
|
|
Lecture notes, cheat sheets
Hospital therapy. Lecture notes: briefly, the most important
Directory / Lecture notes, cheat sheets Table of contents
LECTURE No. 1. Diseases of the cardiovascular system. Rheumatism Rheumatism (Sokolsky-Buyo disease) is a systemic inflammatory disease of the connective tissue with a predominant localization of the process in the cardiovascular system, which develops in persons predisposed to it (as a rule, these are young people) due to an acute infection with group A β-hemolytic streptococcus . This definition of the disease was given in 1989 by V. A. Nasonov. It reflects all the characteristic features of the disease: 1) predominant damage to the cardiovascular system; 2) the role of pathological heredity; 3) the significance of streptococcal infection. The essence of the disease lies in the defeat of all membranes of the heart, but mainly the myocardium and endocardium with the occurrence of deformation of the valvular apparatus - heart disease and the subsequent development of heart failure. The defeat of other organs and systems in rheumatism is of secondary importance and does not determine its severity and subsequent prognosis. Etiology. Group A beta-hemolytic streptococci cause damage to the upper respiratory tract. That is why the onset of rheumatism, as a rule, is preceded by a sore throat, an exacerbation of chronic tonsillitis, and an increased amount of streptococcal antigen and anti-streptococcal antibodies (ASL-O, ASG, ASA, antideoxyribonuclease B (anti-DNase B)) are detected in the blood of the sick. Such a connection with a previous streptococcal infection is especially pronounced in the acute course of rheumatism, accompanied by polyarthritis. In the development of rheumatism, age and social factors (adverse living conditions, malnutrition) play a role, and genetic predisposition also matters (rheumatism is a polygenically inherited disease, the existence of "rheumatic" families is well known), which consists in a hyperimmune response to streptococcus antigens, the propensity of patients to autoimmune and immunocomplex processes. Pathogenesis. With rheumatism, a complex and diverse immune response occurs (immediate and delayed hypersensitivity reactions) to numerous streptococcal antigens. When an infection enters the body, anti-streptococcal antibodies are produced and immune complexes are formed (streptococcal antigens + antibodies to them + complement), which circulate in the blood and settle in the microcirculatory bed. Streptococcal toxins and enzymes also have a damaging effect on the myocardium and connective tissue. Due to a genetically determined defect in the immune system, streptococcal antigens and immune complexes are not completely and quickly eliminated from the body of patients. The tissues of such patients have an increased tendency to fix these immune complexes. Cross-reacting antibodies also play a role here, which, being formed on streptococcal antigens, are able to react with tissue, including cardiac, antigens of the body. In response, inflammation develops on an immune basis (according to the type of immediate hypersensitivity), while the factors that implement the inflammatory process are lysosomal enzymes of neutrophils that phagocytize immune complexes and are destroyed at the same time. This inflammatory process is localized in the connective tissue, predominantly of the cardiovascular system, and changes the antigenic properties of it and the myocardium. As a result, autoimmune processes develop according to the type of delayed-type hypersensitivity, and lymphocytes reacting with cardiac tissue are found in the blood of patients. These cells are of great importance in the origin of organ lesions (mainly the heart). In the connective tissue with rheumatism, phase changes occur: mucoid swelling - fibrinoid changes - fibrinoid necrosis. The morphological expression of immune disorders are cellular reactions - infiltration by lymphocytes and plasmocytes, the formation of rheumatic, or Ashoff-Talalayevsky, granuloma. The pathological process ends with sclerosis. Another morphological substrate of heart damage in rheumatic heart disease is a nonspecific inflammatory reaction similar to that in the joints and serous membranes: swelling of the intermuscular connective tissue, fibrin sweating, infiltration by neutrophils and lymphocytes. The disease flows in waves, aggravated under the influence of infection or nonspecific factors (hypothermia, physical stress, stress, etc.), which is associated with the autoimmune nature of the pathological process. When the heart is affected, the inflammatory process can spread to all the membranes of the heart (pancarditis) or in isolation to each of the membranes. Morphological changes in rheumatism are found primarily in the myocardium, so it is myocarditis in the early stages that determines the clinical picture. Inflammatory changes in the endocardium (valvulitis, verrucous endocarditis), damage to the tendon filaments and fibrous ring are clinically detected 6-8 weeks after the attack of rheumatism. The mitral valve is most commonly affected, followed by the aortic and tricuspid valves. The pulmonary valve in rheumatism is almost never affected. Rheumatism classification. Currently, the classification and nomenclature of rheumatism, approved in 1990 by the All-Union Scientific Society of Rheumatology, has been adopted, reflecting the phase of the process, the clinical and anatomical characteristics of damage to organs and systems, the nature of the course and the functional state of the cardiovascular system (see Table 1). clinical picture. All manifestations of the disease can be divided into cardiac and extracardiac. The clinical picture of the disease can be described from these positions. Stage I: the connection of the disease with the transferred infection is revealed. In typical cases, 1-2 weeks after a sore throat or acute respiratory illness, body temperature rises, sometimes up to 38-40 ° C, with fluctuations during the day within 1-2 ° C and strong sweat (usually without chills). With repeated attacks of rheumatism, a recurrence of the disease often develops under the influence of non-specific factors (such as hypothermia, physical overload, surgery). Table 1 Rheumatism classification
The most common manifestation of rheumatism is heart damage - rheumatic heart disease: simultaneous damage to the myocardium and endocardium. In adults, rheumatic heart disease is not severe. Patients complain of mild pain or discomfort in the region of the heart, slight shortness of breath during exercise, interruptions or palpitations are much less common. These symptoms are not specific to rheumatic heart disease and may be seen in other heart conditions. The nature of such complaints is specified at the subsequent stages of the diagnostic search. Rheumocarditis in young patients, as a rule, is severe: from the very beginning of the disease, severe shortness of breath during exercise and at rest, constant pain in the heart, and palpitations are noted. There may be symptoms of circulatory failure in a large circle in the form of edema and heaviness in the right hypochondrium (due to an increase in the liver). All these symptoms point to severe diffuse myocarditis. Pericarditis, as well as extracardiac manifestations of rheumatism, is rare. With the development of dry pericarditis, patients note only constant pain in the region of the heart. With exudative pericarditis, characterized by the accumulation of serous-fibrinous exudate in the heart sac, the pain disappears, as the inflamed pericardial layers are separated by the accumulating exudate. Shortness of breath appears, which increases with the horizontal position of the patient. Due to the difficulty of blood flow to the right heart, congestion appears in a large circle (edema, heaviness in the right hypochondrium due to an increase in the liver). The most characteristic of rheumatism is the defeat of the musculoskeletal system in the form of rheumatic polyarthritis. Patients note rapidly increasing pain in large joints (knee, elbow, shoulder, ankle, wrist), the impossibility of active movements, an increase in the volume of joints. There is a rapid effect after the use of acetylsalicylic acid and other non-steroidal anti-inflammatory drugs with relief for several days, often several hours of all articular manifestations. Rheumatic lesions of the kidneys are also extremely rare, detected only in the study of urine. Lesions of the nervous system in rheumatism are rare, mainly in children. Complaints are similar to those of encephalitis, meningoencephalitis, cerebral vasculitis of a different etiology. Only "small chorea" deserves attention, which occurs in children (more often girls) and is manifested by a combination of emotional lability and violent hyperkinesis of the trunk, limbs and mimic muscles. Abdominal syndrome (peritonitis) occurs almost exclusively in children and adolescents with acute primary rheumatism. It is characterized by sudden onset, fever, and signs of dysphagia (diffuse or localized cramping pains, nausea, vomiting, retention or frequent stools occur). At stage II of the diagnostic search, the detection of signs of heart damage is of little importance. In primary rheumatic heart disease, the heart is usually not enlarged. Auscultation reveals a muffled I tone, sometimes the appearance of a III tone, a soft systolic murmur at the apex. This symptomatology is due to changes in the myocardium. However, an increase in the intensity, duration and persistence of the noise may indicate the formation of mitral valve insufficiency. It is possible to confidently judge the formation of the defect 6 months after the onset of the attack, while maintaining the above auscultatory picture. In case of damage to the aortic valve, a proto-diastolic murmur at the Botkin point may be heard, and the sonority of the II tone may be preserved. Only