
|
|
Lecture notes, cheat sheets
Anesthesiology and resuscitation. Cheat sheet: briefly, the most important
Directory / Lecture notes, cheat sheets Table of contents
1. The concept of resuscitation Resuscitation is a branch of clinical medicine that studies the problems of revitalizing the body, developing principles for the prevention of terminal conditions, methods of resuscitation and intensive care. Practical methods of revitalizing the body are united by the concept of "resuscitation". Resuscitation (from Latin "revival" or "animation") is a system of measures aimed at restoring sharply impaired or lost vital functions of the body and removing it from a terminal state and clinical death. Effective resuscitation measures are indirect heart massage and artificial ventilation of the lungs. If they are ineffective within 30 minutes, biological death is ascertained. Intensive care is a set of measures used to treat severe, life-threatening conditions and involves the use of a wide range of therapeutic measures, according to indications, including intravenous infusions, prolonged mechanical ventilation, electrical pacing, dialysis methods, etc. A critical state is the impossibility of maintaining the integrity of body functions as a result of an acute dysfunction of an organ or system, requiring drug or hardware-instrumental replacement. The terminal state is a borderline state between life and death, a reversible extinction of body functions, including the stages of preagony, agony and clinical death. Clinical death is a terminal condition in which there is no blood circulation and respiration, the activity of the cerebral cortex stops, but metabolic processes are preserved. With clinical death, the possibility of effective resuscitation remains. The duration of clinical death is from 5 to 6 minutes. Biological death is an irreversible cessation of physiological processes in organs and tissues, in which resuscitation is impossible. It is established by a combination of a number of signs: the absence of spontaneous movements, contractions of the heart and pulse in large arteries, respiration, reactions to painful stimuli, corneal reflex, maximum pupil dilation and the absence of their reaction to light. Reliable signs of the onset of death are a decrease in body temperature to 20 C, the appearance of cadaveric spots and muscle rigor mortis. 2. Basic manipulations in intensive care Percutaneous puncture and catheterization of the main vein (subclavian). Indications: large volumes of infusion-transfusion therapy, parenteral nutrition, detoxification therapy, intravenous antibiotic therapy, probing and contrasting of the heart, measurement of CVP, implantation of a pacemaker, impossibility of catheterization of peripheral veins. Contraindications: violation of the blood coagulation system, inflammatory and purulent process at the site of puncture and catheterization, trauma in the clavicle, superior vena cava syndrome, Paget-Schretter syndrome. Instrumentation and accessories for puncture and catheterization: puncture needle, a set of plastic catheters, a set of conductors, a 10 ml syringe for intramuscular injections, scissors, a needle holder, a surgical needle and a silk ligature, an adhesive plaster. Technique: catheterization is carried out in compliance with the rules of asepsis and antisepsis, treatment of the operator's hands, the operating field and wrapping with sterile material. The position of the patient is horizontal on the back with the arms brought to the body and the lapel of the head in the opposite direction. Local anesthesia is used - 0,5-1% novocaine solution. The puncture is best done on the right, since when puncturing the left subclavian vein, there is a danger of damaging the thoracic lymphatic duct. Puncture point - on the border of the inner and middle third of the clavicle 2 cm below it. The needle is passed slowly at an angle of 45 to the collarbone and 30-40 to the surface of the chest between the clavicle and the 15st rib in the direction of the upper edge of the sternoclavicular joint. When passing the needle, the syringe plunger is periodically tightened to determine if it enters the vein, and novocaine is injected along the needle. When piercing a vein, sometimes there is a feeling of failure. After entering the vein, the syringe is disconnected from the needle and the cannula is closed with a finger. Then a conductor is inserted through the needle to a length of 20-6 cm and the needle is removed. A catheter of the appropriate diameter is passed through the conductor and, together with the conductor, is inserted into the vein by 8-2 cm, after which the conductor is carefully removed. To check the correct position of the catheter, a syringe is attached to it and 3-3 ml of blood is drawn into it, after which a plug is placed or infusion therapy is started. The catheter is fixed with a silk ligature to the skin. To do this, a sleeve of adhesive plaster is made on the catheter 5-XNUMX mm from the skin, on which silk is tied, then passed through the ears of the catheter and tied again. After fixing the catheter, the puncture site is closed with an aseptic sticker. Complications: puncture of the subclavian artery, air embolism, puncture of the pleural cavity, damage to the brachial plexus, damage to the thoracic lymphatic duct, damage to the trachea, goiter and thyroid gland, suppuration at the puncture site. 3. Tracheostomy. Conicostomy Tracheostomy Indications: obstruction of the larynx and upper trachea due to obstruction by a tumor or foreign body, paralysis and spasm of the vocal cords, severe swelling of the larynx, acute respiratory distress, aspiration of vomit, prevention of asphyxia in severe chest injuries. Tools: 2 scalpels, 2 anatomical and surgical tweezers, several hemostatic clamps, an elevator, a grooved probe, 2 blunt and 1 single-toothed sharp hook, Trousseau or Deschamps dilator, surgical needles with a needle holder. Technique. The patient lies on his back, a roller under his shoulders, his head is thrown back. If the patient is in a state of asphyxia, the roller is placed only at the last moment, before opening the trachea. Local infiltration anesthesia is performed with a 0,5-1% solution of novocaine with the addition of adrenaline. In acute asphyxia, it is possible to operate without anesthesia. Identification points: the angle of the thyroid cartilage and the tubercle of the arch of the cricoid cartilage. An incision of the skin, subcutaneous tissue and superficial fascia is made from the lower edge of the thyroid cartilage to the jugular notch strictly along the midline of the neck. The median vein of the neck is retracted or ligated, finding a white line, along which the muscles are pushed apart in a blunt way and the isthmus of the thyroid gland is exposed. The edges of the incision are moved apart with a Trousseau dilator, ligatures are applied to the edge of the wound and the tracheostomy tube is carefully inserted, making sure that its end enters the lumen of the trachea. The surgical wound is sutured. The tube is fixed on the patient's neck with a gauze splint, previously tied to the tube shield. Insert the inner tube into the outer tube. Conicostomy The patient is placed on his back with a transverse roller at the level of the shoulder blades. The patient's head is tilted back. The larynx is fixed with fingers on the lateral surfaces of the thyroid cartilage and the gap between the thyroid and cricoid cartilage is felt, where the cone-shaped ligament is located. Under local infiltration anesthesia with a pointed scalpel, a transverse skin incision about 2 cm long is made, the cone-shaped ligament is felt for and dissected or perforated. Any tracheostomy cannula of suitable diameter is inserted into the hole formed and fixed with a gauze strip around the neck. In the absence of a cannula, it can be replaced by a piece of rubber or plastic tube of suitable diameter and length. To prevent this tube from slipping into the trachea, its outer end is pierced transversely at a distance of 2 cm from the edge and fixed with a gauze strip. Conicotome is a small diameter metal tracheostomy cannula with a piercing mandrel inside it. After dissection of the skin over the cone-shaped ligament, it is pierced with a conicotome, the mandrel is removed, and the cannula is placed in a position that ensures free flow of air into the trachea and fixed. 4. Tracheal intubation Indications: narrowing of the larynx, pathological breathing, acute respiratory failure, coma II and III degree, high risk of aspiration during surgical interventions on the organs of the chest and abdominal cavity, head and neck, in diseases of the pharynx, larynx and trachea (acute inflammation, cancer, tuberculosis and etc.). A laryngoscope is used for intubation. It consists of a handle and a blade. The most widely used curved blades, as they are more physiological. Straight blades are used with a long neck. Preparation for intubation includes checking equipment and positioning the patient correctly. The endotracheal tube should be checked. The cuff is tested by inflating it with a 10 ml syringe. Check the contact of the blade with the handle of the laryngoscope and the light bulb. It is necessary to ensure that the suction is ready in case of sudden sputum discharge, bleeding or vomiting. Successful intubation depends on the correct position of the patient. The patient's head should be at the level of the xiphoid process of the intubator. Moderate head elevation with simultaneous extension at the atlantooccipital joint creates an improved position for intubation. Preparation for intubation also includes mandatory pre-oxygenation. The laryngoscope is held in the non-dominant hand (for most people, this is the left), and the patient's mouth is opened wide with the other hand. The blade is inserted along the right side of the oropharynx, avoiding damage to the teeth. The tongue is shifted to the left, and the blade is raised up to the arch of the pharynx. The tip of a curved blade is inserted into the vallecula (a fossa located on the anterior surface of the epiglottis), while the tip of a straight blade should lift the epiglottis directly. The handle of the laryngoscope is pushed up and forward perpendicular to the mandible until the vocal cords come into view. Reliance on teeth should be avoided. The endotracheal tube is taken in the right hand and passed through the open glottis under visual control. The cuff should be positioned in the upper trachea, but below the larynx. The laryngoscope is removed from the mouth, again avoiding damage to the teeth. Immediately after intubation, auscultation is performed over the lungs on both sides (since it is possible to pass a tube into one bronchus) and in the epigastrium (to exclude esophageal intubation). If the tube is in the trachea, it is fixed in position with ribbons and the cuff is inflated. The cuff should be positioned above the level of the cricoid cartilage, as long standing in the larynx can lead to hoarseness in the postoperative period. Complications: intubation of the esophagus, bronchus, location of the cuff in the larynx, damage to the teeth, dislocation of the lower jaw, laryngospasm, reflex disorders (hypertension, tachycardia, increased intracranial pressure), respiratory tract injury, inflammation, etc. 5. Puncture and catheterization of the epidural space Indications: severe pain syndrome, surgical interventions, providing postoperative analgesia. The level of setting the epidural block depends on which organ needs to be anesthetized. Levels of the spinal column and "target organs" in epidural anesthesia
Instrumentation: needles for anesthesia, a special needle for puncturing the epidural space, a sample syringe, a catheter, a plug, filter balls, napkins, adhesive tape and sterile gloves. The position of the patient is sitting or lying on his side. In this case, the knees and chin should be brought as close to the chest as possible. Thus, maximum flexion of the spine is created, at which the angle between the spinous processes of adjacent vertebrae increases and the approach to the yellow ligament is facilitated. Under aseptic conditions and under local anesthesia with a 0,5% solution of novocaine, a puncture of the epidural space is performed. The needle is injected strictly perpendicularly, but with osteochondrosis, an angle of inclination is possible or during puncture in the mid-thoracic region. When the needle enters the thickness of the ligaments, the mandrin is removed from it and a syringe with liquid is attached. Further advancement of the needle is carried out slowly and smoothly with pressure on the syringe plunger. Due to the significant resistance of the ligaments, the liquid cannot leave the syringe. The syringe is disconnected and the catheter is inserted 5-7 cm, there should be no resistance. The needle is removed and the guidewire is fixed to the back with adhesive plaster, bringing it to the front surface of the chest. The plug with the filter is fixed to the conductor. An anesthetic is injected. After that, the level of skin anesthesia is determined. Complications: respiratory and hemodynamic disorders, intoxication, damage to the dura mater, neurological complications, periduritis. 6. Acute disturbances of consciousness Consciousness is the highest form of reflection of reality, which is a set of mental processes that allow a person to navigate in the world around him, time, his own personality, which ensures his behavior. Impairment of consciousness is the general name for disorders of the integral activity of the brain, expressed in a violation of the ability to adequately perceive, comprehend and respond to the environment, navigate it, remember current events, make speech contact, and perform arbitrary expedient behavioral acts. There are various options for the oppression of consciousness (stupor, stupor, coma of various depths), as well as acute confusion (delirious state or metabolic encephalopathy). The degree of impaired consciousness varies from mild confusion to coma, and there are no clear transitions between these states. In practice, the degree of impaired consciousness is determined by the patient's reaction to stimuli. Stupefaction is a form of impaired consciousness, characterized by lethargy, slowing down and difficulty in the course of mental processes, rapid exhaustion of attention, an increase in the threshold for the perception of external stimuli, but while maintaining limited verbal contact. Stupefaction is based on a violation of attention, i.e., the ability to select the necessary information and coordinate responses in such a way that the logical sequence of thoughts and actions is not violated. The most common causes of stupor are metabolic and toxic disorders, but sometimes it is also observed with focal lesions of the cortex, especially the right parietal lobe. In such patients, it is possible to achieve a monosyllabic answer or the implementation of the simplest instructions only after persistent appeals to it or additional stimulation. With further oppression of consciousness, the possibility of speech contact is lost and sopor develops. Sopor is a state of deep depression of consciousness with the loss of the possibility of contact with the patient, but the preservation of coordinated defensive reactions and the opening of the patient's eyes in response to pain, sound or other stimuli. The patient cannot be fully awakened even with the help of painful stimuli, he lies with his eyes closed. The reaction to verbal instructions is weak or completely absent, it is impossible to get a response word or sound from the patient. With further oppression of consciousness, a coma develops. Coma is an unconscious state characterized by insensitivity to external stimuli. This is a life-threatening state of depression of the functions of the central nervous system and disorders of the regulation of vital functions. Coma can be caused by many different metabolic disorders and structural damage. 7. Examination of a patient with a coma The plan of examination of the patient is as follows. 1. Assessment of the functional state of the respiratory and cardiovascular systems. 2. General clinical examinations, taking into account laboratory data, allowing to assess extracranial pathology. 3. Neurological examination. Laboratory studies: general clinical blood test (signs of a bacterial or viral infection); biochemical blood test: glucose, blood coagulation factors (clotting time, prothrombin, fibrinogen, APTT, antithrombin III, paracoagulation tests, platelet count), urea, creatinine, bilirubin, ALT, AST, osmolarity, electrolytes (K, Na, Mg , Ca); toxicological screening of blood, urine, gastric contents. Instrumental studies: radiography of the skull and cervical spine. Consultation of a neuropathologist (neurosurgeon) determines the further direction of the diagnostic search: computed or magnetic resonance imaging; EEG; ultrasound dopplerography. Lumbar puncture with analysis of cerebrospinal fluid is mandatory after: 1) consultation of an ophthalmologist and exclusion of signs of increased intracranial pressure - edema and elevation of the optic discs; 2) exclusion of signs of herniation of the brain. The following localizations of the herniation of the brain are distinguished. Diencephalic herniation, which occurs when the medial supratentorial localization is damaged and consists in the displacement of the diencephalon through the notch of the cerebellar tenon. This process calls: 1) Cheyne-Stokes breathing; 2) constriction of the pupils while maintaining their reaction to light; 3) paralysis of gaze up; 4) changes in mental status. The herniation of the medial parts of the temporal lobe, which occurs when the lateral supratentorial localization is affected, consists in the displacement of the medial parts of the temporal lobe through the notch of the cerebellar tenon. The resulting pressure on the structures of the midbrain is manifested by: 1) impaired consciousness; 2) an enlarged, non-reactive pupil on the side of the herniation, which is associated with compression of the III cranial nerve; 3) hemiparesis on the opposite side. The movements of the eyeballs are not always disturbed. Herniation of the tonsils of the cerebellum, which is caused by pressure pushing the lower part of the cerebellum through the foramen magnum, which leads to compression of the medulla oblongata. It causes: 1) impaired consciousness; 2) violations of the rhythm of breathing or apnea. 