esophagitis (reflux esophagitis), which can be complicated by peptic ulcer of the esophagus. Etiology and pathogenesis. The main cause of the disease is a constant reflux of gastric contents into the esophagus, sometimes bile and intestinal contents, i.e. peptic esophagitis is an aseptic burn of the esophagus by stomach acid. In the pathogenesis of reflux esophagitis, regurgitation of acidic contents and a violation of the purification and emptying of the esophagus from it are important. There are five criteria for the pathogenicity of reflux in the genesis of peptic esophagitis: frequency, volume, regurgitation, chemical composition, condition of the esophageal mucosa and sensitivity to a chemical factor (inflammation of the walls reduces sensitivity), emptying rate (clearance), which depends mainly on active peristalsis, alkalizing action saliva and mucus. The occurrence of reflux esophagitis is promoted by hernia of the esophageal opening of the diaphragm, duodenal ulcer, post-gastroresection disorders, and allergies. Allergic predisposition also matters. Morphological examination of patients with peptic esophagitis reveals edema, hyperemia of the mucosa, infiltration of the submucosa of the supradiaphragmatic segment of the esophagus. clinical picture. Typical signs of reflux esophagitis include burning behind the sternum, heartburn, regurgitation, which is aggravated by lying down, dysphagia, and the positive effect of taking antacids. There may be pain behind the sternum after eating, resembling angina pectoris. The occurrence of pain in reflux esophagitis is associated with peptic irritation of the esophageal wall and its spasms during regurgitation of acidic gastric contents, as well as with infringement of the prolapsed mucosa. Distinctive features of this pain: its long, burning character, localization in the xiphoid process, irradiation along the esophagus, less often to the left half of the chest, no noticeable effect from taking antacids, antispasmodics, increased in a horizontal position, especially after eating. Particular attention in clinical diagnosis should be given to minor symptoms of dysphagia, such as a feeling of a lump behind the sternum, a feeling of hot food passing through the esophagus. A sign of gradually beginning esophagitis may be salivation and the habit of drinking water with food. Physical examination of patients with reflux esophagitis does not provide diagnostically significant information. The complications of reflux esophagitis include bleeding, ulceration, strictures, shortening of the esophagus, and malignancy. Chronic reflux esophagitis can lead to the development of axial hiatal hernia. 37. Diagnosis, treatment of chronic esophagitis Diagnosis and differential diagnosis. The most valuable research method for this pathology is endoscopy, during which hyperemia, edema, and thickening of the mucosal folds are noted. It is necessary to differentiate reflux esophagitis with peptic ulcer of the stomach and duodenum, coronary heart disease, chronic cholecystitis and pancreatitis. The leading symptom in the differential diagnosis is pain. Differentiation with peptic ulcer is helped by the absence of late and "hungry" pains in esophagitis, as well as data obtained from endoscopy of the esophagus and stomach. Coronary pain, in contrast to esophagitis, is characterized by a connection with physical and emotional stress, the effect of nitrates, signs of ischemia on the ECG, including those according to bicycle ergometry. Ultrasound data of the abdominal organs help to exclude the pathology of the gallbladder and pancreas as the cause of the pain syndrome. Treatment. Therapy of reflux esophagitis includes the treatment of diseases that caused it, and the appointment of antireflux therapy. Patients are advised to avoid lifting weights, bending over. It is necessary to take the correct position during rest and sleep (the headboard is raised by 15-20 cm, at an angle of 30-50). It is recommended to normalize body weight, eat fractionally (the last meal - 3 hours before bedtime). Alcohol and spicy foods are excluded from the diet. Assign adsorbents and alkalizing drugs that have a protective effect on the mucous membrane. These substances include Venter, which is administered orally at a dose of 1 g (preferably in the form of a suspension) 30-40 minutes before meals 3 times a day and the 4th time on an empty stomach at bedtime. The course of treatment is 8-10 weeks. Almagel, phosphalugel, maalox, gastal have a similar effect. These drugs are used in the interdigestive period (1/2-2 hours after meals and at night) until complete remission occurs. Phosphalugel and Maalox are prescribed 1-2 packets 2-3 times a day, gastal - 2-3 tablets a day. Tea soda, a mixture of Bourget, white clay due to insufficient efficiency is not advisable to use. Enveloping and astringent action has bismuth nitrate 1 g 3-4 times a day. A high antireflux activity of a new antacid, topalkan, was noted. Mineral waters - "Borjomi", "Essentuki No. 4", "Jermuk", "Smirnovskaya" have an alkalizing effect. To reduce acidic gastric secretion, histamine H2 receptor blockers (cimetidine, ranitidine, famotidine), Ka-K-ATPase inhibitors (omeprazole), a selective blocker of M-cholinergic receptors of parietal cells, and its analogue buscopan are prescribed. Forecast and prevention. The prognosis for life and work is favorable. In a complicated course, the prognosis is determined by the timeliness and quality of medical care. Patients with a severe course are assigned a disability group. Patients with chronic reflux esophagitis should be under the supervision of a gastroenterologist. At least 2 times a year, endoscopic and morphological studies are indicated due to the possibility of malignancy. 38. Peptic ulcer of the esophagus Peptic ulcer of the esophagus is an acute or chronic disease characterized by ulceration of the mucosa of the distal segment of the esophagus under the influence of active gastric juice. Etiology and pathogenesis. Chronic peptic ulcers of the esophagus are complications of reflux esophagitis and hiatal hernia. Their occurrence is facilitated by the internal short esophagus, focal metaplasia of the mucosa, heterotopia of the gastric mucosa into the esophagus, reflux disease with cardia insufficiency, diseases accompanied by frequent vomiting (post-vagotomy syndrome, afferent loop syndrome, chronic alcoholism). Clinical picture. Symptoms of a peptic ulcer of the esophagus resemble the clinical picture of peptic esophagitis: persistent heartburn, worsening after eating, when bending the body, in a lying position, regurgitation, pain when swallowing, and impaired passage of solid food occur. The clinical symptoms of perforation are indistinguishable from the symptoms of acute penetrating and non-penetrating mechanical injury by foreign bodies. Approximately 14% of esophageal ulcers penetrate into the surrounding tissues. Diagnosis and differential diagnosis. Based on clinical symptoms, it