many years later, after the formation of severe aortic valve insufficiency, weakening (or absence) of the II tone in the II intercostal space on the right joins this auscultatory sign. In patients with polyarthritis, joint deformity is noted due to inflammation of the synovial membrane and periarticular tissues, pain on palpation of the joint. In the area of the affected joints, rheumatic nodules may appear, which are located on the forearms and shins, above the bony prominences. These are small, dense, painless formations that disappear under the influence of treatment. Erythema annulare (a sign almost pathognomonic for rheumatism) are pink ring-shaped elements, not itchy, located on the skin of the inner surface of the arms and legs, abdomen, neck and trunk. This symptom is extremely rare (in 1-2% of patients). Rheumatic pneumonia and pleurisy have the same physical signs as similar diseases of banal etiology. In general, non-cardiac lesions are currently observed extremely rarely, in young people with an acute course of rheumatism (in the presence of high activity - III degree). They are unsharply expressed, quickly amenable to reverse development during antirheumatic therapy. At the III stage of the diagnostic search, the data of laboratory and instrumental studies allow us to establish the activity of the pathological process and clarify the damage to the heart and other organs. With an active rheumatic process, laboratory tests reveal nonspecific acute phase and altered immunological parameters. Acute phase indicators: neutrophilia with a shift of the leukocyte blood formula to the left; an increase in the content of 2-globulins, followed by an increase in the level of - globulins; increase in fibrinogen content; the appearance of C-reactive protein; ESR increases. With regard to immunological parameters, the titers of anti-streptococcal antibodies increase (anti-hyaluronidase and antistreptokinase more than 1: 300, anti-O-streptolysin more than 1: 250). The ECG sometimes reveals rhythm and conduction disturbances: transient atrioventricular blockade (more often I degree - prolongation of the P-Q interval, less often - II degree), extrasystole, atrioventricular rhythm. In a number of patients, a decrease in the amplitude of the T wave is recorded up to the appearance of negative teeth. These rhythm and conduction disturbances are unstable and quickly disappear in the course of antirheumatic therapy. If changes in the ECG are persistent and remain after the elimination of a rheumatic attack, then one should think about organic damage to the myocardium. During phonocardiographic examination, auscultation data are specified: weakening of the XNUMXst tone, the appearance of the XNUMXrd tone, systolic murmur. In the case of the formation of a heart disease, changes appear on the PCG that correspond to the nature of the valvular lesion. X-ray at the first attack of rheumatism, no changes are detected. Only with severe rheumatic heart disease in children and young people can an increase in the heart be detected due to dilatation of the left ventricle. With the development of rheumatic heart disease against the background of an existing heart disease, the x-ray picture will correspond to a specific defect. An echocardiographic study in primary rheumatic heart disease does not reveal any characteristic changes. Only in severe rheumatic heart disease with signs of heart failure on the echocardiogram show signs indicating a decrease in the contractile function of the myocardium and expansion of the heart cavities. Diagnostics. Recognizing primary rheumatism is very difficult, since its most common manifestations, such as polyarthritis and heart damage, are nonspecific. Currently, the major and minor criteria for rheumatism of the American Heart Association are most widely used. The combination of two major or one major and two minor criteria indicates a greater likelihood of rheumatism only in cases of previous streptococcal infection. With the gradual onset of rheumatism, the syndromic diagnosis proposed by A. I. Nesterov in 1973 (see Table 2) matters: clinical and epidemiological syndrome (connection with streptococcal infection); clinical and immunological syndrome (signs of incomplete convalescence, arthralgia, increased titers of antistreptococcal antibodies, as well as the detection of dysproteinemia and acute phase indicators); cardiovascular syndrome (detection of carditis, as well as extracardiac lesions) (see Table 3). Table 2 Criteria for rheumatism
Table 3 Degrees of rheumatism
Differential diagnostics. Rheumatic polyarthritis must be differentiated from non-rheumatic ones (see Table 4). Table 4 Rheumatic and non-rheumatic polyarthritis
The following diseases and symptoms are suspect in relation to rheumatism: 1) endocarditis; 2) myocarditis; 3) pericarditis; 4) heart defects; 5) rhythm and conduction disturbances; 6) acute and chronic heart failure; 7) prolonged subfebrile condition; 8) erythema nodosum; 9) annular erythema; 10) subcutaneous nodules; 11) acute allergic polyarthritis; 12) chorea. None of the clinical syndromes listed above is specific to this disease. Only a combination of heart pathology with at least one extracardiac main symptom of rheumatism gives reason to suspect rheumatism. Recognition of rheumatic heart disease itself is carried out on the basis of symptoms such as shortness of breath and palpitations, fatigue, pain in the region of the heart and heart rhythm disturbances, noises, sometimes a gallop rhythm and a weakening of the I tone. Of great importance in the diagnosis of rheumatic heart disease is the identification of pathology on the ECG. In rheumatism, it is caused by myocarditis, pericarditis and heart defects. Dynamic observation makes it possible to distinguish irreversible changes characteristic of hypertrophy of various parts of the heart in case of defects, from transient ones, indicating the current inflammatory process. Treatment. A positive effect in treatment, as well as prevention of the development of heart disease, is facilitated by early diagnosis and individual treatment, which is based on an assessment of the type of course, the activity of the pathological process, the severity of carditis, and the variant of valvular heart disease. The condition of the myocardium, other tissues and organs, the patient’s profession, etc. are important. Thus, the whole complex of treatment of rheumatism consists of antimicrobial and anti-inflammatory therapy, measures that are aimed at restoring immunological homeostasis. It is recommended to use a rational balanced diet, focus on adaptation to physical activity, preparation for work, timely surgical treatment of patients with complex heart defects. All patients during the active phase of rheumatism are shown penicillin (1-200 IU for 000 doses per day, every 1 hours), which has a bactericidal effect on all types of A-streptococcus. The course of treatment is 500 weeks during the active phase of rheumatism, in the future, a transfer to the prolonged drug bicillin-000 (6 units) is required. With intolerance to penicillin, erythromycin 4 mg 2 times a day can be prescribed. Drugs with anti-inflammatory effect, which are used in the modern treatment of the active phase of rheumatism, are glucocorticosteroids, salicylic, indole derivatives, derivatives of phenylacetic acid, etc. Prednisolone is used at 20-30 mg per day (for 2 weeks, then the dose is reduced by 2,5-5 mg every 5-7 days, for a total of 1,5-2 months) for primary and recurrent with III and II degree activity of the process of rheumatic heart disease, with polyserositis and chorea, with the development of heart failure due to active carditis. In the latter case, triamcinolone at a dose of 12-16 mg per day is preferred, since it has little ability to disturb the electrolyte balance. Corticoid agents affect water-salt metabolism, therefore, potassium chloride 3-4 g / day, panangin and others should be used in the treatment, with fluid retention - aldosterone antagonists (veroshpiron up to 6-8 tablets per day), diuretics (lasix 40 -80 mg / day, furosemide 40-80 mg / day, etc.), with euphoria - tranquilizers, etc. Non-steroidal anti-inflammatory drugs are also widely used for rheumatism: average doses of acetylsalicylic acid are 3-4 g per day, less often 5 g per day or more. Indications for the use of salicylates: 1) minimal degree of activity, slight severity of carditis, mainly myocarditis; 2) long-term treatment of rheumatism, suspicion of a latent course; 3) prolonged treatment with a decrease in the activity of the course of the process and the cessation of the use of corticosteroids, as well as after completion of treatment in a hospital; 4) recurrent rheumatic heart disease occurring against the background of severe heart defects and circulatory failure, since salicylates are not able to retain fluid, prevent the formation of blood clots, and are stimulants of the respiratory center; 5) reducing the likelihood of exacerbation of rheumatism in the spring and autumn periods, as well as after suffering intercurrent infections (together with antibiotics). Acetylsalicylic acid is used 1 g 3-4 times a day after meals for 1-3 months or more with normal tolerance and subject to control of side effects. The successful use of indolacetic acid derivative - indomethacin in rheumatism for more than 20 years. It has a pronounced therapeutic effect: subjective symptoms of carditis (cardialgia, palpitations, shortness of breath) disappear by the 8-10th day of therapy, and objective signs - by the 14-16th day. The disappearance of polyarthritis and polyserositis occurs even faster. In the treatment of rheumatism, a combination of three main stages is important: hospital - clinic - resort. In the hospital, treatment is carried out with the drugs listed above. After reducing the activity of rheumatism and normalizing the patient's condition, they are transferred to stage II - treatment in a rheumatological sanatorium. The main goal of this stage is the continuation of treatment with non-steroidal anti-inflammatory drugs, which are individually selected in the hospital, aminoquinoline derivatives, bicillin-5, rehabilitation. Stage III includes dispensary observation and preventive treatment. This is the implementation of therapeutic measures aimed at the final elimination of the active course of the rheumatic process; conducting symptomatic treatment of circulatory disorders in patients with heart disease; resolving issues of rehabilitation, working capacity and employment; implementation of primary prevention of rheumatism and secondary prevention of recurrence of the disease. LECTURE № 2. Diseases of the cardiovascular system. Cardiomyopathy. Dilated cardiomyopathy 1. Cardiomyopathy Cardiomyopathy - primary isolated myocardial lesions of a non-inflammatory nature of unknown etiology (idiopathic), they are not associated with valvular defects or intracardiac shunts, arterial or pulmonary hypertension, coronary heart disease or systemic diseases (such as: collagenoses, amyloidosis, hemochromatosis, etc.), and in the final stage of the disease, severe congestive heart failure and complex disturbances of the heart rhythm and patency develop. The classification of cardiomyopathies is as follows: 1) dilated cardiomyopathy: a) idiopathic; b) toxic; c) infectious; d) with collagenoses; 2) hypertrophic; 3) restrictive; 4) arrhythmic dysplasia of the right ventricle; 5) a combination of one of the 4 types of cardiomyopathies with arterial hypertension. 2. Dilated cardiomyopathy Dilated cardiomyopathy (DCM) is a disease of the heart muscle characterized by a diffuse expansion of all chambers of the heart (mainly the left ventricle), in which the pathology of the pumping function of the heart is in the foreground and, as a result, chronic heart failure (hence the second name is congestive, when the heart is not able to fully pump blood and it "stagnates" in the tissues and organs of the body). The muscular wall of the heart remains either unchanged or hypertrophied to varying degrees. Diseases and factors that preceded the development of DCM are described in the table below (see Table 5). Table 5 Diseases and factors that preceded the development of DCMP
This is the most common form of damage to the heart muscle. The incidence is 5-8 cases per 100 people per year. There is no clear family history for these patients. Men get sick 000-2 times more often than women. Pathogenesis. As a result of the inflammatory process in the heart muscle (myocarditis), the death of individual cells occurs in its various parts. In this case, inflammation is viral in nature, and cells affected by the virus become foreign agents for the body. Accordingly, when antigens appear in the body, a complex of immune response reactions develops aimed at their destruction. Gradually, dead muscle cells are replaced by connective tissue, which does not have the ability to extensibility and contractility inherent in the myocardium. As a result of the loss of basic myocardial functions, the heart loses its ability to function as a pump. In response to this (as a compensatory reaction), the chambers of the heart expand (i.e., they dilate), and in the remaining part of the myocardium thickening and compaction occurs (i.e., its hypertrophy develops). To increase the delivery of oxygen to the organs and tissues of the body, a persistent increase in heart rate occurs (sinus tachycardia). This compensatory response only temporarily improves the pumping function of the heart. However, the possibilities of myocardial dilatation and hypertrophy are limited by the amount of viable myocardium and are individual for each specific case of the disease. With the transition of the process to the stage of decompensation, chronic heart failure develops. However, at this stage, another compensatory mechanism comes into play: the tissues of the body increase the extraction of oxygen from the blood compared to a healthy body. But this mechanism is insufficient, since a decrease in the pumping function of the heart leads to a decrease in the supply of oxygen to organs and tissues, which is necessary for their normal functioning, while the amount of carbon dioxide in them increases. In 2/3 of patients in the cavities of the ventricles in the late stages of the disease, parietal thrombi form (due to a decrease in the pumping function of the heart, as well as uneven contraction of the myocardium in the chambers of the heart), followed by the development of embolism in the pulmonary or systemic circulation. Pathohistological and pathomorphological changes in the heart. The shape of the heart becomes spherical, its mass increases from 500 to 1000 g, mainly due to the left ventricle. The myocardium becomes flabby, dull, with noticeable whitish layers of connective tissue, there is a characteristic alternation of hypertrophied and atrophic cardiomyocytes. Microscopically, diffuse fibrosis is detected, it can be combined with both atrophy and hypertrophy of cardiomyocytes, in which there is a significant increase in the volume of nuclei, the number of mitochondria, hyperplasia of the Golgi apparatus, an increase in the number of myofibrils, free and associated with the endoplasmic reticulum ribosomes, an abundance of glycogen granules. clinical picture. There are no specific signs of the disease. The clinical picture is polymorphic and is determined by: 1) symptoms of heart failure; 2) rhythm and conduction disturbances; 3) thromboembolic syndrome. All these phenomena develop in the terminal stage of the disease, and therefore the recognition of DCM before the appearance of these symptoms presents significant difficulties. In most cases, the prognosis of the disease is determined by the defeat of the left ventricle of the heart. Before the onset of heart failure, DCM is latent. The most frequent complaints of already onset heart failure are complaints of decreased performance, increased fatigue, shortness of breath during exertion, and then at rest. At night, he has a dry cough (the equivalent of cardiac asthma), later - typical asthma attacks. Patients present with characteristic anginal pain. With the development of congestion in the systemic circulation, heaviness appears in the right hypochondrium (due to an enlarged liver), swelling of the legs. Diagnostics. When diagnosing the disease, an important sign is a significant enlargement of the heart (there are no signs of valvular heart disease or arterial hypertension). Cardiomegaly is manifested by expansion of the heart in both directions, determined by percussion, as well as a displacement of the apical impulse to the left and down. In severe cases, a gallop rhythm, tachycardia, and sounds of relative insufficiency of the mitral or tricuspid valves are heard. Atrial fibrillation develops in 20% of cases. Blood pressure is usually normal or slightly elevated (due to heart failure). Biochemical studies of blood and urine can detect various toxic substances, as well as vitamin deficiencies. Instrumental research methods make it possible to detect: 1) signs of cardiomegaly; 2) changes in indicators of central hemodynamics; 3) rhythm and conduction disturbances. There are no characteristic changes on the ECG or the shifts are nonspecific. These are signs of an increase in the size of the heart, conduction disturbances in the form of a blockade of the anterior branch of the left leg of the atrioventricular bundle (His bundle) or a complete blockade of the left leg (15% of cases); as well as persistent sinus tachycardia (heart rate often exceeds 100 beats per minute). Phonocardiogram confirms auscultatory data in the form of a gallop rhythm, a fairly frequent detection of systolic murmur (due to relative insufficiency of the mitral or tricuspid valve). With congestion in the pulmonary circulation, an accent of the II tone is revealed. X-ray reveals a significant increase in the ventricles (often in combination with a moderate increase in the left atrium) and stagnation of blood in the pulmonary (small) circulation. Violations in the pulmonary circulation are manifested by an increase in the pulmonary vascular pattern, as well as the appearance of transudate in the pleural cavities, which is formed due to increased pressure in the vessels of the lungs. The method of echocardiography is one of the main methods in the diagnosis of the disease. Echocardiography helps to detect dilatation of both ventricles, hypokinesia of the posterior wall of the left ventricle, paradoxical movement of the interventricular septum during systole. In addition, echocardiography allows you to clarify the increase in the amplitude of movement of the unchanged leaflets of the mitral valve. Additional instrumental studies are not mandatory for making a diagnosis, but their results allow us to detail the degree of hemodynamic disorders and the nature of morphological changes in the myocardium. A radioisotope study of the heart (myocardial scintigraphy) is performed to clarify the state of the pumping function of the heart, as well as to determine the zones of the dead myocardium. The study of indicators of central hemodynamics reveals a low minute and stroke volume (minute and stroke indices), an increase in pressure in the pulmonary artery. Angiocardiographically, the same changes are detected as on the echocardiogram. Live myocardial biopsy is not informative for determining the etiology of cardiomyopathy. In some cases, a viral antigen or an increase in the content of LDH, as well as a decrease in energy production by mitochondria, can be detected in the biopsy. However, this surgical method can be used to clarify the etiology of the disease and further therapy. The manipulation is carried out as follows: under local anesthesia, a large artery and vein are pierced (punctured), then a special instrument with small scissors at the end