8. Treatment of coma Treatment should be as aggressive as possible and primarily aimed at ensuring adequate oxygenation and stabilization of central hemodynamics. If spontaneous breathing is maintained, humidified oxygen insufflation through a mask or nasal catheter is recommended. In the absence of spontaneous respiration or in the presence of pathological respiration, tracheal intubation is performed and the patient is transferred to artificial lung ventilation. With psychomotor agitation and reaction to mechanical ventilation, the use of sedatives (benzodiazepines, butyrophenones) is necessary. Stabilization of central hemodynamics is the normalization of blood pressure. In a hypertensive state, blood pressure must be reduced, but not more than 10% of the original per hour. A good effect is the use of sodium nitroprusside or magnesium sulfate. With hypotension, dopamine, dopamine, dobutrex and hormonal drugs are used. In the absence of anamnestic data and an unclear diagnosis, exjuvantibus therapy is performed (a positive response to drug exposure, on the one hand, gives the key to the diagnosis, on the other hand, it helps to buy time to avoid irreversible changes): 1) thiamine - 100 mg intravenously, subsequently - 100 mg intramuscularly (especially if there is a history of alcoholism, when determining high concentrations of ethanol in the blood); 2) glucose - a 40% solution of 60 ml intravenously (with an unknown level of glucose in plasma or at a level less than 3 mmol / l); 3) naloxone - 0,4-1,2 mg intravenously, fractionally, repeatedly, especially in the presence of "opiate signs" (traces of intravenous injections, narrow pupils, central respiratory disorders); 4) anexat (flumazenil) - 0,2 mg for 30 seconds, over the next minute, inject another 0,3 mg, over each next minute - 0,5 mg to a total dose of 3 mg. In the absence of an effect, it can be assumed that the coma is unlikely to be caused by benzodiazepine drugs; 5) in case of poisoning or overdose with a known drug or substance, an appropriate antidote should be administered (if there is a possibility of antidote therapy). The treatment is carried out: 1) control of convulsive syndrome; 2) maintenance of normothermia; 3) prevention of aspiration of gastric contents; 4) urological treatment; 5) decrease in intracranial pressure. 9. Cardiopulmonary resuscitation Cardiopulmonary resuscitation (CPR) is a complex of surgical and therapeutic measures performed in the absence of life-threatening injuries and aimed at restoring and supporting the function of the cardiorespiratory system. Indications for cardiopulmonary resuscitation: carried out in patients with no effective pulse on the carotid arteries or a thready, weak pulse, who are unconscious and (or) in the absence of effective respiratory movements. The most common cases of primary cardiac arrest, as well as primary respiratory failure. Contraindications: trauma incompatible with life, terminal stages of incurable diseases and biological death. Basic principles Primary efforts in CPR are aimed at: 1) chest compression; 2) blowing air into the lungs and ventilation; 3) preparation and administration of drugs; 4) installation and maintenance of intravenous access; 5) specialized activities (defibrillation, pacemaker installation, tracheal intubation). Thus, to complete the full scope of activities, 4 people and a team leader are needed. One person should be in charge of CPR. This person should integrate all available information and prioritize impact. He must monitor the ECG monitor, the use of drugs and ensure that the actions of other team members are corrected. He should be removed from the performance of procedures that detract from the leadership role. For more than 40 years, the Safar resuscitation alphabet has been used for CPR. In this complex, the sequence of actions of the resuscitator is sustained; according to their English name, they are indicated by the corresponding letters. A - Airway - ensuring airway patency. B - Breathing - artificial ventilation of the lungs (ALV) in an accessible way, for example, when breathing "mouth to mouth". C - Circulation - ensuring hemocirculation - indirect heart massage. D - Drugs - the introduction of drugs. E - Electrocardiography - ECG registration. F - Fibrilation - conducting, if necessary, electrical defibrillation (cardioversion). G - Gauging - evaluation of primary results. H - Hypothermy - head cooling. I - Intensive care - intensive care for post-resuscitation syndromes. 10. Ensuring the patency of the respiratory tract. IVL A - Airway - airway management The patient is placed horizontally on his back. The head is thrown back as much as possible. If a patient with reduced muscle tone lies on his back, his tongue may sink, as if packing the throat. At the same time, the epiglottis descends, further blocking the airways. Appear: sonorous breathing, then violations of the respiratory rhythm up to its complete stop. Such phenomena develop especially rapidly in patients who are unconscious. To prevent and eliminate the retraction of the tongue, the lower jaw should be brought forward and at the same time hyperextension in the occipito-cervical joint should be performed. To do this, with the pressure of the thumbs on the chin, the lower jaw of the patient is shifted down, and then with the fingers placed at the corners of the jaw, they push it forward, supplementing this technique with overextension of the head posteriorly (triple Safar technique). With the correct and timely conduct of these manipulations, the patency of the airways at the level of the pharynx is quickly restored. The cause of airway obstruction may be foreign bodies. They are quickly removed with any improvised materials (napkin). The patient's head should be turned to the side due to the danger of aspiration. The restoration of patency of the upper respiratory tract is facilitated by the use of various air ducts. The most expedient is the use of an S-shaped air duct. For its introduction, the patient's mouth is opened with crossed fingers II and I, and the tube is advanced to the root of the tongue so that its opening "slides" along the palate. Care must be taken to ensure that the air duct does not move during transport. If all the described procedures are not effective, then we can assume the presence of obturation of the airways in the underlying sections. In these cases, direct laryngoscopy and active aspiration of pathological secretion is required, followed by tracheal intubation for 10-15 seconds. It is advisable to perform conicotomy and tracheostomy. B - Breathing - artificial lung ventilation (ALV) in an accessible way The simplest and most effective method of artificial respiration during resuscitation is the mouth-to-mouth method. After 2-3 inflations of the lungs, the presence of a pulse on the carotid artery is determined, if it is not detected, then they proceed to artificial restoration of blood circulation. Manual ventilation is used using a self-expanding Ambu-type bag. When using a ventilator, the respiratory rate is 12-15 per minute, the inspiratory volume is 0,5-1,0 liters. In a hospital, tracheal intubation is performed and the patient is transferred to a ventilator. 11. Indirect cardiac massage C-Circulation - ensuring hemocirculation - chest compressions Closed heart massage is the simplest and most efficient way of emergency artificial circulatory support. Closed heart massage should be started immediately, as soon as the diagnosis of acute circulatory arrest is made, without clarifying its causes and mechanisms. In cases of ineffective heart contractions, one should not wait for a complete cardiac arrest or an independent restoration of adequate cardiac activity. Basic rules for closed heart massage. 1. The patient should be in a horizontal position on a solid base (floor or low couch) to prevent the possibility of displacement of his body under the strengthening of the massaging hands. 2. The zone of application of the force of the hands of the resuscitator is located on the lower third of the sternum, strictly along the midline; the resuscitator can be on either side of the patient. 3. For massage, one palm is placed on the other and pressure is applied to the sternum in the area located 3-4 transverse fingers above the place of attachment to the sternum of the xiphoid process; the hands of the massager, straightened at the elbow joints, are positioned so that only the wrist produces pressure. 4. Compression of the victim's chest is performed due to the gravity of the doctor's torso. The displacement of the sternum towards the spine (i.e., the depth of the deflection of the chest) should be 4-6 cm. 5. The duration of one chest compression is 0,5 s, the interval between individual compressions is 0,5-1 s. Rate of massage - 60 massage movements per minute. In intervals, the hands are not removed from the sternum, the fingers remain raised, the arms are fully extended at the elbow joints. When resuscitation is carried out by one person, after two quick injections of air into the lungs of the patient, 15 chest compressions are performed, i.e. the ratio "ventilation: massage" is 2: 15. If 2 persons are involved in resuscitation, then this ratio is 1: 5, i.e., there are 5 chest compressions per breath. A prerequisite for cardiac massage is the constant monitoring of its effectiveness. The criteria for the effectiveness of massage should be considered as follows. 1. Change in skin color: it becomes less pale, gray, cyanotic. 2. Constriction of the pupils, if they were dilated, with the appearance of a reaction to light. 3. The appearance of a pulse impulse on the carotid and femoral arteries, and sometimes on the radial artery. 4. Determination of blood pressure at the level of 60-70 mm Hg. Art. when measured at the shoulder. 5. Sometimes the appearance of independent respiratory movements. 12. The introduction of drugs. ECG registration D - Drugs - the introduction of drugs. In case of acute cessation of blood circulation, the introduction of agents that stimulate cardiac activity should begin as soon as possible, if necessary, be repeated during resuscitation. After the start of cardiac massage, 0,5-1 ml of adrenaline should be administered as soon as possible (intravenously or intratracheally). Its repeated introductions are possible after 2-5 minutes (up to 5-6 ml in total). With asystole, adrenaline tones the myocardium and helps "start" the heart, with ventricular fibrillation it contributes to the transition of small-wave fibrillation to large-wave, which greatly facilitates defibrillation. Adrenaline facilitates coronary blood flow and increases the contractility of the heart muscle. Instead of epinephrine, isodrin can be used, which is 3 times more effective than adrenaline in terms of the effectiveness of the effect on the myocardium. The initial dose is 1-2 ml by intravenous injection, and the next 1-2 ml in 250 ml of a 5% glucose solution. In conditions of impaired blood circulation, metabolic acidosis progressively increases, therefore, immediately after the infusion of adrenaline, a 4-5% solution of sodium bicarbonate is administered intravenously at the rate of 3 ml / kg of the patient's body weight. In the process of dying, the tone of the parasympathetic nervous system increases significantly, the brain is depleted, therefore, M-cholinolytics are used. With asystole and bradycardia, atropine is administered intravenously in a 0,1% solution - 0,5-1 ml, up to a maximum dose of 3-4 ml. To increase myocardial tone and reduce the effect of hyperkalemia, intravenous administration of 5 ml of a 10% solution of calcium chloride is recommended. Adrenaline, atropine and calcium chloride can be administered together in the same syringe. With severe tachycardia and especially with the development of fibrillation, the use of lidocaine at a dose of 60-80 mg is indicated, but since it is short-acting, it is infused at a rate of 2 mg / min. It is also indicated to use glucocorticoids, which, by increasing the sensitivity of adrenoreactive myocardial structures to catecholamines and normalizing the permeability of cell membranes, contribute to the restoration of adequate cardiac activity. E - Electrocardiography - ECG registration With the help of an ECG study, the nature of the violation of cardiac activity is determined. Most often it can be asystole - complete cessation of heart contractions, fibrillation - chaotic uncoordinated contraction of myocardial fibers with a frequency of 400-500 beats / min, in which cardiac output practically stops. Initially, large-wave fibrillation is noted, which, within 1-2 minutes, passes into small-wave fibrillation, followed by asystole. The presence of any rhythm on the ECG is better than the complete absence of electrical activity of the myocardium. Therefore, the key task of CPR is to stimulate the electrical activity of the myocardium and subsequently modify it into an effective (presence of a pulse) rhythm. 13. Electrical defibrillation F - Fibrilation - conducting, if necessary, electrical defibrillation (cardioversion) Cardiac fibrillation can be eliminated by the use of electrical defibrillation. It is necessary to apply electrodes tightly to the chest (in the anterolateral position, one electrode is located in the region of the apex of the heart, the second in the subclavian region to the right of the sternum), which increases the force of the discharge and, accordingly, the effectiveness of defibrillation. In a number of patients, the anteroposterior (apex of the heart - interscapular space) position of the electrodes is more effective. Do not apply electrodes over the overlays of the ECG monitor. It should be noted that electrical defibrillation is effective only when large-wave oscillations with an amplitude of 0,5 to 1 mV or more are recorded on the ECG. This kind of myocardial fibrillation indicates the safety of its energy resources and the possibility of restoring adequate cardiac activity. If the oscillations are low, arrhythmic and polymorphic, which is observed in severe myocardial hypoxia, then the possibility of restoring cardiac activity after defibrillation is minimal. In this case, with the help of heart massage, mechanical ventilation, intravenous administration of adrenaline, atropine, calcium chloride, it is necessary to achieve the transfer of fibrillation to large-wave, and only after that defibrillation should be performed. The first attempt at defibrillation is carried out with a discharge of 200 J, with subsequent attempts the charge is increased to 360 J. The electrodes must be moistened and firmly pressed against the surface of the chest. The most common errors during defibrillation, which cause the ineffectiveness of the latter, include the following. 1. Long interruptions in heart massage or complete absence of resuscitation during the preparation of the defibrillator for discharge. 2. Loose pressing or insufficient moistening of the electrodes. 3. Application of a discharge against the background of low-wave fibrillation without taking measures that increase the energy resources of the myocardium. 4. Applying a discharge of low or excessively high voltage. It should be noted that electrical defibrillation of the heart is an effective method for correcting such cardiac arrhythmias as paroxysmal ventricular tachycardia, atrial flutter, nodal and supraventricular tachycardia, atrial fibrillation. The indication for electrical defibrillation, at the prehospital stage, is most often paroxysmal ventricular tachycardia. A feature of defibrillation in these conditions is the presence of consciousness in the patient and the need to eliminate the reaction to pain when applying an electric discharge. 14. Intensive care of post-resuscitation syndromes I-Intensive care - intensive care for post-resuscitation syndromes 1. Correction of CBS and water-electrolyte balance. Often after CPR, metabolic alkalosis, hypokalemia, hypochloremia, and other electrolyte disorders develop. There is a shift in pH to an acidic or alkaline environment. The key to pH correction is adequate ventilation. The use of bicarbonate should be carried out under the control of the gas composition of the blood. As a rule, there is no need for the introduction of HCO3 with a rapid restoration of blood circulation and respiration. With a functioning heart, a pH level of ~ 7,15 is adequate for the functioning of the cardiovascular system. 2. Normalization of the antioxidant defense system. Intensive therapy includes a complex of antioxidant drugs with multidirectional action - mafusol, unitiol, vitamin C, multibiont, tocopherol, probucol, etc. 3. The use of antioxidants helps to reduce the intensity of metabolic processes and, consequently, reduce the need for oxygen and energy, as well as the maximum use of the reduced amount of oxygen that is available during hypoxia. This is achieved through the use of neurovegetative protection drugs and antihypoxants (seduxen, droperidol, ganglion blockers, mexamine, sodium hydroxybutyrate, cytochrome, gutimin, etc.). 4. An increase in energy resources is provided by intravenous administration of concentrated glucose solutions with insulin and the main coenzymes involved in energy utilization (vitamin B6, cocarboxylase, ATP, riboxin, etc.). 5. Stimulation of the synthesis of protein and nucleic acids - substrates that are absolutely necessary for the normal functioning of cells, the synthesis of enzymes, immunoglobulins and others, is carried out by the use of anabolic hormones (retabolil, nerabolil, insulin, retinol), folic acid, as well as the introduction of amino acid solutions. 6. Activation of aerobic metabolism is achieved by introducing a sufficient amount of oxidation substrates (glucose), as well as using hyperbolic oxygenation (HBO) - this method ensures the supply of the required amount of oxygen even in conditions of sharp violations of its delivery. 7. Improvement of redox processes (succinic acid, riboxin, tocopherol, etc.). 8. Active detoxification therapy contributes to the normalization of metabolic processes. For this, various methods of infusion therapy (gelatinol, albumin, plasma), forced diuresis, etc. are used. In severe cases, extracorporeal detoxification methods are used (hemosorption, hemodialysis, plasmapheresis). 9. Elimination of violations of microcirculation processes. For this, heparin therapy is performed. 