is extremely difficult to suspect a peptic ulcer. The diagnosis is verified in the course of instrumental and laboratory research. The most informative X-ray and endoscopic examination. The most reliable information in the verification of peptic ulcer of the esophagus is provided by endoscopy and multiple biopsy from the edges of the ulcer. When advancing the endoscope to the peptic ulcer, signs of stage I-IV esophagitis, motor dysfunction of the esophagus, perifocal edema and hyperemia of the mucous membrane are revealed. It is necessary to differentiate peptic ulcers of the esophagus with ulcerations of a specific nature (with tuberculosis, syphilis). In these situations, specific serological tests, the results of histological and bacteriological studies significantly help. The combination of the pathology of the esophagus with damage to the lungs and other organs makes it necessary to purposefully examine the patient in relation to a specific process. Treatment. Treatment includes the appointment of a diet: mechanically and chemically sparing food is recommended, which is taken in small portions 5-6 times a day. To prevent reflux of contents from the stomach into the esophagus, the position of the patient in bed should be with a raised headboard. Medicines are taken lying down. Assign monotherapy with a drug of one of the following pharmacological groups: antisecretory, including antacids and adsorbents, stimulants of the motor-evacuation function of the stomach (prokinetics), drugs - mucus simulators. Therapy is carried out for a long time - 1,5-3 months. Indications for surgical treatment - lack of healing within 6-9 months, complicated course (perforation, penetration, stenosis, bleeding). Forecast and prevention. The prognosis for life and work is favorable. 39. Etiology, pathogenesis, clinical picture of chronic gastritis Chronic gastritis is a disease that is clinically characterized by gastric dyspepsia, and morphologically - by inflammatory and degenerative changes in the gastric mucosa, impaired cell renewal processes, and an increase in the number of plasma cells and lymphocytes in the mucous membrane's own membrane. Etiology and pathogenesis. At the present stage of development of gastroenterology, it has been established that the appearance of chronic gastritis is promoted by the microbial expansion of Helicobacter pylori (HP), which causes antral gastritis in 95% of cases and pangastritis in 56% of cases. The etiological factors of chronic gastritis can be attributed with a high degree of certainty to risk factors (irregular unbalanced diet, smoking, alcohol intake, hypersecretion of hydrochloric acid and pepsin). The leading role in the development of the disease also belongs to autoimmune mechanisms, accompanied by the accumulation of antibodies to the parietal cells of the gastric mucosa, aggravated heredity, as well as the use of drugs that have a damaging effect on the gastric mucosa. Classification. In 1990, at the IX International Congress of Gastroenterologists in Australia, a new systematization of chronic gastritis was adopted, called the Sydney system. Histological bases of classification. 1. Etiology: chronic gastritis associated with HP, autoimmune, idiopathic, acute drug-induced gastritis. 2. Topography: antral, fundal, pangastritis. 3. Morphology: acute, chronic, special forms. Endoscopic basis of classification: 1) gastritis of the antrum of the stomach; 2) gastritis of the body of the stomach; 3) pangastritis; 4) changes in the gastric mucosa: edema, erythema, mucosal vulnerability, exudate, flat erosions, elevated erosions, fold hyperplasia, fold atrophy, visibility of the vascular pattern, supramucosal hemorrhages. clinical picture. Chronic gastritis is one of the most common diseases in the clinic of internal diseases. Its frequency among the inhabitants of the globe ranges from 28 to 75%. Chronic gastritis is more often manifested by symptoms of gastric dyspepsia and pain in the epigastric region. Rarely, it is asymptomatic. An equally important place in the clinical picture of chronic gastritis is dyspeptic syndrome: nausea, belching (sour, bitter, rotten), heartburn, constipation or diarrhea, unstable stools. With isolated antral gastritis, complaints of heartburn and constipation, arising from the hypersecretion of hydrochloric acid and pepsin, become paramount. 40. Diagnosis and treatment of chronic gastritis Diagnostics. Chronic gastritis flows for a long time, with an increase in symptoms over time. Exacerbations are provoked by alimentary violations. The physical picture of chronic gastritis is rather poor. In 80-90% of patients during an exacerbation of the disease, an objective study determines only local pain in the epigastric region. When chronic gastritis is combined with duodenitis, cholecystitis or pancreatitis, localization of pain that is not typical for gastritis, but characteristic of the pathology of another organ, can be determined. An x-ray examination is more likely to exclude other diseases of the stomach (ulcer, cancer), help in the diagnosis of Menetrier's disease than to confirm the diagnosis of chronic gastritis. Due to the paucity of clinical manifestations of the disease, as well as the non-specificity of laboratory tests, the diagnosis of chronic gastritis is based on the results of endoscopic and morphological studies. Endoscopy reveals changes in the gastric mucosa of varying severity: edema, erythema, mucosal vulnerability, exudate, flat erosions, raised erosions, hyperplasia or atrophy of the folds, visibility of the vascular pattern, submucosal hemorrhages. Clinical manifestations characteristic of gastritis are also observed in other diseases of the digestive system, therefore, in the process of diagnosis, ultrasound of the abdominal cavity, a thorough endoscopic and morphological examination of the digestive organs are necessary. Treatment. Patients with gastritis need general medical measures: regular balanced nutrition, normalization of the work and rest regime, leveling of stressful situations of the domestic and industrial plan. Drug therapy is indicated only in the presence of clinical manifestations of chronic gastritis. Patients with gastritis associated with HP are treated according to the peptic ulcer program (see next lecture). Persons with autoimmune gastritis need vitamin B12 (500 mcg once a day subcutaneously for 1 days, followed by repeated courses of treatment), folic acid (30 mg per day), ascorbic acid (up to 5 g per day). If necessary, substitution therapy is carried out with enzyme preparations (mezim-forte, festal, enzistal, creon, pancitrate, acidin-pepsin). The pain syndrome is usually stopped by the appointment of antacids (maalox, almagel, gastal) or H-histamine receptor blockers (ranitidine, famotidine) in medium therapeutic doses. With special forms of gastritis, treatment of the underlying disease is necessary. Forecast and prevention. The prognosis for life and work is favorable. Prevention of gastritis is reduced to rational nutrition, compliance with the regime of work and rest, limiting the intake of NSAIDs. 