is passed along their course to the heart. When myocardial biopsy is combined with coronary angiography (injection of a contrast agent into the coronary arteries supplying the heart), it becomes possible to exclude coronary artery disease in a patient as one of the diseases that has symptoms similar to DCM. These two studies are performed under X-ray television control. Differential diagnostics. It is produced primarily with myocarditis and myocardial dystrophies, i.e. with those conditions that are sometimes unreasonably called secondary cardiomyopathies. Myocardial biopsy provides significant assistance in the differential diagnosis of dilated cardiomyopathy and heart disease, occurring with a pronounced increase in it: 1) with severe diffuse myocarditis, cellular infiltration of the stroma is found in combination with dystrophic and necrotic changes in cardiomyocytes; 2) with primary amyloidosis occurring with heart damage (the so-called cardiopathic variant of primary amyloidosis), there is a significant deposition of amyloid in the interstitial tissue of the myocardium, combined with atrophy of muscle fibers; 3) with hemochromatosis (a disease caused by a violation of iron metabolism), deposits of iron-containing pigment are found in the myocardium, various degrees of dystrophy and atrophy of muscle fibers, and proliferation of connective tissue are observed. As a variant of DCM, drug-induced and toxic cardiomyopathies can be considered. Numerous agents can cause toxic damage to the myocardium: ethanol, emetine, lithium, cadmium, cobalt, arsenic, isoproterenol and other poisons. Histopathological changes in the tissues of the heart muscle appear as focal dystrophies. In the future, the development of microinfarctions occurs, accompanied by a peripheral inflammatory reaction. The most striking example of toxic cardiomyopathy is cardiomyopathy, which occurs in people who consume excessive beer. It is due to the presence of cobalt in it, which is added to beer to improve foam. Cobalt blocks the action of vitamin B1, and also directly affects the change in the enzymatic processes of the cell. In the acute stage of the course of cobalt cardiomyopathy, the presence of hydropic and fatty degeneration, destruction of intracellular organelles, and focal necrosis of cardiomyocytes are noted. In the future, diffuse or small-focal interstitial fibrosis develops, the final result is the formation of extensive scars. Cobalt cardiomyopathy is more severe than alcoholic cardiomyopathy. If the diagnosis is made on time, then a clinical cure of patients is observed. Alcoholic cardiomyopathy. Ethanol has a direct toxic effect on cardiomyocytes. In addition, with chronic ethyl intoxication, there is often a lack of nutrition. It has been proven that alcohol leads to commulation of fatty acids in cardiomyocytes, since there is a lack of energy, which is necessary for their activity. Acetaldehyde, formed during the metabolism of alcohol, can be a factor in direct toxic effects on protein synthesis. Alcoholism is also accompanied by the activation of latent viruses. Macroscopically, the myocardium is flabby, clay-like, sometimes small scars are observed. The coronary arteries are intact. Microscopic examination shows a combination of dystrophy (hydropic and fatty), atrophy and hypertrophy of cardiomyocytes, possibly the presence of foci of cardiomyocyte lysis and sclerosis. The affected areas of the myocardium contrast with unchanged ones. Electron microscopic examination of heart biopsy specimens shows cystic expansion of the sarcoplasmic reticulum and T-system of cardiomyocytes, which is characteristic of alcoholic cardiomyopathy. Complications of alcoholic cardiomyopathy - sudden death as a result of ventricular fibrillation or chronic heart failure, thromboembolic syndrome. Treatment. Therapy of cardiomyopathies is a difficult task, since the specific causes of their occurrence are not known. The general principles of treatment of DCM do not differ significantly from the treatment of chronic heart failure. In cases of secondary DCM, the previous disease (heart valve disease, etc.) is additionally treated, and all measures are taken to eliminate the causes of DCM. In essence, we can talk about the treatment of patients with cardiomyopathy only when clinical signs appear. In heart failure, cardiac glycosides are ineffective. Patients quickly develop intolerance to drugs (glycoside intoxication), and therefore it is necessary to use glycosides that are rapidly excreted from the body (strophanthin, isolanide). Peripheral vasodilators are quite effective, especially with concomitant anginal syndrome (nitrong, sustak, nitrosorbide). These drugs should be prescribed for severe heart failure, difficult to treat with glycosides and diuretics. With anginal syndrome, it becomes necessary to use antianginal drugs, preferably prolonged nitrates (sustak, nitrong, nitrosorbide). Adrenoblockers are effective (they are prescribed in the absence of signs of heart failure). Of the modern methods of surgical treatment of DCMP, the most effective is heart transplantation (transplantation). However, the possibilities of carrying out this operation are significantly limited. For this reason, as an alternative to heart transplantation in modern treatment, to increase the life expectancy of patients with DCMP, reconstructive surgeries have been developed and are being performed, which are aimed at eliminating insufficiency of the mitral and tricuspid heart valves. Operative elimination of insufficiency of these valves allows for some time to "slow down" the onset of the final stage of the disease. Another alternative to heart transplantation in patients with DCM was the partial removal of the left ventricle in order to reduce its size (Baptiste operation). Not so long ago, for the treatment of patients with DCMP, special models of pacemakers were developed, they allow you to make the work of the ventricles of the heart synchronous. This leads to an improvement in the filling of the ventricles of the heart with blood and an increase in the pumping function of the heart. A separate issue should be considered DCM in children, which is 5-10 cases per 100 children per year. It is noteworthy that the disease can develop in different age groups, including infants. The data obtained in the study of a group of children are as follows: patients received 000 options for therapy (monotherapy with prednisolone, monotherapy with digoxin or prednisolone + digoxin). The effectiveness of the treatment was evaluated according to the following criteria: the heart rate was determined before and after the treatment, the respiratory rate, the state of the ejection fraction and the contractility fraction. The analysis of the obtained results shows that the greatest effect in the treatment of dilated cardiomyopathy in young children is achieved with a combination of corticosteroids and glycosides (prednisolone and digoxin). After completion of the main course of treatment (prednisolone administered 3 mg/kg per day for 2 days, digoxin), there was a pronounced decrease in heart rate, a decrease in shortness of breath. Against the background of monotherapy with prednisolone, a decrease in heart rate occurs. Monotherapy with digoxin leads to a decrease in tachycardia and dyspnea. Given the inadvisability of prescribing cytostatic drugs in young children, since a significant number of treatment complications were observed, it is more optimal in pediatrics to use long-acting cardiac glycosides in combination with corticosteroid hormones in dilated cardiomyopathy. Prevention. Prevention of DCM involves avoiding alcohol, cocaine, and carefully monitoring cardiac parameters during tumor chemotherapy. It is useful to harden the body from an early age. Complete abstinence from alcohol in alcoholic DCM improves heart contractility and may eliminate the need for a heart transplant. The fact that in most cases the diagnosis occurs at the stage of heart failure can also lead to negative results in treatment. Early diagnosis of dilated cardiomyopathy can be performed with random (screening) echocardiography, which is performed during the annual medical examination, as well as when examining people with heredity burdened by this disease. It is in this case that it is possible to increase the effectiveness of drug treatment of DCM. LECTURE № 3. Diseases of the cardiovascular system. Hypertrophic cardiomyopathy Hypertrophic cardiomyopathy (HCM) is a non-coronary disease of the ventricular myocardium (mainly the left), characterized by massive hypertrophy of their walls with protrusion of the interventricular septum (IVS) into the cavity of the right ventricle, which can be significantly thickened, a decrease in the internal volume of the ventricles, normal or increased contractility of the ventricular myocardium and impaired relaxation (diastolic dysfunction). The most common is isolated hypertrophy of the interventricular septum (isolated hypertrophic subaortic stenosis - IHSS) or the apical part of the ventricles. Classification. Classification of HCM by localization of hypertrophy (E. D. Wigle et al., 1985 with additions). I. LV hypertrophy. 1) Asymmetric hypertrophy, in which myocardial hypertrophy of individual walls or segments of the ventricles occurs (including IVS hypertrophy - 90% with or without obstruction of the outflow tract of the left ventricle, midventricular - 1%, apical hypertrophy of the left ventricle - 3%, free wall hypertrophy left ventricle and posterior part of the IVS - 1%). 