15. Laryngospasm Laryngospasm is the closure of the true and false vocal cords. In both cases, control agents (eufillin) are necessarily used. If this does not help, it is necessary to introduce short-acting muscle relaxants, intubate and transfer the patient to mechanical ventilation. Muscle relaxants cause respiratory failure in the postoperative period if sufficient decurarization is not performed. It is usually produced by anticholinesterase drugs (prozerin). By the time of extubation, it is necessary to make sure that strength and muscle tone have recovered (ask to raise a hand, squeeze a hand, raise a head). With multiple fractures of the ribs, part of the chest sinks during inhalation, the so-called paradoxical breathing develops, so it is necessary to restore the chest frame. For this patient, it is necessary to intubate, after introducing relaxants, with further transfer to mechanical ventilation (until the integrity of the chest is restored). The following leads to a decrease in the functioning lung parenchyma: atelectasis, lung collapse, pneumonia, the consequences of surgery, pneumo-, hemo-, pyothorax. Differences between atelectasis and collapse: atelectasis is an obstruction in a straightened state. This condition is characterized by the presence of an unventilated lung through which half of the circulating blood passes, the latter is not oxygenated. As a result, acute respiratory failure develops. When the lung collapses, it is compressed by air or fluid in the pleural cavity. At the same time, the blood circulation in the compressed lung sharply decreases, and the blood circulation in the healthy lung increases. Therefore, collapse is not as dangerous a complication in terms of the development of acute respiratory failure as atelectasis. Before surgery, the function of the intact lung should be assessed (separate spirography). According to the stage of development, acute respiratory failure is divided into: 1) dysfunction; 2) insufficiency; 3) failure of prosthetic function. According to the rate of development, acute respiratory failure is divided into: 1) lightning fast (develops within a minute); 2) acute (develops within a few hours); 3) subacute (develops within a few days); 4) chronic (lasts for years). The main elements of intensive care for acute respiratory failure: oxygen therapy, drainage position of the patient, fibrobronchoscopy, tracheostomy, intubation and mechanical ventilation, bronchodilation, hormone therapy, HBO. 16. Pulmonary embolism Pulmonary embolism (PE) is a blockage of the main or middle trunk, small vascular trunks of the pulmonary artery, leading to an increase in pressure in the pulmonary circulation, right ventricular failure. Clinical classification of PE Form: heavy, medium and light. Downstream: fulminant, acute, recurrent. According to the level of damage to the pulmonary artery: trunk or main branches, lobar (segmental) branches, small branches. The clinical course of PE is quite variable. The most common symptoms are sudden onset of shortness of breath (RR ranges from 30 to more than 50 per minute), rapid breathing, pallor, more often cyanosis, swelling of the jugular veins, tachycardia, arterial hypotension (up to shock), retrosternal pain, cough and hemoptysis. Auscultation often determines the strengthening of the II tone over the pulmonary artery. X-ray signs - an increase in the size of the proximal pulmonary artery, depletion of the peripheral pattern, as well as raising the dome of the diaphragm. The ECG may reveal overload of the right departments (cor pulmonale): 1) the appearance of Q waves with a simultaneous increase in the amplitude of the R and S waves (QS syndrome); 2) rotation of the heart around the longitudinal axis with the right ventricle forward (shift of the transition zone to the left chest leads); 3) ST-segment elevation with negative wave in leads III, aUR, V1-V3; 4) the appearance or increase in the degree of blockade of the right leg of the bundle of His; 5) high pointed "pulmonary" tooth P with a deviation of its electrical axis to the right; 6) sinus tachycardia or tachysystolic form of atrial fibrillation. Echocardiography allows detecting acute cor pulmonale, determining the severity of hypertension in the pulmonary circulation, assessing the structural and functional state of the right ventricle, detecting thromboembolism in the heart cavities and in the main pulmonary arteries, visualizing an open foramen ovale, which can affect the severity of hemodynamic disorders and be the cause of paradoxical embolism . However, a negative echocardiographic result by no means rules out the diagnosis of pulmonary embolism. The most informative diagnostic method is pulmonary artery angiography. Treatment 1. Anticoagulant therapy. 2. Thrombolytic therapy. 3. Surgical treatment. 17. Emergency treatment of status asthmaticus Oxygen therapy. Moistened oxygen is inhaled2through nasal catheters or through a mask at a rate of 1-2 l / min. Adrenaline stimulatesα1-,β., - and β2-adrenergic receptors, dilates the bronchi and reduces airway resistance. Eufillin inhibits phosphodiesterase, which contributes to the accumulation of cyclic AMP and the removal of bronchospasm. When prescribing aminophylline, contraindications should be taken into account, which include smoking and childhood, heart failure and acute coronary syndrome, chronic diseases of the lungs, liver and kidneys. With AS, the loading dose of aminophylline is 3-6 mg/kg, it is administered intravenously over 20 minutes. Then carry out maintenance drip infusion of the drug. The effect of corticosteroid therapy is associated with the suppression of airway inflammation and increased sensitivity to β-adrenergic agents. The more severe the AS, the greater the indication for immediate corticosteroid therapy. A high dose of corticosteroids should be administered initially. If therapy is ineffective, the dose is increased. At least every 6 hours, appropriate equivalent doses of these drugs are administered. Most patients are shown inhalation therapy with b - adrenomimetics; (fenoterol, alupent, salbutamol). Exceptions are cases of drug overdose of sympathomimetics. If the ongoing therapy does not give an effect, intravenous administration of β-adrenergic agonists, such as isoproterenol, diluted in 5% glucose solution, is indicated. Contraindications are heart disease (coronary cardiosclerosis, myocardial infarction), severe tachycardia and symptoms of tachyphylaxis, old age. The rate of administration of isoproterenol is 0,1 μg / kg per 1 min until the onset of tachycardia (HR 130 per 1 min or more). Infusion therapy is the most important component of the treatment of AS, aimed at replenishing fluid deficiency and eliminating hypovolemia, the total volume of infusion therapy is 3-5 liters per day. Hydration is carried out by introducing solutions containing a sufficient amount of free water (glucose solutions), as well as hypo- and isotonic electrolyte solutions containing sodium and chlorine. Indicators of adequate hydration are the cessation of thirst, a wet tongue, the restoration of normal diuresis, improved sputum evacuation, and a decrease in hematocrit to 0,30-0,40. Halothane anesthesia can be used in the treatment of a severe asthma attack that is not amenable to conventional therapy. Artificial ventilation of the lungs. Indications for the transfer of patients with AS to mechanical ventilation should be very strict, since in this state it often causes complications and is characterized by high mortality. At the same time, mechanical ventilation, if it is carried out according to strict indications, is the only method that can prevent further progression of hypoxia and hypercapnia. 18. Myocardial infarction Myocardial infarction is a discrepancy between myocardial oxygen demand and its delivery, resulting in limited necrosis of the heart muscle. The most common cause is a thrombus, less often an embolus, less often a spasm of the coronary arteries. Thrombosis is most often observed against the background of atherosclerotic damage to the coronary arteries. Classically, myocardial infarction begins with increasing pain behind the sternum, which is burning and pressing in nature. Characterized by extensive irradiation of pain in the arms (usually in the left), back, abdomen, head, under the left shoulder blade, in the left lower jaw, etc. Patients are restless, anxious, sometimes they note a feeling of fear of death. There are signs of heart and vascular insufficiency - cold extremities, clammy sweat, etc. The pain syndrome is prolonged, and is not relieved by nitroglycerin for 30 minutes or more. There are various disorders of the heart rhythm, a drop in blood pressure or its rise. Patients subjectively note the feeling of lack of air. The above signs are typical for period I - painful or ischemic, the duration of which ranges from several hours to 2 days. Objectively, an increase in blood pressure (then a decrease); increased heart rate or rhythm disturbance; on auscultation, an abnormal IV tone is heard; heart sounds are muffled; on the aorta accent II tone; there are practically no biochemical changes in the blood, characteristic signs on the ECG. The second period is acute (feverish, inflammatory), characterized by the occurrence of necrosis of the heart muscle at the site of ischemia. The pain usually goes away. The duration of the acute period is up to 2 weeks. The patient's well-being gradually improves, but general weakness, malaise, and tachycardia persist. Heart sounds are muffled. The increase in body temperature caused by the inflammatory process in the myocardium, usually small, up to 38 ° C, usually appears on the 3rd day of the disease. By the end of the first week, the temperature usually returns to normal. The third period (subacute, or scarring) lasts 4-6 weeks. Characteristic for it is the normalization of blood parameters (enzymes), body temperature normalizes, all other signs of an acute process disappear: the ECG changes, a connective tissue scar develops at the site of necrosis. The fourth period (rehabilitation period, recovery) lasts from 6 months to 1 year. There are no clinical signs. During this period, compensatory hypertrophy of intact myocardial muscle fibers occurs, and other compensatory mechanisms develop. There is a gradual restoration of myocardial function. But the pathological Q wave persists on the ECG. Treatment is aimed at preventing complications, limiting the infarct zone, pain relief and correction of hypoxia. 19. Cardiogenic shock Cardiogenic shock is a critical circulatory disorder with arterial hypotension and signs of acute deterioration of blood circulation in organs and tissues. The main diagnostic sign is a significant decrease in systolic blood pressure, which is below 90 mm Hg. Art. The difference between systolic and diastolic pressure (pulse pressure) is 20 mm Hg. Art. or getting even smaller. In addition, a clinic of a sharp deterioration in the perfusion of organs and tissues is developing: 1) impaired consciousness from mild lethargy to psychosis or coma, focal neurological symptoms may appear; 2) diuresis less than 20 ml/h. Symptoms of deterioration of peripheral circulation: pale cyanotic, marbled, brick, moist skin; collapsed peripheral veins, a sharp decrease in the temperature of the skin of the hands and feet; decrease in blood flow. The value of the CVP can be different. Normal indicators of CVP are 5-8 cm of water. Art.; indicator below 5 cm of water. Art. indicates hypovolemia and low blood pressure, and above 8 cm of water. Art. indicates right ventricular failure. Treatment Oxygen therapy with humidified oxygen through a mask or nasal catheters is indicated. Painfully administered anticoagulants at a dose of 10 IU, followed by intravenous infusomat 000 IU per hour. It is necessary to administer analgesics: morphine 1000% 1 ml subcutaneously or intravenously by bolus; analgin 1,0% 50 ml intramuscularly, intravenously. Vascular tonics: Cordiamin 1-4 ml intravenously; mezaton 1% 1,0 g subcutaneously, intravenously, in saline; norepinephrine 0,2% 1,0 g intravenously. True cardiogenic shock is treated as follows. To increase the contractile activity of the myocardium, the following is used: strophanthin 0,05% 0,5-0,75 g intravenously slowly per 20,0 isotonic solution, korglucon 0,01 g intravenously, also in an isotonic solution or in a polarizing mixture, glucagon 2-4 mg intravenously drip on a polarizing solution. Normalization of blood pressure: norepinephrine 0,2% 2-4 ml per 1 liter of 5% glucose solution or isotonic solution. BP is maintained at 100 mm Hg. Art., mezaton 1% 1,0 g intravenously; cordiamine 2-4 ml, dopamine 200 mg in 400 ml of rheopolyglucin or 5% glucose. With an unstable effect from the above drugs, hydrocortisone 200 mg, prednisolone 90-120 mg are used. Normalization of rheological properties of blood. Elimination of hypovolemia, as there is sweating of the liquid part of the blood: reopoliglyukin, polyglukin - in a volume of up to 100 ml at a rate of 50,0 ml per minute. Correction of acid-base balance (fight against acidosis): sodium bicarbonate 5% to 200,0 ml. Re-introduction of painkillers. Restoration of rhythm and conduction disturbances. 20. Hypertensive crisis A hypertensive crisis is a sudden increase in blood pressure to a level that is usually not characteristic of this patient, leading to acute regional circulatory disorders and damage to target organs (heart, brain, kidneys, intestines). External factors provoking a crisis can be: 1) psycho-emotional stress; 2) meteorological influences; 3) excessive consumption of table salt. Clinical symptoms of a crisis are manifested by noise in the ears, flashing flies before the eyes, bursting headache in the occipital region, aggravated by bending over, straining, coughing, nausea, vomiting, heart rhythm disturbances. During a crisis, dangerous violations of the cerebral coronary, less often renal and abdominal circulation occur, which leads to stroke, myocardial infarction and other serious complications. ECG reveals left ventricular hypertrophy. Chest x-ray shows an enlarged heart, aortic deformity in the form of the number "3", usury of the ribs as a result of increased collateral blood flow through the intercostal arteries. Aortography confirms the diagnosis. The neurovegetative form of the crisis is characterized by a sudden onset, excitation, hyperemia and moisture of the skin, tachycardia, frequent profuse urination, a predominant increase in systolic pressure with an increase in pulse amplitude. Such crises are otherwise called adrenal, or type I crises. Type I crises usually have a relatively benign course, although they can lead to paroxysmal arrhythmias or angina pectoris, and in severe cases, myocardial infarction. With the water-salt form of the crisis, the condition worsens gradually, drowsiness, weakness, lethargy, disorientation, pallor and puffiness of the face, and swelling are noted. Systolic and diastolic pressure increase evenly or with a predominance of the latter and a decrease in pulse pressure. Such crises are called type II crises. Crises of type II, as a rule, are severe and can be complicated by myocardial infarction, stroke, acute left ventricular failure. It is necessary to highlight hypertensive crises that develop as a result of an abrupt cessation of permanent antihypertensive therapy, in particular, taking b-blockers, nifedipine, sympatholytics, and especially clonidine. Treatment of a hypertensive crisis consists in an urgent decrease in blood pressure to a normal level, necessary to prevent or limit damage to target organs in hypertension, to prevent complications up to death in the most severe cases, or permanent disability in the development of stroke, myocardial infarction. 21. Arrhythmia. Paroxysm of atrial fibrillation An arrhythmia is a heart rhythm other than sinus. Arrhythmia classification 1. Violation of the formation of impulses: 1) in the sinus node: a) sinus tachycardia; b) sinus bradycardia; c) sinus arrhythmia; d) sick sinus syndrome (SSS); 2) ectopic arrhythmias: a) extrasystole; b) paroxysmal tachycardia; c) atrial fibrillation and flutter; d) flicker and flutter of the ventricles. 2. Violation of impulse conduction: 1) additional pathways (Kent bundles); 2) heart block: a) atrial (intra-atrial); b) atrioventricular; c) intraventricular. Mechanisms of arrhythmias A decrease in the resting potential, the excitability threshold occurs only on the basis of a deficiency of cellular potassium, the ratio "plasma - cell" (normally 80 meq of potassium is in the cell and 5 meq in plasma). Asymmetry of the electrophysiological-metabolic focus of the myocardium due to ischemia, inflammation, reperfusion during thrombolysis. Electrophysiological weakness of the superior pacemaker. Congenital accessory conduction pathways. Paroxysmal supraventricular tachycardia is a sudden attack of heartbeat with a frequency of 150-250 beats per minute. There are 3 forms: 1) atrial; 2) nodal; 3) ventricular. The etiology of supraventricular paroxysmal tachycardia is more often associated with an increase in the activity of the sympathetic nervous system. It is clinically manifested by a sudden attack of the heartbeat, the vessels of the neck pulsate, cardiac activity switches to a different rhythm. The duration of the attack is from several minutes to several days. The number of heartbeats in the ventricular form is usually in the range of 150-180 beats per minute, with supraventricular forms - 180-240 beats per minute. During an attack, a pendulum-like rhythm is characteristic auscultatory, there is no difference between I and II tone. It increases myocardial oxygen demand and can provoke an attack of acute coronary insufficiency. ECG signs 1. QRS complexes are not changed. 2. In the supraventricular form, the P wave merges with T. 22. Ventricular extrasystole. AV conduction disorder Ventricular extrasystole is the occurrence of an extraordinary wide deformed QRS complex, discordant ST and T shift, a complete compensatory pause (the interval between the pre- and post-extrasystolic P wave is equal to twice the normal RR interval). The drug of choice is lidocaine, which is administered according to the above scheme. Perhaps the use of cordarone at a dose of 300-450 mg intravenously drip. Violation of AV conduction with the development of syncope (Morgagni-Adams-Stokes syndrome) When conduction is disturbed, various types of heart blocks occur, there is a slowdown or complete cessation of the conduction of the impulse through the conduction system of the heart. Sinoauricular blockade is characterized by dysfunction of T cells and impaired conduction of impulses from the sinus node to the atria. There are 3 degrees. I degree - slowing down the impulse. On the ECG - prolongation of the PQ interval for more than 0,20 s. Prolapse of the QRS complex. The RR interval is stable. II degree - loss of part of the impulses, incomplete conduction. Mobitz type I - as the impulses are carried out, the PQ interval gradually lengthens until the complete loss of the pulse wave. QRS is not changed. At the site of the QRS prolapse, the greatest distance is RR. Prognostically, this type is relatively favorable. Mobitz type II with a constant PQ interval and an unchanged QRS complex. At the same time, not all impulses reach the ventricles - in some cases, every second impulse is carried out, in others - every third, etc., i.e., there is a periodic prolapse of the QRS complex 3: 2, 4: 3, 5: 6, etc. d. III degree - complete blockade of conduction. At the same time, the conduction of impulses to the ventricles completely stops, in the ventricles their own heterotopic focus of idioventricular rhythm is born, and the lower the automatism, the more difficult the clinic. Complete dissociation is observed: the atrial rhythm is close to normal, and the ventricles have their own frequency - 40 beats per minute or less. The latter depends on the level of damage: if the AV node suffers, 40-50 beats per 1 minute, if the leg of the bundle of His - 20 beats per 1 minute or less. The level of damage is also indicated by the degree of deformation of the QRS complex. The heart sounds are weakened, periodically there is a "cannon" I tone, when the systole of the atria and ventricles almost coincide in time. May be III additional tone. Systolic ejection murmurs may appear at the base of the heart. Often a pulsation of the veins associated with atrial contraction is found, especially distinct with Strazhesko's cannon tone. Clinic Failing of the heart, if one impulse falls out. Vertigo if several impulses fall out. Morgagni-Adams-Stokes syndrome (loss of consciousness), if 6-8 complexes fall out. Treatment To restore an adequate rhythm, atropine is administered at a dose of 0,5-1 mg to 3 mg. Every 3 minutes, 1 mg to a total dose of 0,4 mg/kg. Calcium antagonists - isoptin 0,04 mg/kg. With frequent loss of consciousness, the patient is transferred to permanent electropulse therapy. But more often pacing has to be done "on demand". 