41. Etiology of gastric ulcer Peptic ulcer (peptic ulcer) is a chronic, relapsing disease, clinically manifested by a functional pathology of the gastroduodenal zone, and morphologically - by a violation of the integrity of its mucous and submucosal layers, and therefore the ulcer always heals with the formation of a scar. Etiology. The main etiological factor of peptic ulcer is the microbial expansion of HP on the surface of the epithelium of the stomach. The significance of bacterial aggression in the etiology of the disease has been studied since 1983, when J. Warren and B. Marshall reported the discovery of a large number of S-spiral bacteria on the surface of the epithelium of the antrum of the stomach. Helicobacteria are able to exist in an acidic environment due to the production of the urease enzyme, which converts urea (from the bloodstream) into ammonia and carbon dioxide. The products of enzymatic hydrolysis neutralize hydrochloric acid and create conditions for changing the pH of the environment around each bacterial cell, thus providing favorable conditions for the vital activity of microorganisms. No less important in the development of peptic ulcers are neuropsychic effects, hereditary predisposition, infectious agents, alimentary errors and the intake of certain medications, and bad habits. Popular among researchers are hereditary factors: the inertia of the main nervous processes, group-specific properties of blood, immunological and biochemical features, hereditary burden syndrome. In the occurrence of peptic ulcer, essential importance was attached to alimentary violations. However, clinical and experimental studies conducted in the last two decades in most cases did not reveal the damaging effect of food products on the gastroduodenal mucosa. The prevalence of peptic ulcer disease among significant contingents of people with different dietary habits also testifies against the leading importance of nutritional factors. Disturbances in the rhythm and regularity of nutrition, long breaks between meals, untimely eating are essential for the occurrence of peptic ulcers. Researchers have expressed relatively conflicting views about the role of alcohol in ulcerogenesis. Alcohol is known to cause atrophic changes in the gastric mucosa. These observations are in conflict with the general concept of ulceration. The role of medicinal effects in ulcerogenesis is being actively studied. The results of studies published in the literature and our own data indicate that non-steroidal anti-inflammatory drugs and glucocorticoid hormones have the most pronounced ulcerogenic properties. 42. Diagnosis of gastric ulcer Diagnostics. In the uncomplicated course of peptic ulcer, there are no changes in the general blood test, some decrease in ESR, slight erythrocytosis are possible. With the addition of complications, anemia appears in blood tests, leukocytosis - when the peritoneum is involved in the pathological process. There are no changes in the general analysis of urine. The traditional method of research in the pathology of the stomach is the determination of the acidity of gastric contents. Various indicators are possible: elevated and normal, in some cases even reduced. A duodenal ulcer occurs with high acidity of gastric juice. In X-ray examination, a peptic ulcer is a "niche" - a depot of barium suspension. Gastroduodenoscopy with biopsy is the most reliable method for diagnosing peptic ulcer. It allows you to assess the nature of changes in the mucous membrane in the edge of the ulcer, in the periulcerous zone and guarantees the accuracy of the diagnosis at the morphological level. In endoscopic and morphological studies, it was found that most stomach ulcers are located in the area of the lesser curvature and antrum, much less often - on the greater curvature and in the area of the pyloric canal. 90% of duodenal ulcers are located in the bulbar region. A morphological study of a biopsy specimen obtained from the bottom and edges of the ulcer reveals cellular detritus in the form of an accumulation of mucus with an admixture of decaying leukocytes, erythrocytes and desquamated epithelial cells with collagen fibers located underneath. 43. Treatment of gastric ulcer Treatment. Rational therapy for peptic ulcer should include a regimen, appropriate nutrition, drug treatment, psychotherapy, physical and spa treatments. During the period of exacerbation of peptic ulcer, it is necessary to strictly observe the fragmentation in nutrition (from 4 to 6 times a day with a small amount of each serving of food taken at certain hours). Food products should have good buffering properties and contain a sufficient amount of protein (120-140 g). Psychotherapy is essential for stopping or reducing psychoneurotic reactions arising from persistent pain syndrome and its expectation. Medicines used to treat peptic ulcers are divided into 5 groups: 1) drugs that affect the acid-peptic factor (antacids and histamine H2 blockers, other antisecretory agents); 2) drugs that improve the gastric mucosal barrier; 3) drugs that increase the synthesis of endogenous prostaglandins; 4) antibacterial and antiseptic agents; 5) drugs that normalize motor-evacuation disorders of the stomach and duodenum. Antacids: 1) soluble (absorbable) - bicarbonate of soda, calcium carbonate (chalk) and magnesium oxide (burnt magnesia); 2) insoluble (non-absorbable): magnesium trisilicate and aluminum hydroxide. Several schemes of combination therapy (two-, three-, four-component). Two-component therapy: amoxicillin 1000 mg 2 times a day for 2 weeks; omeprazole 40 mg twice a day. The three-component scheme includes the preparation of colloidal bismuth 2 mg 120 times a day; tetracycline 4 mg 250 times a day; metronidazole 4 mg 250 times a day. The therapy cycle is 4 days. The four-component regimen involves omeprazole 20 mg 2 times a day from days 1 to 10; denol 120 mg 4 times a day from the 4th to the 10th day; tetracycline 500 mg 4 times a day from the 4th to the 10th day; metronidazole 500 mg 3 times a day from the 4th to the 10th day. The most effective is a four-component treatment regimen for gastric and duodenal ulcers. 6 weeks after its implementation, healing of the peptic defect is observed in 93-96% of patients. After scarring of a peptic ulcer of the stomach and duodenum, two types of treatment are traditionally used. 1. Continuous maintenance therapy is carried out with antisecretory drugs at half the daily dose for a period of up to one year. 2. Therapy "on demand", involves the use of one of the antisecretory agents in half the daily dose for two weeks when symptoms of peptic ulcer appear. 