2) Symmetrical (concentric) hypertrophy of the left ventricle, when myocardial hypertrophy extends to all walls of the ventricles, occurs in 5% of cases. II. Hypertrophy of the pancreas. In the case when myocardial hypertrophy prevents the normal outflow of blood from the ventricles of the heart, they speak of an obstructive form of HCM. In other cases, HCM is non-obstructive. Etiology. The disease can be either congenital or acquired. Congenital HCM is inherited in an autosomal dominant manner. Within the same family, various forms and variants of HCM can be observed. Most often, asymmetric hypertrophy of the interventricular septum is inherited. The acquired form of HCM occurs in elderly patients with a history of arterial hypertension. The prevalence is 0,02-0,05%. The reasons for the development of acquired HCM are not fully understood. According to one of the proposed hypotheses, individuals with acquired HCM in the prenatal period develop a defect in the adrenergic receptors of the heart involved in the regulation of cardiac activity, in particular heart rate. As a result, the sensitivity to norepinephrine and similar hormones, which increase the heart rate, is significantly increased, which affects the development of myocardial hypertrophy in them, and eventually HCM. Pathohistological picture. Disoriented, incorrect, chaotic arrangement of cardiomyocytes and myofibrils in cardiomyocytes, myocardial fibrosis is a violation of the architectonics of the heart muscle. Pathogenesis. Hemodynamic disorders arise due to impaired diastolic function of the heart. During diastole, insufficient blood flows into the ventricles (especially the left) due to their density and rigidity, which leads to a rapid rise in end-diastolic pressure. Both increased myocardial stiffness and increased intraventricular pressure cause less blood to be ejected from the ventricle during systole. For adequate delivery of oxygen to the organs and tissues of the body (with the normal functioning of the cardiovascular system), for the implementation of any load, the release of blood from the heart must increase. Accordingly, in response to the load, the heart rate increases. With the development of HCM, the filling of the heart with blood also suffers at rest, and with an increase in the heart rate during the period of exercise, it is even more negatively affected. As a result of this, there is no adequate increase in the pumping function of the heart during exercise in HCM. Physical activity in HCM affects the increase in intraventricular pressure, which leads to an increase in pressure in the left atrium located above, as well as in the vessels of the small (pulmonary) circulation. Under these conditions, hyperfunction and hypertrophy of the left atrium develop, and later - pulmonary hypertension ("passive"). As a result, shortness of breath occurs, which is proportional to the degree of load. Since during exercise the ejection of blood from the left ventricle does not correspond to the increase in load, the blood flow in the coronary arteries that feed the heart muscle itself begins to suffer. It also plays an important role that in HCM there is a discrepancy between a significant mass of hypertrophied myocardium and the possibility of coronary blood supply, which remains the same as in healthy people. The decrease in blood flow through the coronary arteries leads to the occurrence of angina pectoris in the middle and in the left half of the chest, radiating to the left arm, under the left shoulder blade. Like shortness of breath, angina pectoris is provoked by physical exertion. In some cases of HCM during exercise, the cerebral blood supply also deteriorates, resulting in syncope. It should be noted that to reduce the increase in intraventricular pressure during exercise, there is a compensatory mechanism, the operation of which is based on the fact that the cavity of the left atrium expands, and the thickness of its walls increases. As a result, there is an additional filling of the left ventricle with blood during exercise. However, this is only a temporary compensation due to the fact that the reserve of the left atrium as a "pump" is insignificant, and a significant expansion of the cavity of the left atrium leads to the development of atrial fibrillation. clinical picture. HCM is characterized by an extreme variety of symptoms, which causes misdiagnosis. The presence and timing of complaints in HCM are mainly determined by 2 factors: the form of HCM and the location of the lesion. The most powerful chamber of the heart is the left ventricle, therefore, with hypertrophy of the myocardial walls, complaints may not appear for a long time. Isolated damage to the right ventricle of the heart is extremely rare. In the non-obstructive form of HCM, when nothing interferes with the outflow of blood from the ventricle, the patient may not present any complaints. Sometimes there may be shortness of breath (with significant physical exertion), interruptions in the work of the heart, as well as an irregular heartbeat. In the obstructive form of HCM, the ejection of blood from the heart during exercise is significantly reduced due to the presence of an obstruction to the outflow of blood from the ventricle. In this case, the typical complaints are shortness of breath on exertion, angina pectoris and fainting. The disease is characterized by a slow progression of complaints from the moment of its onset. Due to the similarity of complaints (pain in the region of the heart and behind the sternum) and study data (intense systolic murmur), rheumatic heart disease and coronary heart disease are most often misdiagnosed. The clinical picture of HCM is: 1) signs of ventricular myocardial hypertrophy (mainly left); 2) a sign of insufficient diastolic ventricular function; 3) variable signs of left ventricular outflow tract obstruction. Diagnostics. In the process of diagnostic search, the most significant is the detection of systolic murmur, altered pulse and displaced apical impulse. The auscultatory picture of the heart in patients with obstructive HCM has a number of features: the maximum sound of the systolic murmur (ejection murmur) is determined at the Botkin point and at the apex of the heart, the severity of the murmur is proportional to the degree of obstruction, its intensification occurs when the patient stands up abruptly, as well as during the Valsalva test ; II tone is always preserved; noise is not carried out on the vessels of the neck. The pulse is usually high and fast. This is due to the absence of narrowing in the outflow tracts from the left ventricle at the beginning of systole, but then, with the contraction of powerful muscles, a “functional” narrowing of the outflow tracts appears, as a result of which the pulse wave decreases prematurely. The apex beat in about 1/3 of cases has a "double" character: at first, on palpation, a blow is felt from contraction of the left atrium, then from contraction of the left ventricle. For the convenience of identifying this property of the apex beat, palpation is best done with the patient lying on his left side. For the diagnosis of HCM, echocardiography data are of the greatest importance, allowing to clarify the anatomical features of the disease, the severity of myocardial hypertrophy, obstruction of the outflow tract of the left ventricle. The following signs are revealed: asymmetric hypertrophy of the IVS, more pronounced in the upper third, its hypokinesis; systolic movement of the anterior leaflet of the mitral valve in the anterior direction; contact of the anterior leaflet of the mitral valve with the IVS in diastole. Nonspecific signs are: hypertrophy of the left atrium, hypertrophy of the posterior wall of the left ventricle, a decrease in the average speed of the diastolic cover of the anterior leaflet of the mitral valve. On the ECG, any specific changes are found only with sufficiently developed left ventricular hypertrophy. By recording an ECG for 24 hours (Holter monitoring), existing heart rhythm disturbances are detected. An ECG test with dosed physical activity using a bicycle ergometer or treadmill allows you to assess the severity of the symptoms of the disease, its prognosis and develop appropriate treatment. Isolated hypertrophy of the IVS causes an increase in the amplitude of the Q wave in the left chest leads (V5-6), which complicates the differential diagnosis with focal changes due to myocardial infarction. However, a small width of the Q wave allows excluding a myocardial infarction. In the process of developing hemodynamic overload of the left atrium, the ECG may show signs of left atrial hypertrophy: widening of the P wave for more than 0,10 s, an increase in its amplitude, the appearance of a biphasic P wave in lead V1 with the second phase increased in amplitude and duration. X-ray diagnostics is important only in the advanced stage of the disease, when an increase in the left ventricle and left atrium, an expansion of the descending part of the aorta can be determined. On the phonocardiogram, the amplitudes of I and II tones are preserved, which is a differential sign of HCM from stenosis of the aortic orifice, and systolic murmur of varying severity is also detected. Invasive research methods (probing of the left parts of the heart, contrast angiography) are currently not mandatory, since echocardiography provides quite reliable information for making a diagnosis. However, sometimes these methods are used in controversial cases to clarify the diagnosis or in preparing patients for surgery. Cardiac probing is used under X-ray television control. Technique for performing the method: by puncturing a large artery under local anesthesia with the further introduction of a special catheter into the heart cavity, the pressure gradient (difference) between the left ventricle and the aorta departing from it is measured. Normally, this gradient should not be. However, with HCM, there is a pressure difference between the left ventricle and the aorta from 50 to 150 mm Hg. Art., an increase in end-diastolic pressure in the cavity of the left ventricle up to 18 mm Hg. Art. The pressure gradient decreases after the introduction of β-blockers. Also, during sounding of the heart, a contrast agent is injected into the cavity of the ventricle (ventriculography) to