23. Causes of acute renal failure Acute renal failure (ARF) is a complication of a number of renal and extrarenal diseases characterized by a sharp deterioration or cessation of kidney function and manifested by the following symptom complex: oligoanuria, azotemia, hyperhydration, impaired CBS and water and electrolyte balance. The forms of OOP include: 1) prerenal (hemodynamic); 2) renal (parenchymal); 3) postrenal (obstructive); 4) arenal. Reasons for the development of prerenal acute renal failure. 1. Decreased cardiac output (cardiogenic shock, paroxysmal arrhythmia, cardiac tamponade, pulmonary embolism, congestive heart failure). 2. Reduced vascular tone (sepsis, infectious-toxic shock, anaphylactic shock, overdose of antihypertensive drugs). 3. Decreased effective intravascular volume (blood loss, plasma loss, dehydration - loss of 7-10% of body weight). 4. Violation of intrarenal hemodynamics (taking NSAIDs, ACE inhibitors, radiopaque drugs, sandimmune). 5. Water poisoning - hyperhydration (uncontrolled production of ADH in malignant tumors, inflammatory diseases of the central nervous system, drug overdose - drugs, barbiturates, antidiabetic sulfanilamide drugs, indomethacin, amitriptyline, cyclophosphamide). Reasons for the development of renal acute renal failure. 1. Ischemia of the kidney. 2. Nephrotoxic damage due to exposure to: 1) drugs (aminoglycosides, NSAIDs, radiopaque drugs, etc.; 2) industrial nephrotoxins (heavy metal salts); 3) household nephrotoxins (ethylene glycol, methyl alcohol, dichloroethane, carbon tetrachloride). 3. Intratubular obstruction by pigments: 1) hemoglobin; 2) urates; 3) myoglobin; 4) inflammatory processes; 5) necrotic papillitis (diabetes mellitus, analgesic, alcoholic nephropathy); 6) vascular pathology. Reasons for the development of postrenal acute renal failure. 1. Pathology of the ureters: 1) obstruction; 2) compression. 2. Pathology of the bladder. 3. Urethral stricture. 24. Clinic and treatment of acute renal failure There are five stages in the clinical course of acute renal failure. Stage I of acute renal failure is initial, it lasts from the moment the etiological factor occurs until the first signs appear. At this stage, therapeutic tactics are aimed at eliminating or mitigating the impact of the etiological factor: anti-shock therapy, replenishing the BCC, combating heart failure, alkalizing therapy for intravascular hemolysis, combating pain, treating septic conditions, etc. Along with etiological therapy, spasm of kidney vessels is eliminated under the control of hourly diuresis. The earlier diuresis stimulation is started, the better the prognosis. Stage II of acute renal failure, or oligoanuric, is characterized by dysfunction of 70% of nephrons. Urine output less than 500 ml per day indicates the development of oliguria, and a decrease to 50 ml per day or lower indicates anuria. Along with impaired water excretion ability of the kidneys, concentration and nitrogen excretion functions also suffer. The amount of electrolytes and nitrogen in the urine sharply decreases. At this stage, the most pronounced changes in hemostasis occur. Treatment should be aimed at constancy of the internal environment in order to allow time and opportunity for the renal epithelium to regenerate. A state of hyperhydration develops due to the loss of electrolytes during vomiting and diarrhea. Therefore, it is necessary to stimulate diuresis, but only under the control of the CVP. Improve renal blood flow. Since it is necessary to carry out strict control of diuresis, bladder catheterization is performed. Violation of the nitrogen-excreting function of the kidneys leads to azotemia, therefore, to maximize the prevention of protein breakdown in the body, it is necessary to introduce a sufficient amount of carbohydrates. If the course is severe and not treatable, then hemodialysis sessions are performed. If the etiological factor is removed, then after 5-7 days of treatment, diuresis begins to increase. The maximum duration of this stage is up to 2 weeks. III stage of acute renal failure - early polyuric. It is characterized by a progressive increase in diuresis (by 200-300 ml per day) up to 3 liters. The nitrogen excretion and concentration functions of the kidneys have not yet fully recovered, but the concentration of potassium, magnesium, and phosphates is gradually normalizing. Intensive therapy in the early polyuric stage should include the same measures as in the previous one, except for the stimulation of diuresis. Often, hemodialysis is required. There is a high risk of dehydration. IV stage of acute renal failure - late polyuria. The daily increase in urine reaches 500-1000 ml, and diuresis can reach 8-10 liters per day or more. In the kidneys, ion exchange processes begin to recover. Losses of potassium, magnesium, phosphorus and other electrolytes sharply increase, patients are at risk of dehydration and demineralization. Therefore, electrolytes and fluid are given intravenously at this stage. Stage V OPN, or recovery stage. The concentration function of the kidneys is restored. Diuresis begins to gradually decrease to normal (2-3 liters per day) and urine density increases (1008-1028). 25. Acute liver failure Acute liver failure is a symptom complex characterized by a violation of one or more liver functions due to acute or chronic damage to its parenchyma. The clinical manifestations of ARF are as follows. 1. Coagulopathy is caused by a deficiency of coagulation factors and an increase in fibrinolytic activity. It predisposes to spontaneous bleeding from the mucous membranes: gastrointestinal, uterine, nasal bleeding can be observed. Brain hemorrhages are possible. To assess the state of the hemostasis system, prothrombin time is determined. 2. Hypoglycemia is characterized by a high level of insulin in plasma, which is due to a decrease in its uptake by the liver. It leads to a rapid deterioration of the neurological status and death of patients. 3. Violations of water-electrolyte and acid-base balance. End-stage acute renal failure is characterized by hyponatremia, hypophosphatemia, hypocalcemia, and hypomagnesemia. The change in the acid-base state does not have an unambiguous direction. Respiratory alkalosis associated with stimulation of the respiratory center with toxic substances may be replaced by respiratory acidosis due to increased intracranial pressure and suppression of respiratory activity. In the development of hepatic coma as a severe course of the disease, the stages of precoma, threatening coma and coma proper are distinguished. There are also hepatocellular (endogenous) coma, resulting from massive necrosis of the parenchyma, porto-caval (bypass, shunt, exogenous), due to a significant exclusion of the liver from metabolic processes due to the presence of pronounced porto-caval anastomoses, and mixed coma, occurring mainly in liver cirrhosis . In the precomatous period, progressive anorexia, nausea, a decrease in the size of the liver, an increase in jaundice, hyperbilirubinemia, and an increase in the content of bile acids in the blood develop. In the future, neuropsychic disorders, slowing of thinking, depression, and sometimes euphoria increase. Characterized by instability of mood, irritability, memory is disturbed, sleep is disturbed. Tendon reflexes increase, a small tremor of the limbs is characteristic. Azotemia develops. With timely therapy, patients can get out of this state, but more often with severe irreversible changes in the liver, coma occurs. During the period of coma, excitation is possible, which is then replaced by depression (stupor) and a progressive impairment of consciousness up to its complete loss. Meningeal phenomena, pathological reflexes, motor restlessness, convulsions develop. Breathing is disturbed (such as Kussmaul, Cheyne-Stokes); the pulse is small, arrhythmic; there is hypothermia. The patient's face is haggard, the extremities are cold, a characteristic sweet liver smell comes from the mouth and skin, hemorrhagic phenomena intensify (skin hemorrhages, bleeding from the nose, gums, varicose veins of the esophagus, etc.). 26. Treatment of acute liver failure Timely inotropic support is an essential component of intensive care. Prevention of infectious complications - the appointment of cephalosporin antibiotics in combination with antifungal drugs (amphotericin-B). Hepatoprotectors and membrane stabilizing drugs: prednisolone up to 300 mg, vitamin C 500 mg, troxevasin 5 ml, sodium etamsylate 750 mg, Essentiale 30 ml, tocopherol 4 ml intramuscularly, cytomak 35 mg, cocarboxylase 300 mg, nicotinic acid 30-40 mg, com-plamin 900 mg, sirepar 5-10 ml, glutamic acid 1% 400 ml, vikasol 10 ml intravenously, B vitamins. Protease inhibitors, which include cortri-cal 100 thousand units, trasylol 400 thousand units, antagonosan, go-dox. Stimulation of diuresis: reogluman 400 ml, mannitol, lasix up to 200 mg intravenously, eufillin 240 mg. To correct coagulopathy, intravenous administration of vitamin K (10 mg per day for 3 days) is used. The effect occurs after 3 hours. In this case, the elimination of hypoprothrombinemia associated with impaired absorption of vitamin K, resulting from a deficiency of bile acids. In case of bleeding or suspected invasive procedures (vascular catheterization, peritoneal dialysis), platelet mass or fresh frozen plasma is administered intravenously. Cerebral edema is a common cause of death. Mannitol is administered at the rate of 1 g/kg of body weight. In patients with renal insufficiency, mannitol is prescribed in combination with ultrafiltration to avoid hyperosmolarity and overhydration. With the development of hepatic coma, potassium chloride is prescribed (0,4-0,5% solution in a 5% glucose solution with a volume of 500 ml intravenously drip) or sodium bicarbonate solution (with metabolic acidosis); Patients breathe humidified oxygen through a nasal catheter. With a decrease in both arterial and venous pressure, polyglucin and albumin are administered intravenously. In the presence of massive bleeding, appropriate measures are taken to stop them, one-group blood is transfused, and drugs that contain blood clotting factors are administered. With significant signs of disseminated intravascular coagulation, heparin is administered intravenously at a dose of 10-000 IU bolus. In case of renal failure, peritoneal hemodialysis and plasmapheresis are performed, which give a good result, but before carrying out these manipulations, the introduction of heparin is contraindicated. To stop psychomotor agitation and seizures, diprazine, haloperidol, sodium oxybutyrate are prescribed. In severe cases, resort to intubation and mechanical ventilation. It is important to remember that the risk of bleeding is high, so all manipulations must be carried out with extreme caution. When removing the patient from a coma, the next step is to conduct intensive therapy for the underlying disease. 27. Shock Shock is a form of a critical state of the body, manifested by multiple organ dysfunction, developing in a cascade on the basis of a generalized circulation crisis and, as a rule, ending in death without treatment. A shock factor is any effect on the body that exceeds adaptive mechanisms in strength. In shock, the functions of respiration, the cardiovascular system, and kidneys change, the processes of microcirculation of organs and tissues and metabolic processes are disrupted. Shock is a disease of a polyetiological nature. Depending on the etiology of occurrence, the types of shock may be different. 1. Traumatic shock: 1) with mechanical injuries - bone fractures, wounds, compression of soft tissues, etc.; 2) with burn injuries (thermal and chemical burns); 3) under the influence of low temperature - cold shock; 4) in case of electrical injuries - electric shock. 2. Hemorrhagic or hypovolemic shock: 1) develops as a result of bleeding, acute blood loss; 2) as a result of an acute violation of the water balance, dehydration of the body occurs. 3. Septic (bacterial-toxic) shock (generalized purulent processes caused by gram-negative or gram-positive microflora). 4. Anaphylactic shock. 5. Cardiogenic shock (myocardial infarction, acute heart failure). Considered in the section emergency conditions in cardiology. In all types of shock, the main mechanism of development is vasodilation, and as a result, the capacity of the vascular bed increases, hypovolemia - the volume of circulating blood (BCC) decreases, since there are various factors: blood loss, redistribution of fluid between the blood and tissues, or a mismatch of the normal blood volume increasing vascular capacity. The resulting discrepancy between the BCC and the capacity of the vascular bed underlies the decrease in cardiac output and microcirculation disorders. The latter leads to serious changes in the body, since it is here that the main function of blood circulation is carried out - the exchange of substances and oxygen between the cell and the blood. There comes a thickening of the blood, an increase in its viscosity and intracapillary microthrombosis. Subsequently, cell functions are disrupted up to their death. In tissues, anaerobic processes begin to predominate over aerobic ones, which leads to the development of metabolic acidosis. Accumulation of metabolic products, mainly lactic acid, increases acidosis. 28. Anaphylactic shock Anaphylactic shock is a complex of various allergic reactions of an immediate type, reaching an extreme degree of severity. There are the following forms of anaphylactic shock: 1) cardiovascular form, in which acute circulatory failure develops, manifested by tachycardia, often with heart rhythm disturbances, ventricular and atrial fibrillation, and a decrease in blood pressure; 2) respiratory form, accompanied by acute respiratory failure: shortness of breath, cyanosis, stridor, bubbling breathing, moist rales in the lungs. This is due to a violation of capillary circulation, swelling of the lung tissue, larynx, epiglottis; 3) cerebral form due to hypoxia, impaired microcirculation and cerebral edema. According to the severity of the course, 4 degrees of anaphylactic shock are distinguished. I degree (mild) is characterized by itching of the skin, the appearance of a rash, headache, dizziness, a feeling of flushing to the head. II degree (moderate) - Quincke's edema, tachycardia, lowering of arterial pressure, increase of the Algover index join the previously indicated symptoms. Grade III (severe) is manifested by loss of consciousness, acute respiratory and cardiovascular failure (shortness of breath, cyanosis, stridor breathing, small rapid pulse, a sharp decrease in blood pressure, high Algover index). IV degree (extremely severe) is accompanied by loss of consciousness, severe cardiovascular insufficiency: the pulse is not determined, blood pressure is low. Treatment 1. Intravenous adrenaline infusion until hemodynamic stabilization. You can use dopmin 10-15 mcg / kg / min, and with symptoms of bronchospasm and b - adrenomimetics: alupent, brikanil drip intravenously. 2. Infusion therapy in a volume of 2500-3000 ml with the inclusion of polyglucin and rheopolyglucin, unless the reaction is caused by these drugs. Sodium bicarbonate 4% 400 ml, glucose solutions to restore bcc and hemodynamics. 3. Membrane stabilizers intravenously: prednisolone up to 600 mg, ascorbic acid 500 mg, troxevasin 5 ml, sodium etamsylate 750 mg, cytochrome C 30 mg (daily doses are indicated). 4. Bronchodilators: eufillin 240-480 mg, noshpa 2 ml, alupent (brikanil) 0,5 mg drip. 5. Antihistamines: diphenhydramine 40 mg (suprastin 60 mg, tavegil 6 ml), cimetidine 200-400 mg intravenously (daily doses are indicated). 6. Protease inhibitors: trasylol 400 thousand U, contrical 100 thousand U. 29. Traumatic shock Traumatic shock is a pathological and critical condition of the body that has arisen in response to an injury, in which the functions of vital systems and organs are impaired and inhibited. During trauma shock, torpid and erectile phases are distinguished. By the time of occurrence, shock can be primary (1-2 hours) and secondary (more than 2 hours after injury). Erectile stage or phase of occurrence. Consciousness remains, the patient is pale, restless, euphoric, inadequate, can scream, run somewhere, escape, etc. In this stage, adrenaline is released, due to which pressure and pulse can remain normal for some time. The duration of this phase is from several minutes and hours to several days. But in most cases it is short. The torpid phase replaces the erectile one, when the patient becomes lethargic and adynamic, blood pressure decreases and tachycardia appears. Estimates of the severity of injury are given in the table. Assessment of the extent of injury severity