44. Chronic enteritis. Etiology, pathogenesis, classification Chronic enteritis is a disease of the small intestine, characterized by a violation of its functions (digestion and absorption) against the background of dystrophic and dysregenerative changes, culminating in the development of inflammation, atrophy and sclerosis of the mucous membrane of the small intestine. Etiology and pathogenesis. This is a polyetiological disease that can be the outcome of acute inflammation of the small intestine or a primary chronic process. In recent years, Yersinia, Helicobacteria, Proteus, Pseudomonas aeruginosa, rotaviruses, numerous representatives of protozoa and helminths (giardia, ascaris, tapeworms, opisthorchia, cryptosporidium) have been given great importance as an etiological factor in chronic enteritis. Of great importance in the occurrence of chronic enteritis are alimentary factors - overeating, eating dry food, unbalanced, predominantly carbohydrate foods, abuse of spices. Enteritis is caused by ionizing radiation, exposure to toxic substances, and drugs. Among the common pathogenetic mechanisms of chronic diseases of the small intestine, there are changes in the intestinal microflora against the background of a decrease in local and general immunity. Changes in the immune status - a decrease in the content of secretory lgA, an increase in the level of lgE, a decrease in blast transformation of lymphocytes and inhibition of leukocyte migration - lead to colonization of the small intestine by representatives of opportunistic microflora and a decrease in normal anaerobic flora. Morphologically, chronic enteritis is manifested by inflammatory and dysregenerative changes in the mucous membrane of the small intestine. If the process progresses, its atrophy and sclerosis are observed. Classification (Zlatkina A. R., Frolkis A. V., 1985). 1. Etiology: intestinal infections, helminthic invasions, alimentary, physical and chemical factors, diseases of the stomach, pancreas, biliary tract. 2. Phases of the disease: exacerbation; remission. 3. Degree of severity: mild; moderate; heavy. 4. Flow: monotonous; recurrent; continuously recurring; latent. 5. Character of morphological changes: eunit without atrophy; jeunitis with moderate partial villous atrophy; jeunitis with partial villous atrophy; eunit with total villous atrophy. 6. The nature of functional disorders: disorders of membrane digestion (disaccharidase deficiency), malabsorption of water, electrolytes, trace elements, vitamins, proteins, fats, carbohydrates. 7. Complications: solaritis, nonspecific mesadenitis. 45. Clinical picture and diagnosis of chronic enteritis clinical picture. The clinical picture of chronic enteritis consists of local and general enteric syndromes. The first is due to a violation of the processes of parietal (membrane) and cavity digestion (maldigestion). Patients complain of flatulence, pain in the paraumbilical zone, bloating in the form of a cap, loud rumbling, diarrhea, less often constipation. Palpation reveals pain in the mesogastrium, as well as on the left and above the navel (positive symptom of Porges), splashing noise in the region of the caecum (Obraztsov's symptom). Feces acquire a clayey appearance, polyfecalia is characteristic. General enteral syndrome is associated with impaired absorption of food ingredients (malabsorption), resulting in disorders of all types of metabolism, changes in homeostasis. Characterized by multifaceted metabolic disorders, primarily protein, which is manifested by a progressive loss of body weight. Changes in carbohydrate metabolism are less pronounced, which is manifested by bloating, rumbling in the abdomen and increased diarrhea while taking dairy products. To a large extent, the deficiency of body weight in patients is due not only to protein, but also to lipid imbalance. Changes in lipid metabolism are closely related to metabolic disorders of fat-soluble vitamins and minerals (calcium, magnesium, phosphorus). The characteristic signs of calcium deficiency are a positive symptom of the muscle roller, convulsions, recurrent "unmotivated" bone fractures, osteoporosis, osteomalacia. Diagnosis and differential diagnosis. A general blood test reveals micro- and macrocytic anemia, an increase in ESR, and in severe cases - lympho- and eosinopenia. If the disease is of parasitic origin, lymphocytosis and eosinophilia may be observed in the blood. A scatological examination reveals an intestinal type of steatorrhea due to fatty acids and soaps, creatorrhea, amylorrhea. The content of enterokinase and alkaline phosphatase in feces increases. The daily mass of feces increases significantly. A biochemical blood test reveals hypoproteinemia, hypoalbuminemia, hypoglobulinemia, hypocalcemia, decreased levels of magnesium, phosphorus, and other microelements, disturbances in electrolyte metabolism in the form of decreased sodium and potassium levels. The morphological picture of a mild form of chronic enteritis is characterized by thickening of the villi, their deformation, a decrease in the depth of the notches, a decrease in the tone of smooth muscles, subepithelial edema, degenerative changes in the surface of the epithelium, thinning of the brush border of cells, a decrease in the number of goblet cells in the region of the villi, an increase in the number of crypts, infiltration of the own layer mucosa with lymphoplasmacytic elements, a decrease in Paneth cells in the area of the bottom of the crypts. 46. Treatment, prognosis of chronic enteritis Treatment. Treatment of chronic enteritis should be comprehensive, including agents that affect etiological factors, pathogenetic mechanisms, as well as local and general symptoms of the disease. The basis is dietary nutrition, which helps to reduce the increased osmotic pressure in the intestinal cavity, reduces secretion, and normalizes the passage of intestinal contents. Drug therapy should be etiotropic, pathogenetic and symptomatic. Etiotropic treatment: for grade II-IV dysbiosis, antibacterial drugs are prescribed: metronidazole (0,5 g 3 times a day), clindamycin (0,5 g 4 times a day), cephalexin (0,5 g 2 times a day). day), biseptol (0,48 g 2 times a day), sulgin (1 g 3-4 times a day), furazolidone (0,1 g 4 times a day). After using antibacterial drugs, eubiotics are prescribed - bifidumbacterin or bificol 5 doses 3 times a day 30 minutes before meals, colibacterin or lactobacterin 3 doses 3 times a day before meals, hilak-forte 40 drops 3 times a day before meals. Treatment with bacterial preparations is carried out for a long time: 3 courses of 3 months each year. For staphylococcal dysbacteriosis, an antistaphylococcal bacteriophage is prescribed (20 ml 3 times a day for 15-20 days), for proteus dysbacteriosis - coliprotean bacteriophage orally, 20 ml 3 times a day, the course of treatment is 2-3 weeks. To improve the digestion process, enzymes are recommended: pancreatin, panzinorm forte, festal, digestal, pankurmen, mezim forte, trienzyme, the doses of which are selected individually (from 1 tablet 3 times a day to 3-4 tablets 4 times a day) and which are prescribed directly before or during meals for 2-3 months. If necessary, enzyme replacement therapy is continued for a longer time. To correct water and electrolyte disorders, intravenous administration of panangin 20-30 ml, calcium gluconate 10% 10-20 ml in 200-400 ml of isotonic solution or glucose solution, polyionic solutions "Disol", "Trisol", "Quartasol" are indicated. Electrolyte solutions are administered intravenously for 10-20 days under the control of the acid-base state and the level of blood electrolytes. Forecast and prevention. The prognosis for life and working capacity in most cases is favorable. Prognostically unfavorable signs are a continuously relapsing course of the disease, a sharp significant weight loss, anemia, a syndrome of endocrine disorders (decreased libido, dysmenorrhea, infertility). Prevention of chronic enteritis consists in the timely treatment of acute intestinal infections and concomitant diseases of the gastroduodenal zone, in observing the diet, in the prophylactic administration of bacterial preparations during X-ray and radiotherapy. 