study its anatomical features. In a number of patients (as a rule, these are persons over 40 years old), angiography of the coronary arteries (coronary angiography) is simultaneously used before heart surgery to clarify the etiology of angina pectoris and exclude concomitant coronary artery disease. Treatment. The basis of drug treatment for HCM is drugs that improve blood flow to the ventricles of the heart in diastole. These drugs are a group of β-blockers (anaprilin, atenolol, metoprolol and propranolol, 160-320 mg/day, etc.) and a group of calcium ion antagonists (verapamil, but with caution). Novokinamid and disopyramide also reduce heart rate and have an antiarrhythmic effect. At the very beginning of treatment, small doses of these drugs are used, then the dosage is gradually increased to the maximum tolerated by the patient. β-blockers are used with caution in diabetes mellitus, bronchial asthma and some other diseases. When treating with these drugs, constant monitoring of blood pressure and pulse rate is necessary. Dangerous is a decrease in pressure below 90/60 mm Hg. Art. and heart rate below 55 per minute. If a patient has dangerous rhythm disturbances that cannot be treated with β-blockers or calcium ion antagonists, then other antiarrhythmic drugs are additionally used in the treatment of such patients. The appointment of anticoagulants is recommended for paroxysmal arrhythmias and atrial fibrillation, as well as in the presence of blood clots in the heart chambers (warfarin, etc.). During the period of treatment with these drugs, it is necessary to regularly monitor a number of indicators of the blood coagulation system. With a significant overdose of anticoagulants, external (nasal, uterine, etc.) and internal bleeding (hematomas, etc.) are possible. Surgical treatment is performed in patients with obstructive HCM when medical treatment is not effective or when the gradient between the left ventricle and aorta is more than 30 mm Hg. Art. (the operation of myotomy or myectomy is performed - excision or removal of a part of the hypertrophied myocardium of the left ventricle). Mitral valve replacement and non-surgical IVS ablation are also performed. Prevention. All patients with HCM, especially those with an obstructive form, are contraindicated in sports that can significantly increase physical activity over a short period of time (athletics, football, hockey). Prevention of the disease lies in early diagnosis, which makes it possible to begin early treatment of the disease and prevent the development of severe myocardial hypertrophy. It is mandatory to perform echocardiography in genetic relatives of the patient. Screening ECG and EchoCG, which are carried out during an annual medical examination, are also important for diagnosis. In patients with obstructive HCM, it is necessary to prevent infective endocarditis (antibiotic prophylaxis, etc.), since the presence of obstruction creates conditions for the development of this life-threatening condition. LECTURE № 4. Diseases of the cardiovascular system. Restrictive cardiomyopathy Restrictive cardiomyopathy (RCMP) - (from the Latin word restrictio - "restriction") - a group of diseases of the myocardium and endocardium, in which, as a result of pronounced fibrosis and loss of elasticity, due to various reasons, there is a fixed restriction in the filling of the ventricles in diastole. The filling of the ventricles is carried out in the phase of early filling, followed by stabilization of intraventricular pressure. The disease is accompanied by insufficient blood filling of the heart, which further leads to the development of chronic heart failure. Restrictive cardiomyopathy is the least studied and least common of all cardiomyopathies. RCMP includes: Lefler's parietal fibroplastic endocarditis (found in countries with a temperate climate, described by W. Loffler et al., 1936) and endomyocardial fibrosis (found in countries of tropical Africa, described by D. Bedford et E. Konstman). Previously, they were considered as two independent pathological processes. However, the pathomorphological picture in these diseases differs little. Causes of RCM. Primary RCM is very rare, and the only proven cause of its occurrence is the so-called hypereosinophilic syndrome (Leffler's disease, Leffler's parietal fibroplastic endocarditis). It occurs mainly in men aged 30-40 years. With hypereosinophilic syndrome, inflammation of the endocardium occurs, which over time culminates in significant compaction of the endocardium and its rough adhesion to the adjacent myocardium, which leads to a sharp decrease in the extensibility of the heart muscle. Lefler's syndrome is also characterized by persistent eosinophilia for 6 months or more (1500 eosinophils per 1 mm3), damage to internal organs (liver, kidneys, lungs, bone marrow). In the vast majority of cases, the origin of RCMP is secondary, due to other reasons, among which the most common are: 1) amyloidosis - a disease associated with a violation of protein metabolism in the body; at the same time, in the tissues of various organs, an abnormal protein (amyloid) is formed and deposited in large quantities; when the heart is damaged, amyloid causes a decrease in its contractility and extensibility; 2) hemochromatosis - a violation of iron metabolism in the body, accompanied by an increased content of iron in the blood, its excess is deposited in many organs and tissues, including the myocardium, thereby causing a decrease in its extensibility; 3) sarcoidosis - a disease of unknown etiology, characterized by the formation of cell clusters (granulomas) in organs and tissues; the lungs, liver, lymph nodes and spleen are most often affected; and developing granulomas in the myocardium lead to a decrease in its extensibility; 4) endocardial diseases (endocardial fibrosis, endocardial fibroelastosis, etc.), when there is a significant thickening and compaction of the endocardium, which also leads to a sharp limitation of myocardial extensibility. Fibroelastosis of the endocardium, in particular, can only occur in infants; this disease is not compatible with life due to the early development of severe heart failure. Pathogenesis. With RCM, myocardial compliance suffers for various reasons. As a result, the filling of the ventricles with blood decreases and intraventricular pressure increases significantly. However, unlike HCM, the possibility of developing compensatory myocardial hypertrophy in restrictive cardiomyopathy is small. Thus, after some time, stagnation occurs in the pulmonary circulation and the pumping function of the heart decreases, which leads to gradual fluid retention in the body, the development of persistent swelling of the legs, hepatomegaly and ascites. If the compaction of the endocardium extends to the atrioventricular valves (mitral and tricuspid), this is aggravated by the development of their insufficiency, and also leads to thrombosis in the heart cavities due to their reduced contractility and extensibility. The spread of fragments of these blood clots with the bloodstream can cause thromboembolism and blockage of large vessels, heart attacks of internal organs. With the spread of pathological inclusions of the myocardium to the zone of the conduction system of the heart, various violations of the conduction of the cardiac impulse may appear, accompanied by the development of blockades. With RCMP, various types of arrhythmias are also quite often observed. Based on the above, we can conclude that the disease from a pathogenetic point of view proceeds in 3 stages. Stage I - necrotic - eosinophilic infiltration of the myocardium and other organs. Stage II - thrombotic - the formation of blood clots in the cavities of the left and right ventricles, the development of thromboembolic complications and the gradual thickening of the endocardium mainly in the apical regions and near the atrioventricular valves. Stage III - fibrous, characterized by thickening of the endocardium up to several millimeters, myocardial fibrosis is expressed - mainly subendocardial areas. The cavity is partially obliterated due to organized thrombi, fibrosis of the mitral valve cusps, mitral regurgitation are noted. Pronounced atrial dilatation. Restrictive diastolic dysfunction is observed. clinical picture. Manifestations of the disease are extremely polymorphic and are determined by symptoms of circulatory disorders in the small or large circle (depending on the predominant damage to the right or left ventricles). Complaints may be absent or may be due to congestion in the pulmonary or systemic circulation. Patients usually complain of shortness of breath, which first appears during exercise, and as the disease progresses, shortness of breath is observed at rest. Due to a decrease in the pumping function of the heart, the patient complains of fatigue and poor tolerance to any load. Over time, swelling of the legs, an enlarged liver and dropsy of the abdomen join. Periodically, an irregular heartbeat appears, and with the development of persistent blockades, there may be fainting. The first stage of the development of the disease (necrotic) is characterized by the appearance of fever, weight loss, cough, skin rash and tachycardia. Diagnostics. Recognizing RCM is extremely difficult. One can speak with confidence about this pathology only after excluding a number of similar diseases (such as idiopathic myocarditis of the Abramov-Fiedler type, exudative pericarditis, valvular heart defects). When examining patients with RCMP, symptoms characteristic of congestive heart failure (edema, hepatomegaly and ascites), as well as pronounced pulsation of the neck veins, are found. The latter is due to the difficulty of blood supply to the heart due to poor myocardial extensibility. During auscultation, the detection of an enlarged heart, a soft late systolic murmur and a loud early III tone (due to rapid filling of the