After calculating the points, the resulting number is multiplied by a coefficient (from 1,2 to 2,0). Treatment. The main directions in treatment. 1. Elimination of the action of the traumatic agent. 2. Elimination of hypovolemia. 3. Elimination of hypoxia. 30. Hemorrhagic shock Hemorrhagic shock is a condition of acute cardiovascular insufficiency that develops after a significant amount of blood loss and leads to a decrease in perfusion of vital organs. Etiology: injuries with damage to large vessels, acute gastric and duodenal ulcers, rupture of an aortic aneurysm, hemorrhagic pancreatitis, rupture of the spleen or liver, rupture of the tube or ectopic pregnancy, the presence of placental lobules in the uterus, etc. According to clinical data and the magnitude of the deficiency of blood volume, the following degrees of severity are distinguished. 1. Not expressed - there are no clinical data, the level of blood pressure is normal. The volume of blood loss is up to 10% (500 ml). 2. Weak - minimal tachycardia, slight decrease in blood pressure, some signs of peripheral vasoconstriction (cold hands and feet). The volume of blood loss is from 15 to 25% (750-1200 ml). 3. Moderate - tachycardia up to 100-120 beats per minute, decrease in pulse pressure, systolic pressure 1-90 mm Hg. Art., anxiety, sweating, pallor, oliguria. The volume of blood loss is from 100 to 25% (35-1250 ml). 4. Severe - tachycardia more than 120 beats per minute, systolic pressure below 60 mm Hg. Art., often not determined by the tonometer, stupor, extreme pallor, cold extremities, anuria. The volume of blood loss is more than 35% (more than 1750 ml). Laboratory in the general analysis of blood, a decrease in the level of hemoglobin, erythrocytes and hematocrit. The ECG shows nonspecific changes in the ST segment and the T wave, which are due to insufficient coronary circulation. Treatment of hemorrhagic shock includes stopping bleeding, the use of infusion therapy to restore BCC, the use of vasoconstrictors or vasodilators, depending on the situation. Infusion therapy involves the intravenous administration of fluid and electrolytes in a volume of 4 liters (saline, glucose, albumin, polyglucin). In case of bleeding, transfusion of one-group blood and plasma is indicated in a total volume of at least 4 doses (1 dose is 250 ml). The introduction of hormonal drugs, such as membrane stabilizers (prednisolone 90-120 mg), is shown. Depending on the etiology, specific therapy is carried out. 31. Septic shock Septic shock is the penetration of an infectious agent from its original source into the blood system and its spread throughout the body. The causative agents can be: staphylococcal, streptococcal, pneumococcal, meningococcal and enterococcal bacteria, as well as Escherichia, Salmonella and Pseudomonas aeruginosa, etc. Septic shock is accompanied by dysfunction of the pulmonary, hepatic and renal systems, a violation of the blood coagulation system, which leads to the occurrence of thrombohemorrhagic syndrome (Machabeli syndrome), which develops in all cases of sepsis. The course of sepsis is influenced by the type of pathogen, this is especially important with modern methods of treatment. Laboratory findings indicate progressive anemia (due to hemolysis and inhibition of hematopoiesis). Leukocytosis up to 12 χ 109/l, however, in severe cases, as a sharp depression of the hematopoietic organs is formed, leukopenia can also be observed. Clinical symptoms of bacterial shock: chills, high fever, hypotension, dry warm skin - at first, and later - cold and wet, pallor, cyanosis, mental status disorder, vomiting, diarrhea, oliguria. Characterized by neutrophilia with a shift of the leukocyte formula to the left up to myelocytes; ESR increases to 30-60 mm/h or more. The level of blood bilirubin is increased (up to 35-85 µmol/l), which also applies to the content of residual nitrogen in the blood. Blood coagulation and prothrombin index are lowered (up to 50-70%), the content of calcium and chlorides is reduced. The total blood protein is reduced, which occurs due to albumin, and the level of globulins (alpha globulins and β - globulins) increases. In the urine, protein, leukocytes, erythrocytes and cylinders. The level of chlorides in the urine is reduced, and urea and uric acid are elevated. Treatment is primarily etiological in nature, therefore, before prescribing antibacterial therapy, it is necessary to determine the pathogen and its sensitivity to antibiotics. Antimicrobial agents should be used in maximum doses. To treat septic shock, it is necessary to use antibiotics that cover the entire spectrum of gram-negative microorganisms. The most rational is the combination of ceftazidime and impinem, which have proven effective against Pseudomonas aeruginosa. Drugs such as clindamycin, metronidazole, ticarcillin or imipinem are used as the drugs of choice when a resistant pathogen occurs. If staphylococci are cultured from the blood, it is imperative to begin treatment with penicillin drugs. Treatment of hypotension consists in the first stage of treatment in the adequacy of the volume of intravascular fluid. Use crystalloid solutions (isotonic sodium chloride solution, Ringerlactate) or colloids (albumin, dextran, polyvinylpyrrolidone). The advantage of colloids is that when they are introduced, the required filling pressures are achieved most quickly and remain so for a long time. If there is no effect, then inotropic support and (or) vasoactive drugs are used. 32. Methyl alcohol poisoning Methyl alcohol is absorbed by all routes - respiratory, digestive and transdermal. The lethal dose of methanol when taken orally ranges from 40-250 ml, but taking even 10-20 ml can cause blindness. Poisoning also occurs after taking various alcoholic mixtures containing from 1,5 to 2,5% methanol. Once absorbed, methanol is distributed throughout all tissues due to its water solubility. The largest amount accumulates in the kidneys and gastrointestinal tract, the smallest in the brain, muscles and adipose tissue. Pathological anatomical lesions include cerebral edema and damage to the initially inflammatory, and later dystrophic, nature of retinal ganglion cells. In some cases, in addition to damage to the nervous system, degenerative lesions of the liver, kidneys, lungs and heart muscle are found. In the toxic effect of methanol, two-phase action can be distinguished. In the initial period (phase I), methanol acts on the body as a whole molecule and has a predominantly narcotic effect, but weaker than that of ethyl alcohol. Subsequently (phase II), the harmful effect of oxidation products is manifested. In the clinical picture, periods are distinguished: intoxication, latent, or relative well-being (lasting from several hours to 1-2 days), the main manifestations of intoxication and, with a favorable outcome, reverse development. According to the severity, mild, moderate (or ophthalmic) and severe (or generalized) are distinguished. With mild poisoning, rapid fatigue, headache, nausea, and a state of slight intoxication are noted, which occur after a latent period of 30 minutes to several hours. The simultaneous absorption of ethyl and methyl alcohol increases the latent period and reduces the severity of poisoning. Treatment 1. Stopping the entry of poison into the body. Cessation of the use of poison, removal from the contaminated atmosphere, removal of poison from the skin. 2. Removal of non-absorbed poison (from the gastrointestinal tract): 1) probe gastric lavage; 2) the use of adsorbents or saline laxatives; 3) cleansing or siphon enema. 3. Removal of absorbed poison: 1) forcing diuresis; 2) methods of extracorporeal detoxification (hemosorption, hemodialysis, peritoneal dialysis, blood replacement surgery). 4. Antidote therapy, i.e. neutralization of the poison due to physical or chemical neutralization, as well as competition with the poison for application points. 5. Maintaining the vital functions of the body. 6. Normalization of the water-electrolyte, acid-base state of the body. 7. Treatment of long-term consequences and complications. 33. Ethyl alcohol and ethylene glycol poisoning When taking toxic doses - agitation, ataxia, stupor, coma with inhibition of reflexes, the smell of alcohol from the mouth, flushing of the face, conjunctivitis, "play" of the pupils, vomiting, involuntary urination, tachycardia, "hoarse" breathing, collapse, vomiting with possible aspiration of emetic wt. Treatment Gastric lavage through a thick probe, followed by the introduction of a saline laxative, siphon enema. Subcutaneously 1 ml of a 0,1% solution of atropine, 2 ml of cordiamine, 1 ml of a 20% solution of caffeine, with collapse - intramuscularly 1 ml of a 1% solution of mezaton. In the absence of pharyngeal reflexes - tracheal intubation and mechanical ventilation. Forcing diuresis with the simultaneous administration of a 4% sodium bicarbonate solution in a volume calculated according to the Astrup formula, hypertonic (10 and 20%) glucose solutions with insulin, B and C vitamins, cocarboxylase, nicotinic acid. With respiratory depression - slowly intravenously 3-5 ml of 1,5% solution of etimizol, 10 ml of 2,4% solution of aminophylline, 1 ml of 5% solution of ephedrine, oxygen inhalation. With aspiration - emergency sanitation bronchoscopy. Parenteral antibiotics. Ethylene glycol (antifreeze) poisoning The mean lethal dose is approximately 100 ml. It is rapidly absorbed in the digestive tract and distributed to all tissues, creating a maximum concentration in the brain. The main toxic effect is observed in the renal parenchyma, where necrosis of the tubular epithelium develops, interstitial edema, and foci of hemorrhagic necrosis in the cortical layer. Edema is found in the brain. In the clinic of intoxication, 3 periods are distinguished: 1) initial - lasting up to 12 hours, symptoms of CNS damage by the type of alcohol intoxication predominate; 2) neurotoxic - when the symptoms of CNS damage progress and respiratory and cardiovascular system disorders join; 3) nephrotoxic - on the 2nd-5th day, kidney damage predominates in the clinical picture of intoxication. Treatment Gastric lavage with water or 2% sodium bicarbonate solution, followed by the introduction of 30 g of magnesium sulfate in 200 ml of water. Inside 200 ml of a 30% solution of ethyl alcohol. 3-5 g of sodium bicarbonate in 100 ml of water. Plentiful drink. Intramuscularly 1-2 ml of cordiamine, 1 ml of a 20% caffeine solution. Intravenously 400 ml of 5% glucose solution with 5 ml of 5% ascorbic acid solution and 8 IU of insulin, glucosone-vocaine mixture, 400 ml of polyglucin, 400 ml of hemodez, 80-120 g of furosemide, 60-100 mg of prednisolone. 34. Dichloroethane poisoning The main routes of entry are the digestive tract, respiratory tract, and skin. The lethal dose of DCE for humans when administered orally is 10-20 ml. The toxic effect of DCE is due to the narcotic effect on the central nervous system, damage to the liver, kidneys, gastrointestinal tract, and a pronounced effect on the cardiovascular system. In the clinical picture, the leading symptoms are: toxic encephalopathy, acute toxic gastritis and gastroenteritis, impaired external respiration, toxic hepatitis, impaired renal function. In the first hours after administration, dizziness, ataxia, psychomotor agitation, clonic tonic convulsions, depression of consciousness, up to a coma appear. One of the early signs of poisoning are gastrointestinal disorders in the form of nausea, repeated vomiting with an admixture of bile. Violation of the function of external respiration often occurs according to the obstructive-aspiration type and is associated with increased salivation, bronchorrhea, and aspiration. Inhibition of the function of the respiratory center, the development of hypertonicity of the respiratory muscles and rigidity of the chest are noted. Treatment In case of poisoning with vapors - removal of the victim from the affected area, with respiratory depression IVL. If the poison gets inside - gastric lavage through a thick probe, followed by the introduction of 3-4 tablespoons of powdered activated carbon in 200 ml of water and 150-200 ml of vaseline oil, siphon enema. Intravenously 20-40 ml of 30% sodium thiosulfate solution, intramuscularly 5 ml of 5% unitiol solution. intravenously 400 ml of polyglucin, 400 ml of hemodez, 400 ml of 5% glucose solution, 80-120 mg of furosemide (lasix), 6-8 ml of 5% ascorbic acid solution. Intramuscularly 2 ml of cordiamine, with collapse - 1 ml of a 1% solution of mezaton, 1 ml of a 20% solution of caffeine, 100-150 mg of prednisolone. With an increase in hepatic-renal failure, specific therapy is carried out. Intravenous bolus 400 ml of polyglucin, 400 ml of hemodez, 400 ml of 5% glucose, 80-120 mg of furosemide, 6-8 ml of 5% ascorbic acid, 100-150 mg of prednisolone, for collapse 1 ml of 1% mesatone . Intramuscularly 2-4 ml of 6% thiamine bromide and 2-4 ml of 5% pyridoxine. For psychomotor agitation, 1 ml of 3% phenozepam solution. Inhalation of oxygen, in case of respiratory depression - mechanical ventilation through a breathing tube. During the first day, the most effective and sparing method is peritoneal dialysis. The composition of the standard dialysis solution includes: potassium chloride 0,3 g, sodium chloride 8,3 g, magnesium chloride 0,1 g, calcium chloride 0,3 g, glucose 6 g per 1 liter of water. At the same time, up to 2 liters of electrolyte solution with the addition of 500 thousand units of penicillin and 1000 units of heparin are injected into the patient's abdominal cavity. 35. Poisoning with mushroom poison and snake venom After a latent period lasting from 1-2 to 36 hours, cramping abdominal pain, salivation, nausea, indomitable vomiting, diarrhea, dehydration, collapse, delirium, hallucinations, convulsions appear. On the 2-3rd day - the phenomena of renal-hepatic insufficiency with anuria, azotemia, jaundice. In severe poisoning with lines and morels, hemolysis is possible. Treatment Gastric lavage through a thick tube, followed by the introduction of 3-4 tablespoons of powdered activated carbon in 200 ml of water and 30 g of magnesium sulfate (sodium) in 100 ml of water, siphon enema. Subcutaneously 1 ml of a 0,1% solution of atropine, 2 ml of cordiamine. In morel poisoning, atropine is not used as an antidote. Intravenously 400 ml of polyglucin, 400 ml of gemodez, 400 ml of 5% glucose solution with 4-6 ml of 5% ascorbic acid solution, 80-120 mg of furosemide (lasix). Intramuscularly 1-2 ml of a 6% solution of thiamine bromide and 2 ml of a 5% solution of pyridoxine hydrochloride (do not inject in one syringe). Relief of pain syndrome intramuscularly with the introduction of 1 ml of a 0,2% solution of platifillin, 2 ml of a 2% solution of papaverine. With convulsions, psychomotor agitation - intramuscularly 1-2 ml of a 3% solution of fenozepam or a lytic mixture (1-2 ml of a 2,5% solution of chlorpromazine, 1-2 ml of a 1% solution of diphenhydramine, 5-10 ml 25 % solution of magnesium sulfate) under the control of blood pressure. Forcing diuresis. In severe cases - hemosorption, early hemodialysis. Symptomatic therapy. Poisoning by snake venom Pain and rapidly spreading swelling at the site of the bite, drowsiness, respiratory depression, collapse, intravascular hemolysis with hemoglobinuria, severe subcutaneous hemorrhages, sometimes convulsions. Possibly kidney failure. With a cobra bite, local changes are less pronounced, bulbar disorders (speech and swallowing disorders, ptosis, paralysis of the motor muscles) and respiratory depression predominate. Treatment Suctioning blood and lymph from the wound (no later than 30-60 minutes after the bite) formed at the site of the bite using a blood-sucking jar. Rinsing the wound with a 1% solution of potassium permanganate. Injection into the wound of 0,3-0,5 ml of a 0,1% solution of adrenaline. If possible, urgent administration of specific mono- or polyvalent antisnake serum after preliminary intravenous administration of 100-150 ml of hydrocortisone or 50-100 ml of prednisolone. In case of cobra bites - intravenous Anticobra serum at a dose of 300 ml in combination with 1 ml of a 0,05% solution of prozerin and repeated administration every 30 minutes with 1 ml of a 0,1% solution of atropine. 36. Acid and arsenic poisoning Inhalation of vapors causes irritation of the eyes and upper respiratory tract (lacrimation, runny nose, cough, shortness of breath). Reflex respiratory arrest is possible. After a latent period (from 2 to 24 hours), toxic pneumonia or toxic pulmonary edema is formed. At hit in eyes, on skin - chemical burns. When ingested - a chemical burn of the oral cavity, pharynx, esophagus, stomach, possible swelling of the larynx with respiratory failure. Repeated vomiting with blood, peritoneal irritation, and occasionally perforation of the esophagus or stomach. Collapse, shock, hemorrhagic syndrome. Possible intravascular hemolysis, hemoglobinuric nephrosis with acute renal (renal-hepatic) insufficiency. Tubeless gastric lavage and artificial vomiting are dangerous due to the possibility of re-burning the esophagus and acid aspiration. Do not inject saline laxative and alkaline solutions. Treatment Gastric lavage through a thick probe with cold water after a preliminary intravenous or intramuscular injection of 1-2 ml of a 2% solution of promedol. Inside pieces of ice, Almagel A 15-20 ml every hour. Intravenously 800 ml of polyglucin, 400 ml of hemodez, glucosone-vocaine mixture (400 ml of 5% glucose solution with 25 ml of 2% novocaine solution), 50-150 mg of prednisolone or 150-250 mg of hydrocortisone, 10 thousand units of heparin, 80-120 mg furosemide (Lasix). Pain relief is achieved by intravenous injection of 1-2 ml of 0,005% fentanyl solution and 2-4 ml of 0,25% droperidol solution, for persistent abdominal pain - intramuscular injection of 1-2 ml of 0,2% platyphylline solution, 2 ml of 2% papaverine solution. Oxygen inhalation with antifoam agent. With increasing swelling of the larynx - intravenously 200-400 mg of prednisolone, 1-2 ml of a 1% solution of diphenhydramine, 10-20 ml of a 2,4% solution of aminophylline, 1-2 ml of a 5% solution of ephedrine. If there is no effect, tracheostomy, oxygen inhalation, and, if indicated, mechanical ventilation. Poisoning with arsenic and its compounds: a metallic taste in the mouth, abdominal pain, vomiting, loose stools, severe dehydration, convulsions, tachycardia, decreased blood pressure, coma, acute renal failure. Intravascular hemolysis and hemoglobinuria develop in arsenic hydrogen poisoning. Treatment Gastric lavage through a thick tube (2-3 times a day) with the introduction at the beginning and at the end of washing 50 ml of a 5% solution of unithiol, repeated siphon enemas with the addition of unithiol. Continuation of antidote therapy intravenously or intramuscularly with the introduction of a 5% solution of unitiol (up to 300 ml per day), intravenous drip of 20 ml of 10% calcium tetacine (ED1A) in 400 ml of a 5% glucose solution. 