47. Etiology, pathogenesis, clinical picture of Crohn's disease Crohn's disease is a chronic bowel disease with systemic manifestations; the morphological basis of which is granulomatous autoimmune inflammation of the gastrointestinal tract. Etiology and pathogenesis. The etiology and pathogenesis of the disease are not well understood. The most popular are the infectious and immune concepts of the onset of the disease. In recent years, there have been reports of the etiological role of microorganisms of the genus Yersinia. However, it is difficult to establish whether these microbial agents are pathogens or commensals. At the same time, changes in the intestinal microflora play an important role in the pathogenesis of the disease. Typically, a decrease in bifidum-type bacteria with a simultaneous increase in enterobacteria with signs of pathogenicity. Autoimmune mechanisms play a role in the development of the disease. In Crohn's disease, autoantibodies (lgC, lgM) appear against intestinal tissues. Classification. Classification (F. I. Komarov, A. I. Kazanov, 1992). 1. Course: acute; chronic. 2. Characteristics of the process: lesion within the small intestine; lesion within the ileocecal region; lesion within the colon. 3. Complications: narrowing of the intestine; toxic dilatation of the colon; fistulas; amyloidosis; nephrolithiasis, cholelithiasis; B12 deficiency anemia. clinical picture. The clinical picture of Crohn's disease is characterized by considerable diversity, which is determined by the localization and extent of the pathological process in the intestine, the form of the disease and the addition of complications. An objective study pays attention to the pallor of the skin, which correlates with the severity of anemia, swelling in the legs due to impaired absorption and protein metabolism. On palpation of the abdomen, flatulence and rumbling are noted. During physical examination of the patient, pallor of the skin, subfebrile condition, body weight deficiency are determined, palpation reveals spasmodic bowel loops, pain in the paraumbilical zone, in the right iliac region. In Crohn's disease, extraintestinal signs of the disease are noted: aphthous stomatitis, phlegmon and fistulas of the oral cavity, arthritis, resembling rheumatoid arthritis in the clinic, with characteristic symptoms of symmetrical lesions of small joints, stiffness in the morning. Typical changes in the eyes: iritis, iridocyclitis, maculopathy. The skin may develop erythema nodosa and pyoderma gangrenosum. Diarrhea is characterized by an increase in the frequency of stools up to 10 times a day or more, polyfecal matter. The volume of the stool is determined by the anatomical localization of the process. Weight loss is noted in all patients. 48. Diagnosis of Crohn's disease Diagnosis and differential diagnosis. In a clinical blood test during an exacerbation, leukocytosis, anemia, and an increase in ESR are detected. Changes in the general analysis of urine appear in severe form, characterized by the addition of amyloidosis of the kidneys (proteinuria). A biochemical blood test reveals hypoproteinemia, hypoalbuminemia, an increase in a-globulins, a decrease in the content of iron, vitamin B12, folic acid, zinc, magnesium and potassium. The data of scatological examination allow to indirectly assess the level of the lesion. In the coprogram with small intestinal localization of the process, polyfecal matter, steatorrhea, creatorrhoea are found; with the colon - an admixture of mucus, leukocytes, erythrocytes. X-ray diagnostics allows you to establish the localization and prevalence of the pathological process in the intestine. Areas of the affected intestine alternate with areas of the unchanged intestine. The altered loops become rigid, the picture is mosaic with small filling defects and with the penetration of contrast beyond the intestinal wall in the form of pockets. The intestine in the affected area acquires the character of finely fringed, with the formation of pseudodiverticula. The contractile capacity of the intestinal wall is reduced or completely lost, the evacuation of barium slows down. An uneven narrowing of the intestinal lumen is observed, as a result, it becomes so narrow that it takes on the form of a lace. Above the zone of narrowing, the intestine expands. Endoscopic diagnosis is of decisive importance in the verification of the diagnosis. For Crohn's disease, the most characteristic is the change in the antrum of the stomach and the initial section of the duodenum. Endoscopically, it is possible to detect a circular narrowing of the antrum, resembling tumor stenosis. The initial period of Crohn's disease is characterized by poor endoscopic data: a dull mucous membrane, against which erosions of the aphthae type are visible, surrounded by whitish granulations. The vascular pattern is absent or smoothed out. In the lumen of the intestine and on its walls, purulent mucus is determined. In clinical remission, the described changes may disappear completely. As the disease progresses, the mucosa becomes unevenly thickened, has a whitish color, and large superficial or deep fissure ulcers are noted. The intestinal lumen narrows, making it difficult to advance the colonoscope. Colonoscopy makes it possible to perform a targeted biopsy of the mucous membrane in any part of the colon and in the terminal ileum. In Crohn's disease, the pathological process begins in the submucosal layer, so the biopsy should be performed in such a way that a portion of the submucosal layer enters the biopsy material. In connection with the above, in 54% of cases the morphological substrate of the disease is not detected. 