ventricles during diastole) is of great importance. Murmurs in the heart are also detected in patients with atrioventricular valve insufficiency. An ECG study reveals moderate hypertrophy of the ventricular myocardium, as well as various disturbances in the rhythm and conduction of the heart impulse, and nonspecific changes in the T wave on the ECG. Echocardiography is one of the most informative methods for diagnosing the disease, with its help, thickening of the endocardium, a change in the nature of the filling of the ventricles of the heart, a decrease in the pumping function of the heart, a rapid movement of the anterior leaflet of the mitral valve during diastole and a rapid early movement of the posterior wall of the left ventricle outward are detected. Magnetic resonance imaging allows you to obtain information about the anatomy of the heart, determine pathological inclusions in the myocardium and measure the thickness of the endocardium. When examining the parameters of central hemodynamics, an increased filling pressure in both ventricles is determined, and the final pressure in the left exceeds that in the right ventricle. Ventriculography reveals increased contraction of the left ventricle, smooth contours of its walls, sometimes with a filling defect in the apex (evidence of obliteration). In some cases, depressions in the region of the papillary muscles are determined. There are signs of valvular insufficiency, in particular the mitral or tricuspid valve. Differential diagnostics. In the differential diagnosis of RCM, it is very important to take into account the similarity of the disease in external manifestations with constrictive pericarditis, but the treatment method for these diseases is diametrically opposite. Intravital biopsy of the myocardium and endocardium is usually used simultaneously with cardiac probing, which allows for greater information to clarify the nature of the disease and further treatment. In extremely rare cases, when the above diagnostic methods do not allow distinguishing RCM from constrictive pericarditis, a direct inspection of the pericardium is performed on the operating table. All patients with RCMP need a comprehensive clinical, biochemical and additional examination to determine non-cardiac causes of the disease. Treatment. Treatment of the disease presents significant difficulties. Most drugs that are used to treat heart failure may not bring the desired results due to the fact that, due to the characteristics of the disease, it is impossible to obtain a significant improvement in myocardial compliance (in some cases, calcium ion antagonists are prescribed for these purposes). Diuretics (aldactone) are used to eliminate excess fluid in the body. To eliminate persistent conduction disorders, it may be necessary to install (implant) a permanent pacemaker. This is caused by diseases such as sarcoidosis and hemochromatosis, leading to the development of secondary RCMP, they are subject to self-treatment. In the treatment of sarcoidosis, hormonal drugs (prednisolone, etc.) are used, and in hemochromatosis, regular bloodletting (to reduce the concentration of iron in the body). Treatment of myocardial amyloidosis is directly dependent on the causes of its occurrence. It is advisable to use anticoagulant drugs for thrombosis in the chambers of the heart. Surgical treatment is resorted to in cases of RCMP caused by endocardial damage. During the operation, if possible, the part of the endocardium that has undergone changes is excised. In some cases, if there is insufficiency of the atrioventricular valves, their prosthesis is performed. Some forms of amyloid myocardial damage are treated with a heart transplant. Prevention of RCMP. Unfortunately, preventive measures for this disease are limited. Mainly, early identification of potentially preventable causes of amyloidosis, sarcoidosis, hemochromatosis, etc. is necessary. To achieve these goals, annual medical examination of the population is of great importance. LECTURE No. 5. Diseases of the cardiovascular system. Infective endocaditis Infective endocarditis (IE) - a disease consisting in a polyposis-ulcerative lesion of the valvular apparatus of the heart (often with the development of valvular insufficiency) or parietal endocardium (less often, the endothelium of the aorta or the nearest large artery is affected). The disease is caused by various pathogenic microorganisms and is accompanied by a systemic lesion of the internal organs (kidneys, liver, spleen) against the background of an altered reactivity of the organism. Until now, in various printed publications, the previously used terms "bacterial endocarditis", "protracted septic endocarditis" can be found to refer to this pathological process. However, it is the term "infective endocarditis" that replaced them that better reflects the cause of the disease caused by a wide variety of microorganisms - bacterial agents, rickettsiae, viruses and fungi. The number of patients with IE is increasing worldwide. This is due to the presence of so-called risk groups (patients with atherosclerotic, rheumatic, traumatic valve injuries, heart or valve defects, ventricular septal defect, aortic coarctation) as a result of the fact that infection occurs more easily on a pathologically altered valve or endocardium. Etiology. The pathogenic causative agents of the disease are most often the coccal group of microorganisms - streptococci (viridans streptococcus was previously isolated in 90% of cases), staphylococci (golden, white), enterococcus, pneumococcus. In recent years, due to the widespread use of antibiotics, the range of microbial pathogens has changed. The disease can be caused by gram-negative flora (Escherichia coli, Pseudomonas aeruginosa, Proteus, Klebsiella); evidence has emerged of the important role of pathogenic fungi, Sarcinus, Brucella and viruses. Diseases caused by these pathogens are more severe, especially endocarditis caused by a fungal infection (usually occurs due to irrational use of antibiotics). However, in some patients the true causative agent of the disease is not detected (negative blood culture rate 20-50%). Often, infection occurs at the site of a prosthetic valve - the so-called prosthetic IE, which develops mainly within 2 months after heart valve replacement surgery. In this case, the causative agent of the disease most often has a streptococcal nature. Thus, the sources of infection and bacteremia in IE are very different (surgeries in the oral cavity, operations and diagnostic procedures in the urogenital area, surgical intervention on the cardiovascular system (including valve replacement), prolonged stay of the catheter in a vein, frequent intravenous infusions and endoscopic research methods, chronic hemodialysis (arteriovenous shunt), intravenous drug administration). There are so-called primary IE, which developed on intact valves, as well as IE against the background of congenital and acquired changes in the heart and its valvular apparatus - secondary endocarditis. These changes make it possible to distinguish patients into separate risk groups: heart defects (congenital and acquired), mitral valve prolapse, arteriovenous aneurysms, post-infarction aneurysms, shunts, condition after surgery on the heart and large vessels. Pathogenesis. The mechanism of development of IE is complex and insufficiently studied, however, the main points in the development of the disease can be identified. If there is a focus of infection in the body under the influence of altered humoral and local (cellular) immunity with a perversion of immunological reactions, various endogenous and exogenous factors, bacteremia develops. From the blood, microorganisms enter the heart valves, creating a secondary focus of infection there. The fixation and reproduction of microorganisms on the endocardium is facilitated by a number of factors: a previous change in the tissue and surface of the valve, the presence of thrombotic masses on it, arising under the influence of the direct damaging effect of the blood stream when its intracardiac circulation changes in conditions of existing heart disease. At the same time, various blood cells (platelets, etc.) “glue” to the site of traumatic injury, forming cell growths resembling icicles hanging from the valve. These vegetations become available for infection that has entered the vascular bed. Deformation of the valves due to the occurrence of a large pressure gradient, the narrowness of the hole and changes in blood flow velocity also contributes to the introduction of infectious agents into the endocardium with the formation of an infectious focus. When a previously intact valve is damaged, changes occur that disrupt the normal properties of individual sections of this valve (swelling appears), exudative or proliferative processes ("interstitial valvulitis" - preclinical phase). In the development of the disease, stage III can be distinguished. Stage I (infectious-toxic) proceeds with varying degrees of severity of intoxication. There is a growth of bacteria, the destruction of valves, leading to the development of heart disease; at the same stage, a generalization of the process often occurs due to the hematogenous spread of infection - pieces of cusps or colonies of microorganisms can separate from the valve, the cusps can rupture. The detachment of pieces of valve microbial vegetation contributes to the introduction of infected emboli into various parts of the vascular bed and exacerbates septic manifestations. Pieces of the valve or microbial vegetations circulate through the body with blood flow, when they enter the brain, they cause cerebral infarctions, which are accompanied by paralysis, paresis and various other neurological disorders. The valve, which has undergone destruction, cannot perform its function, and soon there is lightning-fast developing heart failure. Stage II - immuno-inflammatory, in which microorganisms fixed on the valves cause prolonged autosensitization and hyperergic damage to the organs and tissues of the body (immune generalization of the process). During this period, immune complexes circulate in the blood and are fixed in tissues (heart, kidneys, liver, blood vessels). Immune and autoimmune disorders cause the development of vasculitis and visceritis (immunocomplex nephritis, myocarditis, hepatitis, capillaritis, etc.). Stage III - dystrophic - occurs with the progression of the pathological process: the functions of a number of organs are disturbed, heart and kidney failure occurs, further aggravating the course of the disease. Classification. Currently, the classification and nomenclature of IE are used, reflecting the clinical form, course variant, degree of activity, pathogenetic phase and clinical and morphological form of the disease (see Table 6). Table 6 Classification of IE