37. Poisoning with alkali, atropine, cannabis alkali poisoning When ingested, a chemical burn of the mucous membrane of the oral cavity, esophagus, and stomach develops. Pain along the esophagus and in the abdomen, vomiting with an admixture of blood, esophageal-gastric bleeding. Possible perforation of the esophagus, stomach with the development of mediastinitis, peritonitis. With a burn of the larynx - hoarseness of voice, aphonia, difficulty (stridor) breathing. In severe cases - burn shock, oliguria. Contact with skin causes chemical burns. Treat as in acid poisoning. Atropine poisoning Dry mouth, hoarseness, dry, hyperemic skin, dilated pupils, shortness of breath, palpitations, tachycardia, thirst, nausea, difficulty urinating. In severe poisoning - psychomotor agitation, delirium, hallucinations, convulsions, heart rhythm disturbances, coma, collapse are possible. Treatment If necessary - gastric lavage through a thick probe, richly lubricated with vaseline oil, the introduction of 3-4 tbsp. l. powdered activated carbon in 200 ml of water and 30 mg of magnesium sulfate in 100 ml of water. intravenously 2-4 ml of 0,05% proserin solution, 400-800 ml of 5% glucose solution, 40-80 mg of furosemide (lasix). Plentiful drink. Relief of psychomotor agitation and seizures intramuscularly by administering 1-2 ml of a 3% solution of phenozepam or a lytic mixture (2 ml of a 2,5% solution of aminazine, 2 ml of a 1% solution of diphenhydramine and 10 ml of a 25% solution of magnesium sulfate ) or 1-2 g of chloral hydrate in an enema with 1-2 g of starch per 25-50 ml of water, intravenously 10-15 ml of a 20% solution of sodium hydroxybutyrate, 2-4 ml of a 0,5% solution of seduxen. With severe tachycardia, extrasystole - intravenously anaprilin (1-2 ml of a 0,25% solution) or an anaprilin tablet (40 mg) under the tongue. With collapse - intravenously 1 ml of a 1% solution of mezaton in 10 ml of a 0,9% solution of sodium chloride. With a sharp hyperthermia - intramuscularly 2 ml of a 50% solution of analgin, ice packs on large vessels and the head, wet wraps. Hemp poisoning (hashish, marijuana, marijuana, plan) There is euphoria, psychomotor agitation, vivid visual hallucinations, dilated pupils, tinnitus. Subsequently, weakness, lethargy, depression of mood, drowsiness, bradycardia, hypothermia. Treatment In case of oral poisoning - gastric lavage through a thick probe, followed by the introduction of 3-4 tbsp. l. powdered activated carbon in 200 ml of water. Intravenously 400-800 ml of a 5% glucose solution with 5-10 ml of a 5% solution of ascorbic acid and 8-16 units of insulin, 40-80 mg of furosemide (lasix), intramuscularly 2 ml of a 6% solution of thiamine bromide. 38. Poisoning with cocaine, dicaine, narcotic analgesics cocaine poisoning Clinically manifested by general agitation, headache, flushing of the face, dilated pupils, tachycardia, increased respiration, increased blood pressure, hallucinations. In severe cases - convulsions, coma, respiratory paralysis, collapse. Repeated gastric lavage through a thick probe with a 0,1% solution of potassium permanganate, followed by the introduction of 3-4 tbsp. l. powdered activated carbon in 200 ml of water and 30 g of magnesium sulfate in 100 ml of water. Intravenously 400 ml of gemodez, 400 ml of 5% glucose solution with 5-10 ml of 5% ascorbic acid solution, 40-80 mg of furosemide (lasix). When excited - fixing the victim, intramuscularly 1-2 ml of a 3% solution of fenozepam or a lytic mixture (1-2 ml of a 2,5% solution of chlorpromazine, 2 ml of a 1% solution of diphenhydramine and 5-10 ml of 25% - a solution of magnesium sulfate) under the control of blood pressure. With convulsions, 1-2 g of chloral hydrate is administered in an enema with 1-2 g of starch in 25-50 ml of water, intravenously slowly 15-20 ml of a 20% sodium oxybutyrate solution, if there is no effect, slowly intramuscularly up to 20 ml of 2,5% solution of sodium thiopental or hexenal. With the development of a coma, an ice pack on the head, intravenously 40 ml of a 40% glucose solution with 4-6 ml of a 5% solution of ascorbic acid and 8 units of insulin, intravenously slowly or intramuscularly 2-4 ml of a 6% solution of thiamine bromide and 2-4 ml of a 5% solution of pyridoxine hydrochloride, 80-120 mg of furosemide. With severe respiratory depression, mechanical ventilation is carried out, intravenously slowly 2 ml of cordiamine, oxygen inhalation. Poisoning with narcotic analgesics (morphine, omnopon, droperidol) Drowsiness or unconsciousness, pupillary constriction, muscle hypertonicity (sometimes convulsions), respiratory depression, bradycardia, collapse. Respiratory paralysis is possible with the patient's consciousness preserved. Gastric lavage through a thick probe (while maintaining consciousness), followed by the introduction of 3-4 tbsp. l. powdered activated carbon and 30 g sodium sulfate, siphon enema. Intravenously 400 ml of gemodez, 400 ml of polyglucin, 400 ml of 5% glucose solution, 60-80 mg of furosemide (lasix). Subcutaneously 1-2 ml of a 0,1% solution of atropine, 1-2 ml of cordiamine, 1 ml of a 20% solution of caffeine. With the development of a coma, an ice pack on the head, intravenously 40 ml of a 40% glucose solution with 5-10 ml of a 5% solution of ascorbic acid and 8 units of insulin, intravenously slowly or intramuscularly 2-4 ml of a 6% solution of thiamine bromide and 2-4 ml of a 5% solution of pyridoxine hydrochloride, 80-120 mg of furosemide (lasix). If necessary - bladder catheterization and urine extraction. With respiratory depression - IVL, oxygen inhalation. Hemosorption (2-3 times a day until consciousness is restored). 39. Pain Pain is an unpleasant sensory and emotional state caused by real or potential pathological effects on tissues. In the CNS, pain is conducted along two main pathways. Specific path - the posterior horns of the spinal cord, specific nuclei of the thalamus, the cortex of the posterior central gyrus. This pathway is low-neuronal, fast, conducts threshold, emotionally uncolored, precisely localized pain (epicritic pain). Non-specific way - the posterior horns of the spinal cord, non-specific nuclei of the thalamus, the cortex of the frontal and parietal lobes diffusely. Conducts subthreshold, emotionally colored, poorly localized pain. It is slow, multineuronal, as it forms numerous collaterals to the medulla oblongata, the reticular formation, the limbic system, and the hippocampus. Subthreshold pain impulses undergo summation in the thalamus. Impulses conducted along the nonspecific pain pathway excite the emotional centers of the limbic system, the autonomic centers of the hypothalamus, and the medulla oblongata. Therefore, pain is accompanied by fear, painful experiences, increased breathing, pulse, rise in blood pressure, pupil dilation, dyspeptic disorders. The action of the nociceptive pain system is counteracted by the antinoceceptive system, the main neurons of which are localized in the periaqueductal gray matter (the aqueduct of Sylvius connects the III and IV ventricles). Their axons form descending pathways to the medulla oblongata and spinal cord and ascending pathways to the reticular formation, thalamus, hypothalamus, limbic system, basal ganglia, and cortex. The mediators of these neurons are pentapeptides: methenkephalin and leuenkephalin, which have methionine and leucine as terminal amino acids, respectively. Enkephalins excite opiate receptors. In enkephalinergic synapses, opiate receptors are located on the postsynaptic membrane, but the same membrane is presynaptic for other synapses. Opiate receptors are associated with adenylate cyclase and cause its inhibition by disrupting cAMP synthesis in neurons. As a result, calcium entry and release of mediators, including pain mediators - peptides decreases: substance P, cholecystokinin, somatostatin, glutamic acid. Opiate receptors are excited not only by mediators - enkephalins, but also by other components of the antinoceceptive system - brain hormones (endorphins). Peptide agonists of opiate receptors are formed during proteolysis of the peptide substances of the brain: proopiocortin, proenkephalins A and B. All these peptides are formed in the hypothalamus. Opiate receptors excite receptors in all brain structures involved in the conduction and perception of pain, the formation of emotionally colored reactions to pain. At the same time, the release of pain mediators decreases and all reactions accompanying pain are weakened. 40. Analgesic drugs An analgesic (acetylsalicylic acid, paracetamol, morphine) is a drug that reduces pain of various origins. Drugs that reduce pain provoked only by a certain causative factor, or eliminate a specific pain syndrome, for example, antacids, ergotamine (migraine), carbamazepine (neuralgia), nitroglycerin (angina pectoris), do not belong to classical analgesics. Corticosteroids suppress the inflammatory response and the resulting pain, but despite their widespread use for these purposes, they also do not represent classical analgesics. Analgesics are classified into narcotic, acting on CNS structures and causing drowsiness, such as opioids, and non-narcotic, acting mainly on peripheral structures, such as paracetamol, acetylsalicylic acid. Additional drugs that enhance the effect of analgesics The drugs of this group are not analgesics themselves, but are used in combination with analgesics for pain, as they can change the attitude towards pain, its perception and level anxiety, fear, depression (tricyclic antidepressants can even cause a decrease in the need for morphine in a patient in terminal state). Such drugs can be psychotropic drugs, as well as those that affect the mechanisms of pain, for example, eliminating spasm of smooth and striated muscles. Narcotic analgesics are herbal and synthetic drugs that selectively reduce the perception of pain, increase pain tolerance by reducing the emotional coloring of pain and its vegetative accompaniment, cause euphoria and drug dependence. Classification of narcotic analgesics and their antagonists 1. Piperidine-phenanthrene derivatives: 1) morphine; 2) codeine (methylmorphine, 5-7 times weaker than morphine as an analgesic); 3) ethylmorphine (dionine, equal in strength to morphine). 2. Phenylpiperidine derivatives: 1) promedol (3-4 times weaker than morphine); 2) fentanyl (100-400 times stronger than morphine). 3. Derivatives of diphenylmethane: 1) pyritramide (dipidolor) - equal to morphine; 2) tramadol (tramal) - somewhat inferior to morphine. 4. Agonists-antagonists: 1) opiate receptor agonists and opiate receptor antagonists - buprenorphine (norphine) (25-30 times stronger than morphine); 2) opiate receptor agonists and opiate receptor antagonists - pentazocine (lexir) (2-3 times weaker than morphine) and butorphanol (moradol) (equal to morphine). 41. Stages of anesthesia General anesthesia, or anesthesia, is a state of the body that is characterized by a temporary shutdown of a person’s consciousness, his pain sensitivity and reflexes, as well as relaxation of the muscles of the skeletal muscles, caused by the action of narcotic analgesics on the central nervous system. Depending on the routes of administration of narcotic substances into the body, inhalation and non-inhalation anesthesia are distinguished. There are 4 stages of anesthesia: 1) analgesia; 2) excitement; 3) surgical stage, subdivided into 4 levels; 4) stage of awakening. Stage of analgesia The patient is conscious, but some lethargy is noted, he is dozing, answers questions in monosyllables. Superficial and pain sensitivity are absent, but as for tactile and thermal sensitivity, they are preserved. In this stage, short-term surgical interventions are performed, such as opening phlegmon, abscesses, diagnostic studies, etc. The stage is short-term, lasting 3-4 minutes. Excitation stage At this stage, the centers of the cerebral cortex are inhibited, and the subcortical centers at this time are in a state of excitation. At the same time, the patient's consciousness is completely absent, pronounced motor and speech excitation is noted. Patients begin to scream, make attempts to get up from the operating table. Hyperemia of the skin is noted, the pulse becomes frequent, systolic blood pressure rises. The pupil of the eye becomes wide, but the reaction to light persists, lacrimation is noted. Often there is a cough, increased bronchial secretion, sometimes vomiting. Surgical intervention against the background of excitation cannot be performed. During this period, you should continue to saturate the body with a narcotic to enhance anesthesia. The duration of the stage depends on the general condition of the patient and the experience of the anesthesiologist. Typically, the duration of excitation is 7-15 minutes. Surgical stage With the onset of this stage of anesthesia, the patient calms down, breathing becomes calm and even, heart rate and blood pressure approach normal. During this period, surgical interventions are possible. Depending on the depth of anesthesia, 4 levels and stage III of anesthesia are distinguished. First level: the patient is calm, the number of respiratory movements, the number of heartbeats and blood pressure are approaching the initial values. The pupil gradually begins to narrow, its reaction to light is preserved. Second level: the movement of the eyeballs is stopped, they are fixed in a central position. The pupils dilate, and their reaction to light weakens. Muscle tone is reduced, which allows for abdominal operations. The third level is characterized as deep anesthesia. At the same time, the pupils of the eyes are dilated with a reaction to a strong light stimulus. Anesthesia at the fourth level is life-threatening for the patient, as respiratory and circulatory arrest may occur. Awakening stage As soon as the introduction of narcotic drugs stops, their concentration in the blood decreases, and the patient goes through all the stages of anesthesia in reverse order, awakening occurs. 42. Preparing the patient for anesthesia The anesthesiologist takes a direct and often the main role in preparing the patient for anesthesia and surgery. An obligatory moment is the examination of the patient before the operation, but at the same time, not only the underlying disease, for which surgery is to be performed, but also the presence of concomitant diseases, which the anesthesiologist asks in detail, is important. It is necessary to know how the patient was treated for these diseases, the effect of treatment, the duration of treatment, the presence of allergic reactions, the time of the last exacerbation. If the patient undergoes a surgical intervention in a planned manner, then, if necessary, correction of existing concomitant diseases is carried out. Sanitation of the oral cavity is important in the presence of loose and carious teeth, as they can be an additional and undesirable source of infection. The anesthesiologist finds out and evaluates the psychoneurological state of the patient. So, for example, in schizophrenia, the use of hallucinogenic drugs (ketamine) is contraindicated. Surgery during the period of psychosis is contraindicated. In the presence of a neurological deficit, it is preliminarily corrected. Allergic history is of great importance for the anesthesiologist; for this, intolerance to drugs, as well as food, household chemicals, etc. is specified. If the patient has an aggravated allergic anamnesis, not even to medications, during anesthesia, an allergic reaction up to anaphylactic shock may develop. Therefore, desensitizing agents (diphenhydramine, suprastin) are introduced into premedication in large quantities. An important point is the presence of a patient in the past operations and anesthesia. It turns out what the anesthesia was and whether there were any complications. Attention is drawn to the somatic condition of the patient: the shape of the face, the shape and type of the chest, the structure and length of the neck, the severity of subcutaneous fat, the presence of edema. All this is necessary in order to choose the right method of anesthesia and drugs. The first rule for preparing a patient for anesthesia during any operation and when using any anesthesia is the cleansing of the gastrointestinal tract (the stomach is washed through the tube, cleansing enemas are performed). To suppress the psycho-emotional reaction and suppress the activity of the vagus nerve, before surgery, the patient is given medication - premedication. At night, phenazepam is prescribed intramuscularly. Patients with a labile nervous system are prescribed tranquilizers (seduxen, relanium) a day before surgery. 40 minutes before surgery, narcotic analgesics are injected intramuscularly or subcutaneously: 1 ml of a 1-2% solution of promolol or 1 ml of pentozocine (lexir), 2 ml of fentanyl, or 1 ml of 1% morphine. To suppress the function of the vagus nerve and reduce salivation, 0,5 ml of a 0,1% solution of atropine is administered. 43. Intravenous and inhalation anesthesia The advantages of intravenous general anesthesia are the rapid introduction of the patient into anesthesia. With this type of anesthesia, there is no excitement, and the patient quickly falls asleep. But narcotic drugs that are used for intravenous administration create short-term anesthesia, so they cannot be used in their pure form as mononarcosis for long-term operations. Barbiturates - sodium thiopental and hexenal - are able to quickly induce narcotic sleep, while there is no stage of excitation, and awakening is fast. Clinical pictures of anesthesia conducted by sodium thiopental and hexenal are similar. Geksenal has a less inhibitory effect on the respiratory center. Freshly prepared solutions of barbituric acid derivatives are used. In surgery, anesthesia with barbiturates as mononarcosis is used for short-term operations that do not exceed 20 minutes in duration (for example, opening abscesses, phlegmon, reduction of dislocations, diagnostic manipulations, and repositioning of bone fragments). Derivatives of barbituric acid are also used for induction anesthesia. Sodium hydroxybutyrate is administered intravenously very slowly. The drug creates a superficial anesthesia, so it is often used in combination with other narcotic drugs, such as barbiturates - propanidide. It is often used for induction anesthesia. Ketamine can be used for mononarcosis and for induction anesthesia. The drug causes superficial sleep, stimulates the activity of the cardiovascular system (blood pressure rises, pulse quickens). Inhalation anesthesia is carried out with the help of easily evaporating (volatile) liquids - ether, halothane, methoxy-flurane (pentran), trichlorethylene, chloroform or gaseous narcotic substances - nitrous oxide, cyclopropane. With the endotracheal method of anesthesia, the narcotic substance enters the body from the anesthesia machine through a tube inserted into the trachea. The advantage of the method lies in the fact that it provides free patency of the respiratory tract and can be used in operations on the neck, face, head, eliminates the possibility of aspiration of vomit, blood; reduces the amount of drug used; improves gas exchange by reducing "dead" space. Endotracheal anesthesia is indicated for major surgical interventions, it is used as a multicomponent anesthesia with muscle relaxants (combined anesthesia). The total use of several drugs in small doses reduces the toxic effects on the body of each of them. Modern mixed anesthesia is used to provide analgesia, turn off consciousness, relaxation. Analgesia and switching off consciousness are carried out by using one or more narcotic substances - inhaled or non-inhaled. Anesthesia is carried out at the first level of the surgical stage. Muscle relaxation, or relaxation, is achieved by the fractional administration of muscle relaxants. 44. Stages of anesthesia There are three stages of anesthesia. 