49. Treatment of Crohn's disease Treatment. A mechanically and chemically sparing diet is prescribed with a high content of proteins, vitamins, microelements, with the exception of milk in case of its intolerance, and the restriction of coarse plant fiber. The use of liquid enteral hydrolysates is shown. Salazopreparations and corticosteroids form the basis of pathogenetic drug therapy. The daily dose of drugs is 3-6 g. With the localization of the pathological process in the large intestine, the activity of sulfasalazine exceeds the activity of prednisolone. In the absence of the effect of the use of sulfasalazine, with lesions predominantly of the small intestine and pronounced signs of immune inflammation, as well as in the presence of systemic manifestations of the disease, the use of corticosteroids is indicated. The effect of their use is noted in the first 8 weeks from the start of treatment. Prednisolone is prescribed according to the following scheme: at the height of an exacerbation, 60 mg per day, then the dose is gradually reduced and by the 6-10th week is adjusted to a maintenance dose of 5-10 mg per day. Upon reaching clinical remission, the drug is gradually canceled. If remission is not achieved, treatment with prednisolone is continued on an outpatient basis until 52 weeks. In severe course of the disease, in case of complications in the form of torpid current rectovaginal, skin-enteral, entero-enteral fistulas, the appointment of 6-mercaptopurine orally at 0,05 g 2-3 times a day is indicated for 10-day courses with an interval of 3 days until reaching clinical remission. Subsequently, they switch to taking maintenance doses of the drug during the year. The dose of 6-mercaptopurine in this case is 75 mg per day. The effect of treatment with immunosuppressants can be determined no earlier than after 3-4 months. Metronidazole has found widespread use in the treatment of Crohn's disease, the main indications for which are perianal fistulas and fissures, lack of effect from salazal drugs and glucocorticoids, as well as relapses of the disease after proctectomy. The drug is prescribed at a dose of 500-1000 mg per day. The duration of the continuous course should not exceed 4 weeks. Symptomatic therapy for Crohn's disease is reduced to the prescription of short courses (2-3 days) of antidiarrheal drugs (imodium, loperamide). Doses are selected individually according to the clinical effect. Antidiarrheal drugs should not be prescribed for a long time (more than 5 days). Due to the presence of malabsorption syndrome in Crohn's disease, enzyme preparations that do not contain bile acids (pancreatin, mezim-forte, solisim, somilase) are used in a dose of 2 to 6 tablets with each meal. According to indications, anemia and hypoalbuminemia are corrected by prescribing iron supplements (parenterally) and administering alvesin, protein hydrolysers, aminopeptide, aminokrovin. Multivitamins are prescribed in pills and essentials in capsules. Treatment of dysbiosis is carried out according to general rules. 50. Classification of nonspecific ulcerative colitis Nonspecific ulcerative colitis is an inflammatory disease that affects the mucous membrane of the colon with ulcerative-destructive changes, which has a chronic relapsing course, often accompanied by the development of life-threatening complications. Classification (Yu. V. Baltaitis et al., 1986). Clinical characteristic. 1. Clinical form: 1) acute; 2) chronic. 2. Current: 1) rapidly progressing; 2) continuously relapsing; 3) recurrent; 4) latent. 3. Degree of activity: 1) exacerbation; 2) fading exacerbation; 3) remission. 4. Severity: 1) light; 2) moderate; 3) heavy. Anatomical characteristic. 1. Macroscopic characteristic: 1) proctitis: 2) proctosigmoiditis; 3) subtotal lesion; 4) total defeat. 2. Microscopic characteristic: 1) the predominance of destructive-inflammatory processes; 2) reduction of inflammatory processes with elements of reparation; 3) consequences of the inflammatory process. Complications. 1. Local: 1) intestinal bleeding; 2) perforation of the colon; 3) narrowing of the colon; 4) pseudopolyposis; 5) secondary intestinal infection; 6) disappearance of the mucous membrane; 7) toxic dilatation of the colon; 8) malignancy. 2. General: 1) functional hypocorticism; 2) sepsis; 3) systemic manifestations - arthritis, sacroiliitis, skin lesions, iritis, amyloidosis, phlebitis, sclerosing cholangitis, liver dystrophy. 51. Clinical picture of ulcerative colitis clinical picture. The clinic of ulcerative colitis is polymorphic and depends on the severity of the course and the severity of the process. The course of the inflammatory process, considered more often as chronic, in some cases takes on an acute character. The extent of the colonic lesion may also vary. For nonspecific ulcerative colitis, 3 leading symptoms are characteristic: the release of scarlet blood during bowel movements, impaired bowel function, and abdominal pain. Intestinal dysfunction manifests itself in the form of complaints of repeated unstable stools, which is the result of extensive damage to the mucous membrane and a decrease in the absorption of water and salts. Most often, diarrhea occurs with severe ulcerative colitis. However, diarrhea is not a reliable indicator of the severity of the process. The severity of diarrhea in combination with the presence of red blood in the stool matters. In a significant number of patients with ulcerative colitis, blood and mucus are periodically found on the surface of the formed feces, which is often mistakenly regarded as a manifestation of hemorrhoids. The mild course of nonspecific ulcerative colitis is characterized by a satisfactory condition of patients. Pain in the abdomen is moderate and short-term. The chair is decorated, speeded up, up to 2-3 times a day. Blood and mucus are found in the stool. The process is localized within the rectum and sigmoid colon. The clinical course is recurrent. The effect of treatment with salazopreparations is satisfactory. Relapses occur no more than 2 times a year. Remissions can be long (more than 2-3 years). The moderate course of the disease is diagnosed if the patient has diarrhea. The chair is frequent (up to 6-8 times a day), in each portion an admixture of blood and mucus is visible. Cramping pains in the abdomen are more intense. There are intermittent fever with a rise in body temperature up to 38 C, intense general weakness. There may also be extraintestinal manifestations of the disease (arthritis, uveitis, erythema nodosum). The course is continuously recurrent, the effect of salazopreparations is unstable, hormones are prescribed during exacerbations. The severe form of the disease is characterized by an acute onset. A total lesion of the large intestine rapidly develops with the spread of the pathological process deep into the intestinal wall. The patient's condition deteriorates sharply. The clinic is characterized by a sudden onset, high fever, profuse diarrhea up to 24 times a day, profuse intestinal bleeding, and a rapid increase in dehydration. Tachycardia appears, blood pressure decreases, extraintestinal manifestations of nonspecific ulcerative colitis increase. Conservative treatment is not always effective, and emergency surgery is often required. 