1. Introduction to anesthesia. Introductory anesthesia can be carried out with any narcotic substance, against which a rather deep anesthetic sleep occurs without a stage of excitation. Mostly, barbiturates, fentanyl in combination with sombrevin, and sombrevin were used. Sodium thiopental is also often used. The drugs are used in the form of a 1% solution, they are administered intravenously at a dose of 400-500 mg. Against the background of induction anesthesia, muscle relaxants are administered and tracheal intubation is performed. 2. Maintenance of anesthesia. To maintain general anesthesia, you can use any narcotic that can protect the body from surgical trauma (halothane, cyclopropane, nitrous oxide with oxygen), as well as neurolepta-nalgesia. Anesthesia is maintained at the first and second levels of the surgical stage, and muscle relaxants are administered to eliminate muscle tension, which cause myoplegia of all skeletal muscle groups, including respiratory ones. Therefore, the main condition for the modern combined method of anesthesia is mechanical ventilation, which is carried out by rhythmically squeezing a bag or fur, or using an artificial respiration apparatus. Recently, the most widespread neuroleptanalgesia. With this method, nitrous oxide with oxygen, fentanyl, droperidol, muscle relaxants are used for anesthesia. Introductory anesthesia intravenous. Anesthesia is maintained by inhalation of nitrous oxide with oxygen in a ratio of 2: 1, fractional intravenous administration of fentanyl and droperidol 1-2 ml every 15-20 minutes. With increased heart rate, fentanyl is administered, with an increase in blood pressure - droperidol. This type of anesthesia is safer for the patient. Fentanyl enhances pain relief, droperidol suppresses vegetative reactions. 3. Withdrawal from anesthesia. By the end of the operation, the anesthesiologist gradually stops the administration of narcotic substances and muscle relaxants. Consciousness returns to the patient, independent breathing and muscle tone are restored. The criteria for assessing the adequacy of spontaneous breathing are indicators of PO2, PCO2, and pH. After awakening, restoration of spontaneous breathing and skeletal muscle tone, the anesthesiologist can extubate the patient and transport him for further observation in the recovery room. During general anesthesia, the main parameters of hemodynamics are constantly determined and evaluated. Measure blood pressure, pulse rate every 10-15 minutes. In persons with diseases of the cardiovascular system, as well as during thoracic operations, it is necessary to constantly monitor the function of the heart muscle. Electroencephalographic observation can be used to determine the level of anesthesia. To control lung ventilation and metabolic changes during anesthesia and surgery, it is necessary to study the acid-base state (PO2, PCO2, pH, BE). 45. Complications of anesthesia Complications during anesthesia may occur due to improper anesthesia technique or the effect of anesthetics on vital organs. One such complication is vomiting. At the beginning of the introduction of anesthesia, vomiting may be associated with the nature of the dominant disease (pyloric stenosis, intestinal obstruction) or with the direct effect of the drug on the vomiting center. Against the background of vomiting, aspiration is dangerous - the entry of gastric contents into the trachea and bronchi. Gastric contents that have a pronounced acid reaction, falling on the vocal cords and then penetrating the trachea, can lead to laryngospasm or bronchospasm, resulting in respiratory failure with subsequent hypoxia - this is the so-called Mendelssohn's syndrome, accompanied by cyanosis, bronchospasm, tachycardia. Dangerous can be regurgitation - passive throwing of gastric contents into the trachea and bronchi. Complications from the respiratory system can occur due to impaired airway patency. This may be due to defects in the anesthesia machine. Complications of tracheal intubation performed by direct laryngoscopy can be grouped as follows: 1) damage to the teeth by the laryngoscope blade; 2) damage to the vocal cords; 3) introduction of an endotracheal tube into the esophagus; 4) introduction of an endotracheal tube into the right bronchus; 5) exit of the endotracheal tube from the trachea or bending it. Heart rhythm disturbances (ventricular tachycardia, extrasystole, ventricular fibrillation) can occur due to a number of reasons: 1) hypoxia and hypercapnia resulting from prolonged intubation or insufficient ventilation during anesthesia; 2) overdose of narcotic substances - barbiturates, halothane; 3) the use of adrenaline against the background of fluorotane, which increases the sensitivity of fluorotane to catecholamines. Peripheral nerve damage This complication occurs a day or more after anesthesia. Most often, the nerves of the upper and lower extremities and the brachial plexus are damaged. This is the result of an incorrect position of the patient on the operating table (arm abduction more than 90 from the body, arm behind the head, arm fixation to the arc of the operating table, laying the legs on the holders without padding). The correct position of the patient on the table eliminates the tension of the nerve trunks. Treatment is carried out by a neuropathologist and a physiotherapist. 46. Local anesthesia Surface anesthesia This type of anesthesia is carried out by contact of the anesthetic substance with one or another organ, its surface. For this purpose, a 1-3% solution of cocaine, 0,25-2% dicaine solution, 1-2% lidocaine solution, 1-5% trimecaine solution and 0,5-2% pyromecaine solution. Most local anesthetics bind to inactivated sodium channels, preventing their activation and sodium entry into the cell during membrane depolarization, thus achieving an analgesic effect. The technique of surface anesthesia is simple and consists in lubricating, instilling a solution or spraying it using special spray guns. The onset of action of the anesthetic is pH dependent, with low pH taking longer to take effect than at high pH. The duration of action of the anesthetic depends on the degree of its binding to proteins. This type of anesthesia is used in diagnostic manipulations and in ophthalmology, otorhinolaryngology. Regional anesthesia Regional anesthesia includes plexus, conduction, epidural, paravertebral and other types of anesthesia. Unlike general anesthesia, regional anesthesia provides adequate surgical analgesia due to peripheral blockade of pain impulses while maintaining normal vital functions. Regional anesthesia is technically difficult, and requires accurate knowledge of the anatomical and topographic location of the nerve plexus or nerve conductor, a clear orientation in permanent identification points (bone protrusions, arteries, muscles), the ability to assess tissue resistance and patient sensations. To turn off pain sensitivity, it is enough to introduce a 1% solution of trimecaine (lidocaine), and to turn off proprioceptive sensitivity and achieve muscle relaxation, you need to use more concentrated local anesthetic solutions (for example, trimecaine 2-2,5%). Restoration of sensitivity goes in the reverse order, i.e., first muscle tone and proprioceptive sensations appear, and then pain and temperature sensations. The effect of anesthesia depends on the amount of anesthetic penetrating transperineurally and causing an adequate threshold block. Doubling the concentration of the injected anesthetic prolongs anesthesia by 1/3, and the introduction of a double volume - only by 3-9%. Local anesthetics often lead to anaphylactic reactions. Trimecaine: duration of action is 1-1,5 hours, the maximum single dose is 800-1000 mg. Lidocaine (xicaine) is used in a 1-2% solution, the duration of anesthesia is up to 2,5-3 hours. Bupivocaine (marcaine) is used in a 0,5-0,75% solution in a maximum single dose of 150-170 mg , the duration of action is 8-12 hours. For the use of long-acting anesthetics, the addition of lidocaine clearly accelerates the onset of the effect, reducing the latent period. 47. Anesthesia of the cervical plexus (ASP) ACS, performed on one or both sides, allows you to perform all operations on the neck, thyroid gland, brachiocephalic vessels in case of gunshot wounds, injuries and tumor diseases. The cervical plexus (us cervicalis) is formed from the anterior branches of the four upper cervical nerves (C1-C4) as they emerge from the intervertebral foramina. It is located on the anterior surface of the middle scalene muscle and the muscle that lifts the scapula, lateral to the transverse processes of the cervical vertebrae. The motor nerves of the cervical plexus innervate the muscles of the neck, and the sensory nerves innervate the skin of the occipital region of the head, the anterior and lateral surfaces of the neck, the subclavian region to the level of I and II ribs and the auricle. The largest nerve of the cervical plexus is the phrenic (p. prenicus), which is formed from C3-C4 and less often due to an additional branch from C5. Most sensory nerves exit in the middle from under the posterior edge of the sternocleidomastoid muscle and diverge in the superficial layers of the neck, skin of the occipital region of the head and upper chest. Anesthesia technique 2 cm below the angle of the lower jaw, anterior to the sternocleidomastoid muscle, the pulsation of the internal carotid artery is determined. The horizontal branch of the hyoid bone corresponds to the level of the transverse process of the C3 vertebra. The needle injection point is located at the intersection of the line, which is a continuation of the horizontal branch of the hyoid bone, with the anterior edge of the sternocleidomastoid muscle. At this point of intersection, under aseptic conditions, a “lemon peel” is formed, and an injection needle is directed through it from the outside to the inside and from front to back, advancing it medially to the sternocleidomastoid muscle and behind the internal carotid artery (in the gap between the sternocleidomastoid muscle and palpable internal carotid artery) until the patient develops paresthesia or the needle hits the transverse process of the C3 vertebra. The depth of the injection does not exceed 2-5 cm. The needle is securely fixed in this position and an aspiration test is performed, determining whether the end of the needle is in the lumen of the vessel. For anesthesia, 10-12 ml of a 2% trimecaine solution is injected from both sides. To enhance the anesthesia of the cervical plexus, you can additionally block the superficial branches that go to the anterior surface of the neck. The place of their exit is the middle of the posterior edge of the sternocleidomastoid muscle. The needle is injected at the point of their exit under the superficial fascia of the neck. A solution of 2% trimecaine is administered in an amount of 3-5 ml cranially and caudally (fan-shaped). Adequate anesthesia occurs after 8-12 minutes and provides effective pain relief in most patients within 1,5-2 hours. 48. Anesthesia of the brachial plexus (APS) APS allows you to perform all operations on the upper limb, shoulder joint, shoulder, forearm and hand: amputations, surgical treatment of wounds with reposition and fixation of bone fragments, operations on blood vessels and nerves, reduction of shoulder dislocation, etc. High frequency of surgical interventions on the upper limb, especially in wartime, raises the question of rational methods of anesthesia during these operations. Brachial plexus anesthesia by Winnie The patient lies on his back, his head is turned in the opposite direction from the puncture site, the chin is brought to the contralateral shoulder girdle. The hand from the side of the puncture lies along the body, slightly pulled down. Landmarks: sternocleidomastoid muscle, scalenus anterior, interstitial space, external jugular vein, clavicle, cricoid cartilage. Anesthesia technique. The skin is treated with an antiseptic solution. Posterior to the sternocleidomastoid muscle, which clearly contours with a slight elevation of the head, at the level of the cricoid cartilage, place the fingertips of the left hand on the anterior scalene muscle. With further displacement of the fingers laterally by 0,5-1,5 cm, the interscalene space is felt between the anterior and middle scalene muscles. It becomes more pronounced with a deep breath, as the scalene muscles tense. In the depths of the interscalene space, the transverse processes of the cervical vertebrae are felt (a feeling of solid resistance), and with increased pressure with a fingertip, paresthesia in the shoulder or shoulder girdle is often caused; caudally in the interscalene space the subclavian artery can be palpated. The interscalene space in the upper section is crossed by the external jugular vein. The needle insertion point is in the upper part of the interscalene space at the level of the cricoid cartilage. At this point, a “lemon peel” is formed, and through it the needle is directed medially and slightly downward, from front to back (dorsally) to the transverse process of C6 at an angle of 30 to the sagittal plane. When the needle moves inward to a distance of 1,5-4 cm, paresthesia occurs, and the tip of the needle rests on the transverse process of the 6th cervical vertebra. In this position, the needle is fixed or pulled up by 1-2 mm, and after an aspiration test, 30-40 ml of a 2% solution of trimecaine (lidocaine) or a 0,5-0,75% solution of bupivocaine (marcaine) is injected. During the injection of the first milliliters of local anesthetic solution, the patient experiences short-term pain (“electric shock”), indicating the correct placement of the needle tip. In the absence of paresthesia, you can check the position of the needle tip by injecting 0,5 ml of 0,9% sodium chloride solution taken from the refrigerator. The appearance of a feeling of aching in the upper limb indicates contact of the cold solution with the nerve. 49. Anesthesia of peripheral nerves in the wrist area For operations on the hand, it is necessary to anesthetize the ulnar, median and radial nerves. In all cases, the needle is injected at the level of the proximal fold of the wrist. During anesthesia, the patient lies on his back, in the area of \uXNUMXb\uXNUMXbthe wrist, the arm is supinated and slightly bent. Landmarks: Ulna styloid, pisiform, flexor carpi ulnaris tendon, and flexor carpi longus tendon. Anesthesia of the ulnar nerve Technique for anesthesia of the palmar branch of the ulnar nerve. The needle insertion point is at the level of the proximal carpal crease medial to the flexor carpi ulnaris tendon. The needle is inserted to a depth of 1-2 cm through the subcutaneous tissue towards the pisiform bone. After the appearance of paresthesia and if the aspiration test is negative, fix the needle and inject 3-5 ml of a 2% trimecaine solution. In the absence of paresthesia, the needle is advanced until it comes into contact with the bone and when it is removed, tissue infiltration is carried out with a 2% trimecaine solution. Technique for anesthesia of the dorsal branch of the ulnar nerve. The point of injection of the needle is at the level of the intersection of the proximal fold of the wrist with the medial edge of the tendon of the ulnar flexor muscle of the hand. The needle is directed to the styloid process of the ulna. To obtain paresthesia, 3-5 ml of a 2% solution of trimecaine is injected. In the absence of paresthesia, the needle is removed, and 5-10 ml of a 2% trimecaine solution is infiltrated into the tissues. median nerve anesthesia Anesthesia technique. The needle injection point is located on the line of the proximal skin fold of the wrist between the tendon of the long palmar muscle and the radial flexor of the hand. After the needle is moved perpendicularly through the subcutaneous tissue to a depth of 0,5-1 cm and paresthesia is obtained, the needle is fixed and 3-5 ml of a 2% lidocaine solution is injected. If it is not possible to achieve paresthesia at a depth of 1 cm, the tissues are fan-shaped infiltrated with 5-10 ml of a 2% trimecaine solution while slowly withdrawing the needle. Anesthesia of the radial nerve Anesthesia technique. The point of injection is at the level of the proximal skin fold of the wrist lateral to the radial artery on the projection of the top of the "anatomical snuff box". An injection is made, and the needle is directed towards the "snuff box". When paresthesia appears, the needle is fixed, with a negative aspiration test, 3-5 ml of a 2% trimecaine solution is injected. In the absence of paresthesia, 5-10 ml of a 2% solution of trimecaine is fan-shapedly injected into the underlying tissues, creating an infiltration "bracelet" 3-3,5 cm long from the tendons of the short extensor and long abductor of the thumb on one side, to the long extensor of the thumb - with another. 50. Anesthesia of the lower extremities To perform surgical interventions on the lower limb, it is necessary to anesthetize all four major nerves. Three of them - the femoral, obturator and external cutaneous nerve of the thigh - originate from the lumbar plexus, and the sciatic nerve is formed partly from the lumbar and three branches of the sacral plexus. Anesthesia technique. The skin is treated with a disinfectant solution. A "lemon peel" is formed with an anesthetic solution, after which the needle is injected under the inguinal ligament 1-1,5 cm below the latter and 0,5-1 cm lateral to the palpated femoral artery. The needle is guided through the subcutaneous tissue somewhat in the proximal direction under the inguinal ligament, where at a depth of 3-4 cm after puncture of the fascia, the needle fails with loss of resistance and paresthesia may occur, extending to the anterior surface of the thigh. In this position, the needle is fixed with the thumb and forefinger of the left hand, and the edge of the palm of the left hand is pressed with force on the soft tissues of the thigh distal to the needle and 35-40 ml of a 1,5% trimecaine solution is injected. Pressure on soft tissues lasts 1,5-2 minutes. Thus, anesthesia of the femoral nerve with clamping turns into anesthesia of the lumbar plexus, performed from the anterior approach. The action of anesthesia lasts 2-2,5 hours. Anesthesia of the lumbar plexus can be performed posteriorly, while the femoral (L2-L4) and obturator nerves (L2-L3), genitofemoral nerve (L1-L2) and the lateral femoral cutaneous nerve (L2-L3) are anesthetized simultaneously. The position of the patient during anesthesia is on a healthy side with bent legs. Landmarks: spinous process of the 4th lumbar vertebra (line connecting the iliac crests behind); 3 cm caudal along the crests of the spinous processes from the spinous process of the 4th lumbar vertebra and 5 cm lateral from the last point. Anesthesia technique. From the spinous process of the 4th lumbar vertebra in the caudal direction, a line 3 cm long is drawn, from the end of which a perpendicular 5 cm long is laterally restored upward. The end point of the perpendicular, lying near the iliac crest, is the needle injection point. After creating a "lemon peel", a 12-15 cm long needle is inserted perpendicular to the skin until it contacts the transverse process of the 5th lumbar vertebra. Cranially, sliding off the transverse process of the 5th lumbar vertebra, the needle enters the thickness of the square psoas muscle. At the same time, resistance is felt to the introduction of a solution into it with a syringe (or springy resistance occurs with deformation of the air bubble in the syringe). The needle is passed to a depth where there is a feeling of "loss of resistance" (or the air bubble is not deformed). This test indicates that the needle is in the fascia between the quadrate psoas and psoas major. The needle is fixed at this depth and 35-40 ml of a 1,5-2% trimecaine (lidocaine) solution is injected to achieve anesthesia. 51. Anesthesia of the sciatic nerve Anesthesia of the sciatic nerve from the anterior approach Anesthesia technique. The patient lies on his back. The anterior superior iliac spine and the most protruding point of the greater trochanter of the femur are connected to each other by a straight line, and from the last point a perpendicular is restored to the anterior surface of the thigh. The length of the perpendicular is equal to the distance between the anterior superior iliac spine and the greater trochanter of the femur. The end of this perpendicular is the projection point. In the physiological position of the lower limb, after treating the skin with a disinfectant solution and creating a “lemon peel”, a 12-15 cm long needle is directed vertically down until it rests on the lesser trochanter of the femur. After the needle slips from the lesser trochanter, without changing the main direction, the needle is passed even deeper - 4-5 cm until paresthesia occurs. If it is not possible to achieve paresthesia, the needle is returned to the bone and, turning the limb inward by 7-10, the needle is advanced again until paresthesia appears in the patient. Anesthesia of the sciatic nerve from the posterior approach Anesthesia technique. The patient lies on his healthy side, the anesthetized limb is bent at the hip and knee joints at an angle of 45-60. From the most protruding part of the greater trochanter of the femur, a straight line is drawn to the posterior superior iliac spine, from the middle of which a perpendicular 4-5 cm long is lowered in the caudal direction. The end of the perpendicular serves as a projection point for the sciatic nerve. The needle is inserted at an angle of 90 to the frontal plane of the patient's body and advanced until paresthesia or contact with the bone is obtained. If necessary, the needle is pulled up and inserted approximately 0,5 cm lateral or medial to the initial injection. Obtaining paresthesia is mandatory. 20-25 ml of a 2% solution of lidocaine (trimecaine) is administered. The anesthesia technique will not change if the patient lies on his stomach. Anesthesia in the popliteal fossa Anesthesia technique. The upper corner of the rhomboid fossa is at the level of the upper edge of the patella. The injection point lies 1-1,5 cm below the upper angle on the bisector lowered from this angle, formed from the outside by the tendon of the biceps femoris, from the inside by the tendons of the semimembranosus and semitendinosus muscles of the thigh. The direction of movement of the needle is strictly vertical with the patient in the prone position until paresthesia of the tibial nerve is obtained. In the absence of paresthesia, the needle is directed fan-shaped, pulling it up each time to the level of subcutaneous tissue. After an aspiration test, 5-10 ml of a 2% solution of trimecaine is injected. To block the common peroneal nerve from the same point, the needle is directed laterally at an angle of 30-45 to the frontal plane. After receiving paresthesia, 5-10 ml of a 2% solution of trimecaine is injected. There are no complications or contraindications. 52. Complications of regional anesthesia During RA, complications occur quite rarely, and they can be divided into two groups. 1. Specific, which are more related to the technical errors of the methodology: 1) erroneous injection of a local anesthetic into the spinal canal or epidural space, intravenously or intra-arterially (with anesthesia of the cervical plexus, anesthesia of the lumbar plexus with inguinal access); 2) puncture of cavities and organs (pleural cavity, lung); 3) the formation of a hematoma with a neglect of puncture and damage to a large vessel; hematoma compresses the surrounding tissue or neurovascular bundle; 4) prolonged and severe hypotension that occurs with rapid resorption of the local anesthetic; 5) trauma to the nerve plexus or conductor with the end of the injection needle during rough manipulation; 6) the absence of an analgesic effect after plexus or conduction anesthesia. 2. Nonspecific, manifested mainly by general and local reactions of the body to the action of a local anesthetic in the form of toxic and allergic reactions. Non-specific complications may develop depending on the time, dose and site of administration of the anesthetic. In this case, lesions of the central nervous or cardiovascular systems predominate. Complications from the CNS can be mild (limited only to central excitation) or severe, which is manifested by CNS inhibition with possible total paralysis. The nature of non-specific complications: 1) an overdose of anesthetic with the simultaneous administration of a large dose (more than 1 g) of trimecaine or lidocaine intraarterially or intravenously; 2) allergic reactions to the introduction of a local anesthetic, characterized by a symptom complex of disorders of the central nervous and cardiovascular systems: anxiety, impaired consciousness, speech disorders, muscle twitches, convulsions, deep breathing, heart rhythm disturbance, QR expansion, lowering blood pressure, tachycardia , apnea, asystole; 3) infectious complications due to poor-quality processing of the surgical field at the site of anesthesia; 4) the development of hypotension with plexus and conduction anesthesia is much less common than with epidural and spinal anesthesia; 5) with the introduction of concentrated solutions of local anesthetics in a small percentage of cases, the development of bradycardia is noted. 53. Lumbar anesthesia Blockade according to Vishnevsky This type of anesthesia is achieved by injecting an anesthetic into the spinal canal. The technique of lumbar puncture is described in lecture No. 2. The peculiarities are that the puncture level is higher (T12-1_1, L1-L2) and after removing the mandrel from the needle, an anesthetic is immediately injected. The volume of anesthetic is 3-5 ml. Naropin is administered in 0,5% concentration, lidocaine - in 2%, marcaine - in 0,5%. The duration of anesthesia is 4-6 hours. This type of anesthesia also causes severe hypotension. At a high level of anesthesia (T12-L1), respiratory failure is possible. The most common complication is headache. Cervical vagosympathetic blockade according to A. V. Vishnevsky The patient is placed on the table on his back so that the hand on the side of the proposed blockade hangs over the edge of the table. The sternocleidomastoid muscle should be relaxed. A roller is placed under the shoulder girdle, the head is retracted in the opposite direction; in this position, the anatomical contours of the neck are well outlined. The field is treated with lubrication with alcohol and iodine. The doctor stands on the side of the blockade of the same name. The injection site is the angle formed by the intersection of the posterior edge of the sternocleidomastoid muscle with a vein. The index finger of the left hand is placed at the posterior edge of the sternocleidomastoid muscle, above the place where it crosses with the external jugular vein. Strongly pressing a finger on this place, they try to move the neurovascular bundle to the midline. In this case, the finger easily feels the anterior surface of the cervical vertebrae. The injection of the needle and its advancement should be done slowly, upward and inwards, all the while focusing on the anterior surface of the spine. The needle moves along the course of a 2% solution of novocaine sent in small portions (3-0,25 cm), which ensures the safety of the injection. The syringe during the injection is repeatedly removed from the needle for the purpose of control. Having brought the needle to the vertebra, they feel how it rests against it. Then the pressure on the needle is weakened, due to which it moves away by 1-2 mm, after which 40 to 60 ml of a solution is injected, which, spreading in a creeping infiltrate along the prevertebral aponeurosis, covers the vagus, sympathetic, and often phrenic nerves, interrupting ( blocking) the transmission of irritations from the pleuropulmonary region. The effectiveness of vagosympathetic blockade is evidenced by the appearance of Horner's symptom (narrowing of the pupil, narrowing of the palpebral fissure and retraction of the eyeball). The respiratory rhythm and pulse become less frequent, shortness of breath and cyanosis decrease, and the general condition improves. To avoid getting the needle into the vessels of the neck, the sternocleidomastoid muscle with the underlying neurovascular bundle should be moved strongly enough with the index finger to the midline. It is important to direct the needle up and inward, since moving it in a horizontal direction threatens to introduce a solution under the prevertebral aponeurosis and subsequent complication in the form of a pain syndrome that does not stop during the day. 54. Assessment of the severity of the patient Assessment of the somatic condition of the patient. 1 point - patients whose disease is localized and, as a rule, does not cause systemic disorders, i.e. practically healthy people. 2 points - this includes patients with unexpressed disorders that moderately disrupt the vital activity of the body without pronounced shifts in homeostasis. 3 points - patients with vital systemic disorders that significantly disrupt the functioning of the body, but do not lead to disability. 4 points - patients with severe systemic disorders that pose a high danger to human life and lead to disability. 5 points - patients whose condition is considered critical, the risk of death within 24 hours is high. The volume and nature of the surgical intervention: 1 point - small operations for: removal of superficially located and localized tumors, opening of small abscesses, amputation of fingers and toes, ligation and removal of hemorrhoids, uncomplicated appendectomy and herniotomy. 2 points - operations of moderate severity: removal of superficially located malignant tumors requiring extended intervention; opening of abscesses localized in cavities; amputation and disarticulation of the upper and lower extremities; operations on peripheral vessels; complicated appendectomy and herniotomy requiring extensive intervention; trial thoracotomy and laparotomy; others similar in complexity and scope of intervention. 3 points - extensive surgical interventions: radical operations on the abdominal organs (except those listed above); radical operations on the organs of the chest cavity. extended limb amputations, such as transiliosacral amputation; brain surgery. 4 points - operations on the heart, large vessels and other complex interventions performed under special conditions (artificial circulation, hypothermia, etc.). Classification of the objective status of the patient, developed by the American Society of Anesthesiologists (ASA). 1. There are no systemic disorders. 2. Mild systemic disorders without functional impairment. 3. Moderate and severe systemic diseases with dysfunction. 4. Severe systemic disease that constantly poses a threat to life and leads to failure of functions. 5. Terminal state, high risk of death during the day, regardless of the operation. 6. Brain death, organ donation for transplantation. 55. Artificial lung ventilation Artificial lung ventilation (ALV) provides gas exchange between the surrounding air (or a certain mixture of gases) and the alveoli of the lungs, is used as a means of resuscitation in the event of a sudden cessation of breathing, as a component of anesthesia and as a means of intensive care for acute respiratory failure, as well as some diseases of the nervous and muscular systems. Modern methods of artificial pulmonary ventilation (ALV) can be divided into simple and hardware. A simple method of mechanical ventilation is usually used in emergency situations (apnea, pathological rhythm, agonal breathing, increasing hypoxemia and (or) hypercapnia and gross metabolic disorders). The simplest are expiratory methods of mechanical ventilation (artificial respiration) from mouth to mouth and from mouth to nose. Hardware methods are used when long-term mechanical ventilation is necessary (from one hour to several months and even years). The Phase-50 respirator has great capabilities. The Vita-1 device is produced for pediatric practice. The respirator is connected to the patient's respiratory tract through an endotracheal tube or tracheostomy cannula. Hardware ventilation is carried out in normal frequency mode, which ranges from 12 to 20 cycles per minute. In practice, there are high-frequency ventilations (more than 1 cycles per minute), in which tidal volume is significantly reduced (to 60 ml or less), positive pressure in the lungs at the end of inspiration is reduced, as well as intrathoracic pressure, and blood flow to the heart is improved. Also, with the high-frequency mode, the patient’s adaptation (adaptation) to the respirator is facilitated. There are three methods of high-frequency ventilation: volumetric, oscillatory and jet. Volume is usually carried out with a respiratory rate of 80-100 per 1 min, oscillatory IVL - 600-3600 per 1 min, which ensures the vibration of a continuous or intermittent gas flow. The most widespread jet high-frequency ventilation with a respiratory rate of 100-300 per minute, in which a jet of oxygen at a pressure of 1-2 atm is blown into the airways through a needle or catheter with a diameter of 2-4 mm. Auxiliary ventilation is also carried out, but in this case the patient’s spontaneous breathing is maintained. Gas is supplied after the patient makes a weak attempt to inhale, or the patient is synchronized to an individually selected mode of operation of the device. There is also a mode of intermittent mandatory ventilation (PPVL), which is used in the process of gradual transition from artificial ventilation to spontaneous breathing. In this case, the patient breathes on his own, but additionally a continuous flow of gas mixture is supplied into the respiratory tract. Against this background, with a set frequency (from 10 to 1 time per minute), the device performs artificial inhalation, coinciding (synchronized PPVL) or not coinciding (unsynchronized PPVL) with the patient’s spontaneous inhalation. A gradual reduction in artificial breaths prepares the patient for independent breathing. 56. Infusion therapy Infusion therapy is a drip injection or infusion intravenously or under the skin of drugs and biological fluids in order to normalize the water-electrolyte, acid-base balance of the body, as well as for forced diuresis (in combination with diuretics). Indications for infusion therapy: all types of shock, blood loss, hypovolemia, loss of fluid, electrolytes and proteins as a result of indomitable vomiting, intense diarrhea, refusal to take fluids, burns, kidney disease; violations of the content of basic ions (sodium, potassium, chlorine, etc.), acidosis, alkalosis and poisoning. Crystalloid solutions are able to compensate for the deficiency of water and electrolytes. Apply 0,85% sodium chloride solution, Ringer and Ringer-Locke solutions, 5% sodium chloride solution, 5-40% glucose solutions and other solutions. They are administered intravenously and subcutaneously, by stream (with severe dehydration) and drip, in a volume of 10-50 ml/kg or more. The goals of infusion therapy are: restoration of BCC, elimination of hypovolemia, ensuring adequate cardiac output, maintaining and restoring normal plasma osmolarity, ensuring adequate microcirculation, preventing aggregation of blood cells, normalizing the oxygen transport function of blood. Colloidal solutions are solutions of macromolecular substances. They contribute to the retention of fluid in the vascular bed. Hemodez, polyglucin, reopoliglyukin, reogluman are used. With their introduction, complications are possible, which manifest themselves in the form of an allergic or pyrogenic reaction. Routes of administration - intravenously, less often subcutaneously and drip. The daily dose does not exceed 30-40 ml/kg. They have a detoxifying quality. As a source of parenteral nutrition, they are used in case of prolonged refusal to eat or inability to feed by mouth. Dextrans are colloidal plasma substitutes, which makes them highly effective in the rapid recovery of BCC. Dextrans have specific protective properties against ischemic diseases and reperfusion, the risk of which is always present during major surgical interventions. Fresh frozen plasma is a product taken from a single donor. FFP is separated from whole blood and frozen immediately within 6 hours of blood collection. Stored at 30 C in plastic bags for 1 year. Given the lability of coagulation factors, FFP should be transfused within the first 2 hours after rapid defrosting at 37 C. Transfusion of fresh frozen plasma (FFP) poses a high risk of contracting dangerous infections such as HIV, hepatitis B and C, etc. Frequency of anaphylactic and pyrogenic reactions during transfusion of FFP is very high, so compatibility according to the ABO system should be taken into account. And for young women it is necessary to take into account Rh - compatibility. Author: Kolesnikova M.A.
Artificial leather for touch emulation
15.04.2024 Petgugu Global cat litter
15.04.2024 The attractiveness of caring men
14.04.2024
▪ A black hole cannot become heavier than 50 billion suns ▪ Tea bags are dangerous to humans ▪ Cases with a fingerprint sensor for Android devices ▪ It's time to end the riot with gasoline
▪ section of the site Firmware. Article selection ▪ article General and clinical immunology. Crib ▪ article What makes food taste good? Detailed answer ▪ article Sliding eight. Travel Tips ▪ article Electronic code lock. Encyclopedia of radio electronics and electrical engineering ▪ article Antique charger. Encyclopedia of radio electronics and electrical engineering
Home page | Library | Articles | Website map | Site Reviews www.diagram.com.ua |






 Arabic
Arabic Bengali
Bengali Chinese
Chinese English
English French
French German
German Hebrew
Hebrew Hindi
Hindi Italian
Italian Japanese
Japanese Korean
Korean Malay
Malay Polish
Polish Portuguese
Portuguese Spanish
Spanish Turkish
Turkish Ukrainian
Ukrainian Vietnamese
Vietnamese

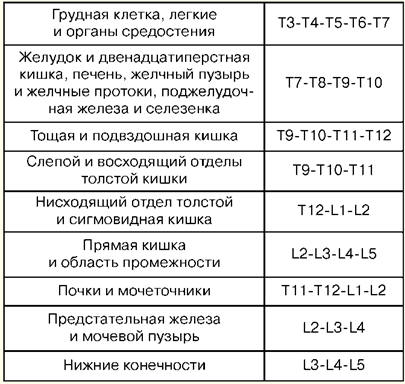


 See other articles Section
See other articles Section 