52. Diagnosis of nonspecific ulcerative colitis Diagnosis and differential diagnosis. In clinical blood tests with a mild form of the disease, slight neutrophilic leukocytosis, an increase in ESR, and red blood counts are not changed. As the severity of the course increases and the duration of the exacerbation increases, anemia of mixed genesis occurs (B12-deficient and iron-deficient), and the ESR increases. In the biochemical analysis of blood in moderate and severe forms, dysproteinemia, hypoalbuminemia, hypergammaglobulinemia, electrolyte imbalance, and acid-base state are noted. In the general analysis of urine, changes appear only when complications arise in the form of nephrotic syndrome against the background of amyloidosis, when characteristic changes in urine tests are noted - proteinuria, "dead" urinary sediment, there is also an increase in the blood and the level of creatinine, urea. The main role in the diagnosis is acquired by endoscopic examination with targeted biopsy, since in nonspecific ulcerative colitis, the colon mucosa is primarily affected. The rectum is always involved in the pathological process, i.e., erosive and ulcerative changes are detected during endoscopy immediately behind the anal sphincter during sigmoidoscopy. In ulcerative colitis, the rectosigmoid bend is not always possible to overcome due to severe spasm. An attempt to hold the tube of the proctoscope is accompanied by severe pain. In this situation, the proctoscope should be inserted to a depth of no more than 12-15 cm. The endoscopic picture depends on the form of the disease. With a mild form, edematous dull mucous membrane, thick whitish overlays of mucus on the walls of the intestine, and slight contact bleeding are visible. The vascular pattern of the submucosal layer is not visually determined. In the moderate course of the disease, hyperemia and edema of the mucous membrane, severe contact bleeding, hemorrhages, erosions and irregularly shaped ulcers, thick overlays of mucus on the walls of the intestine are revealed. In a severe course of the disease, the mucous membrane of the colon is destroyed over a considerable extent. A granular, bleeding inner surface, extensive areas of ulceration with fibrinous deposits, pseudopolyps of various sizes and shapes, pus and blood in the intestinal lumen are found. Contraindications for colonoscopy and sigmoidoscopy are severe forms of ulcerative colitis in the acute stage of the disease. In the presence of an epidemic of intestinal infections, the diagnosis is easily established. But even in the case of sporadic morbidity in acute intestinal infections, the colitis syndrome flows without relapses, while ulcerative colitis has a relapsing course. The most accurate methods for identifying acute intestinal infection include bacteriological and serological. 53. Treatment of nonspecific ulcerative colitis Treatment. The absence of a single etiological factor and the complexity of the pathogenesis of nonspecific ulcerative colitis make it difficult to treat this disease. Anti-inflammatory and antibacterial drugs are used: salazopyridazine, sulfasalazine, salazodimethoxin, salofalk. Ingested sulfasalazine, with the participation of intestinal microflora, breaks down into 5-aminosalicylic acid and sulfapyridine. Unabsorbed sulfapyridine inhibits the growth of anaerobic microflora in the intestine, including clostridia and bacterioids. And thanks to 5-amino-salicylic acid, the drug not only causes changes in the intestinal microflora, but also modulates immune responses, blocks the mediators of the inflammatory process. The drug is prescribed at a dose of 2-6 g per day for the entire period of active inflammation. When the colitis syndrome subsides, the dose of sulfasalazine is reduced gradually, bringing it to a maintenance dose (an average of 1-1,5 tablets per day). In severe diarrheal syndrome in persons with mild and moderate course of the disease, the appointment of sandostatin is indicated, which inhibits the synthesis of gastrointestinal hormones and biogenic amines (vasoactive intestinal peptide, gastrin, serotonin), the production of which is sharply increased in ulcerative colitis and Crohn's disease. And also the drug reduces secretion and improves absorption in the intestine, inhibits visceral blood flow and reduces motility. When using sandostatin (within 7 days at a dose of 0,1 mg 2 times, subcutaneously), diarrhea decreases, tenesmus practically disappears, and blood excretion with feces decreases. In a severe form of nonspecific ulcerative colitis, treatment is carried out against the background of parenteral nutrition. The protein content of these preparations should be approximately 1,5-2,0 g/kg of body weight. Corticosteroids, which are administered parenterally, are a pathogenetic treatment for a severe form of the disease: during the first day, prednisone is administered intravenously at intervals of 12 hours (90-120 mg or more), in the next 5 days - intramuscularly, gradually reducing the dose. With a positive effect, they switch to oral medication (prednisolone 40 mg per day). In the moderate form of the course of nonspecific ulcerative ulcer, a strict diet is required with a restriction of fiber, dairy products and a high protein content. Prednisolone is administered orally at an initial dose of 20-40 mg per day. Treatment can be supplemented with sulfasalazine and its analogues, which are taken orally or administered in microclysters and suppositories into the rectum. The initial dose of sulfasalazine is 1 g per day, then it is increased to 4-6 g. As an auxiliary method of treatment, decoctions of herbs with anti-inflammatory and hemostatic effects (burnet root, nettle leaf, lichen, gray alder cones, licorice root) can be used, herbal medicine often allows you to reduce the dose of salazopreparations, prolong remission. 54. Clinical picture of acute gromerulonephritis Acute glomerulonephritis (AGN) is an acute diffuse kidney disease of an infectious-allergic nature, localized in the glomeruli. AGN can be an independent disease (primary) or be secondary as part of another disease, complicating the clinical picture and diagnosis of the latter. AGN usually affects young and middle-aged men. clinical picture. The clinical picture of the disease consists of the following syndromes. urinary syndrome. 1. Proteinuria due to the passage of protein molecules through the spaces of the capillary wall of the glomerulus, formed during the deposition of immune complexes on them. Proteinuria is selective in nature, in which predominantly albumins pass through the glomerular "filter". 2. Hematuria due to involvement in the pathological process of capillary mesangium and interstitial tissue. Erythrocytes penetrate through the smallest breaks in the basement membrane, changing their shape. 3. Cylindruria - urinary excretion of cylindrical cells of the tubules. During dystrophic processes in the tubules of the disintegrated cells of the renal epithelium, granular cylinders are formed, consisting of a dense granular mass; waxy cylinders have sharp contours and a homogeneous structure; hyaline casts are proteinaceous formations. Hypertensive syndrome is observed due to: 1) sodium and water retention; 2) activation of the renin-angiotensin-aldosterone and sympathoadrenal systems; 3) decrease in the function of the depressor system of the kidneys. Edema syndrome is associated with the following factors: 1) a decrease in glomerular filtration due to their defeat; 2) a decrease in the filtration charge of sodium and an increase in its reabsorption; 3) water retention due to sodium retention in the body; 4) an increase in BCC; 5) secondary hyperaldosteronism; 6) an increase in the secretion of ADH and an increase in the sensitivity of the distal nephron to it, leading to fluid retention; 7) an increase in the permeability of the capillary walls and the release of plasma into the tissues; 8) a decrease in plasma oncotic pressure with massive proteinuria. 55. Diagnosis of acute gromerulonephritis Diagnostics. In 100% of cases, urine tests are diagnosed with proteinuria of varying severity, cylindruria and, most importantly for diagnosis, hematuria of varying severity - from microhematuria (up to 10 erythrocytes per field of view) to macrohematuria (although quite rare). However, if AGN is suspected, it is necessary to conduct a series of repeated urine tests or put a Nechiporenko test (determination of the number of formed elements in 1 μl), since erythrocytes may not be detected in a single portion of urine. A blood test reveals acute phase indicators (increased levels of fibrinogen and a2-globulin, C-reactive protein, accelerated ESR), the number of leukocytes changes little, moderate anemia. With an uncomplicated course of AGN, the content of nitrogenous substances (creatinine, indican, urea) in the blood does not change. In the initial phase of the disease, a change in the Reberg test is observed - a decrease in glomerular filtration and an increase in tubular reabsorption, which normalizes as it recovers. An x-ray examination in patients with severe arterial hypertension may show a moderate increase in the left ventricle, which takes on the same size as the patient recovers. There are 3 clinical variants of AGN. 1. Monosymptomatic variant: minor complaints, absence of edema and arterial hypertension, there is only urinary syndrome; the most common variant of the course of the disease (86% of cases). 2. Nephrotic variant: edema, oliguria are pronounced, it is possible to increase blood pressure to relatively low numbers, it is detected in 8% of patients. 3. Extended version: arterial hypertension, reaching high numbers (180/100 mm Hg), moderately pronounced edema, circulatory failure, occurs in 6% of cases. 56. Treatment of acute gromerulonephritis Treatment. Treatment for AGN is complex and includes the following activities. 1. Mode. If AGN is suspected or immediately after the diagnosis is established, the patient should be immediately hospitalized. Strict bed rest must be observed for about 2-4 weeks until the elimination of edema and normalization of blood pressure. Staying in bed provides uniform warming of the body, which leads to a decrease in vasospasm (hence, to a decrease in blood pressure) and to an increase in glomerular filtration and diuresis. After discharge from the hospital, home treatment is indicated for up to 4 months from the date of onset of the disease, which is the best prevention of the transition of AGN to the chronic stage. 2. Diet. Depending on the severity of clinical symptoms, it is very important to restrict fluid and sodium chloride. With an expanded and nephrotic form, a complete fast is recommended for 1-2 days with fluid intake in an amount equal to diuresis. On the 2-3rd day, the consumption of food rich in potassium salts (rice porridge, potatoes) is shown. The total amount of water drunk per day should be equal to the volume of urine allocated for the previous day plus 300-500 ml. After 3-4 days, the patient is transferred to a diet with protein restriction (up to 60 g per day), and the total amount of salt is not more than 3-5 g / day. Such a diet is recommended until the disappearance of all extrarenal symptoms and a sharp improvement in urinary sediment. 3. Drug therapy includes, first of all, antibacterial therapy, which, however, should be carried out only if the infectious nature of AGN is reliably established (the pathogen has been isolated and no more than 3 weeks have passed since the onset of the disease). Usually prescribed penicillin or its semi-synthetic analogues in conventional dosages. The presence of obvious foci of chronic infection (tonsillitis, sinusitis, etc.) is also a direct indication for antibiotic therapy. Diuretics in the treatment of AGN are indicated only with fluid retention, increased blood pressure and the appearance of heart failure. The most effective furosemide (40-80 mg), used until the elimination of edema and hypertension. There is no need for a long-term prescription of these drugs, 3-4 doses are enough. In the absence of edema, but persistent hypertension or with an insufficient antihypertensive effect of saluretics, antihypertensive drugs (clophelin, dopegyt) are prescribed with a duration of administration that depends on the persistence of arterial hypertension. With prolonged proteinuria, indomethacin or voltaren is prescribed at 75-150 mg per day (in the absence of hypertension and oliguria). The prognosis is favorable, however, with prolonged forms, there is a possibility that the process will become chronic. Prevention of AGN comes down to effective treatment of focal infection, rational hardening. In order to timely detect the onset of the disease after vaccination, transferred ARVI in all patients, it is necessary to examine the urine.
▪ Constitutional law of foreign countries. Crib
Artificial leather for touch emulation
15.04.2024 Petgugu Global cat litter
15.04.2024 The attractiveness of caring men
14.04.2024
▪ Origins of human speech found ▪ Cows are divided into optimists and pessimists ▪ K70 RGB Pro Mechanical Keyboard
▪ section of the site Aphorisms of famous people. Article selection ▪ Philosophy article. Lecture notes ▪ Article Who first announced that the Earth revolves around the Sun? Detailed answer ▪ article Toroidal antennas. Encyclopedia of radio electronics and electrical engineering
Home page | Library | Articles | Website map | Site Reviews www.diagram.com.ua |






 Arabic
Arabic Bengali
Bengali Chinese
Chinese English
English French
French German
German Hebrew
Hebrew Hindi
Hindi Italian
Italian Japanese
Japanese Korean
Korean Malay
Malay Polish
Polish Portuguese
Portuguese Spanish
Spanish Turkish
Turkish Ukrainian
Ukrainian Vietnamese
Vietnamese

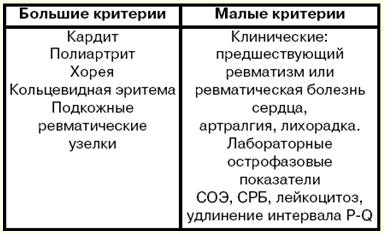


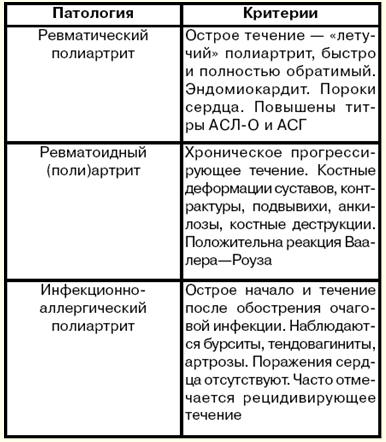

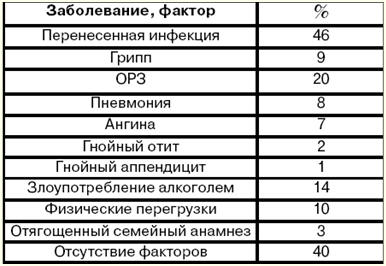



 See other articles Section
See other articles Section 