A distinction is also made between active and inactive (healed) IE. There is also a surgical classification, in which they distinguish: 1) the lesion is limited to the valve leaflets; 2) the lesion extends beyond the valve. Acute IE (rapidly progressive, develops over 8-10 weeks) is rare, usually in individuals who have not previously had heart disease, and is clinically manifested by a picture of general sepsis. With modern methods of treatment, it is possible to translate it into subacute. Subacute IE (most common) lasts 3-4 months, with adequate drug therapy, remission may occur. However, relapses of the disease are possible. Protracted IE lasts for many months with periods of exacerbation and remission, it is characterized by mild clinical manifestations, minor laboratory parameters and general disturbances. The disease usually responds well to treatment. With an unfavorable course, severe complications arise, and patients die from progressive heart failure, increasing septic intoxication. clinical picture. Depending on the causative agent of the infection, IE can occur suddenly and develop rapidly (Staphylococcus aureus, enterococci) or have a latent onset (viridans streptococcus). Manifestations of IE are presented in the form of syndromes. 1) Syndrome of inflammatory changes and septicemia (fever, chills, hemorrhagic rashes, changes in acute phase blood parameters: leukocytosis with a shift to the left, an increase in ESR, the appearance of C-reactive protein, an increase in fibrinogen, α2-globulins. 2) Syndrome of general intoxication of the body (weakness, sweating, headaches, myalgia and arthralgia, loss of appetite, pallor of the skin with an icteric tint). 3) Syndrome of valve damage (formation of heart disease). 4) Syndrome of "laboratory" immune disorders (the presence of immune complexes circulating in the blood or fixed in the kidneys, myocardium, blood vessels; hypergammaglobulinemia; the appearance of rheumatoid factor; detection of anti-tissue antibodies). 5) Syndrome of thromboembolic complications (focal nephritis, myocardial infarction, spleen, intestines, thromboembolism in the brain, vessels of the lower extremities, etc.). 6) Syndrome of generalization of lesions (diffuse glomerulonephritis, myocarditis, hepatitis, vasculitis, etc.). The severity of these syndromes is different. It depends on the nature of the course of IE, stage, type of pathogen. For example, staphylococcal IE is characterized by high activity of the process, severe symptoms of general intoxication, and the development of purulent complications. Fungal endocarditis is usually accompanied by embolic occlusion of large arteries, especially of the lower extremities. A typical picture of the disease is characteristic of IE caused by streptococcus viridans. The onset of the disease is often associated with an acute infection or exacerbation of a chronic infection, as well as with a number of medical manipulations. Especially characteristic is the combination of an increase in body temperature of varying degrees (from prolonged fever to subfebrile condition or normal temperature) with chills and sweating. The patient presents simultaneous complaints due to the presence of an infectious process and intoxication, as well as thromboembolic complications of heart damage. Patients may have a history of episodes of long-term antibiotic treatment (this occurs when IE recurs in previously treated patients). Diagnostics. Of greatest importance for making a correct diagnosis is the detection of damage to the heart valves by changes in the auscultatory pattern of pre-existing heart defects; the appearance of “additional” noise. Characteristic lesions of the skin and mucous membranes are revealed: café au lait skin color, hemorrhages, positive Hecht's (pinch) and Konchalovsky-Rumpel-Leede (tourniquet) symptoms, as well as Osler's nodes - painful hyperemic dense nodules on the palmar surface and fingertips , Lukin-Libman sign (Lukin spots) - hemorrhage on the transitional fold of the conjunctiva. Splenomegaly is often observed in IE. Significant weight loss (sometimes 15-20 kg) is very typical. In rare cases, pericarditis develops (a faint pleural friction noise caused by fibrinous deposits on the pericardium). Physical examination may reveal increased blood pressure, indicating the development of diffuse glomerulonephritis. Sometimes signs of dysfunction of the central nervous system (paresis, hyperkinesis, pathological reflexes, etc.) as a result of embolism of cerebral vessels are determined. In this case, the most common diagnostic error is the assessment of a particular syndrome as a manifestation of an independent disease (for example, with pronounced signs of liver damage, hepatitis is diagnosed, etc.). However, the diagnosis of IE is based primarily on the early detection of the causative agent of the disease. For this, the following laboratory and instrumental studies are used. 1) Obtaining a positive blood culture is the most important diagnostic sign of IE. Analysis is also necessary to select the most effective antibiotic in this case. At least 2-3 of them are required to confirm the diagnosis. Of great importance are the technique of blood sampling and culture, the time of inoculation (preferably at the height of fever), the use of enriched media. 2) Carrying out NBT (nitrobluttetrazolium test) - diagnosticum of systemic bacterial infections, which allows to differentiate bacterial infections from other inflammatory diseases. The method is based on the reduction of soluble NBT dye by neutrophils into an insoluble formazan precipitate. If the number of NBT-positive cells is more than 10%, the test is considered positive. 3) Clinical blood test to detect acute phase indicators: an increase in ESR to 50 mm / h or more, leukocytosis with a shift of the leukocyte formula to the left or (in stage II) leukopenia and hypochromic anemia can be detected. Diagnostic value is attached to the detection of histiocytes in the blood taken from the earlobe. Their content of more than 6 in the field of view may indicate in favor of IE. A biochemical blood test shows an increase in the content of fibrinogen, α2-globulins and α-globulins - up to 30-40%. 4) Identification of immunological changes: hypergammaglobulinemia, circulating immune complexes, decrease in complement titer, the appearance of rheumatoid (antiglobulin) factor, increased reaction of imperious transformation of lymphocytes with PHA (phytohemagglutinin) and bacterial antigens, detection of anti-tissue antibodies. 5) Urinalysis is performed to clarify the lesions of various organs and systems, when glomerulonephritis is detected, manifested by proteinuria, cylindruria and hematuria. An increase in the content of bilirubin, transaminases indicates liver damage. 6) A direct diagnostic sign of IE - the presence of vegetation on the heart valves - is detected by echocardiography. Thus, from the whole variety of symptoms, the main and additional ones should be distinguished. The main criteria for the diagnosis of IE: 1) fever with a temperature above 38 ° C with chills; 2) Lukin spots; 3) Osler's nodules; 4) endocarditis on unchanged valves (primary) or against the background of rheumatic and congenital heart defects. infectious myocarditis; 5) multiple arterial thromboembolism, ruptures of mycotic aneurysms with hemorrhages; 6) splenomegaly; 7) positive blood culture; 8) a pronounced positive effect from the use of antibiotics. Additional criteria for the diagnosis of IE: 1) an increase in body temperature up to 38 ° C, chilling; 2) hemorrhages on the skin; 3) rapid weight loss; 4) asymmetric arthritis of small joints of hands, feet; 5) anemization; 6) ESR over 40 mm/h; 7) sharply positive SRV; 8) the presence of rheumatoid factor; 9) α-globulins above 25%; 10) increase in the content of immunoglobulins M, E and A. Differential diagnostics. Although thromboembolism is most often observed in IE, other causes of embolism in the artery of the systemic circulation should not be excluded: transmural myocardial infarction and cardiac aneurysm, idiopathic Abramov-Fiedler myocarditis and atrial fibrillation of various origins, but primarily observed in rheumatic stenosis of the left atrioventricular orifice . Rheumatic and infective endocarditis are of the greatest importance for differential diagnosis (Table 7). Table 7 Differential diagnostic criteria for rheumatic endocarditis and prolonged IE
The characteristic symptoms of IE include an enlarged spleen. However, a large, firm, painless spleen is seen in amyloidosis; soft, painless indicates its septic hyperplasia. Soreness is noted with infarction of the spleen, located subcapsularly. Splenomegaly may be one of the manifestations of portal hypertension in right heart failure. In this case, it is combined with ascites and hepatomegaly. An increase in liver size with prolonged IE is observed quite often. Septic hyperplasia is characterized by relatively small enlargement and soft consistency of the liver. There are fatty degeneration and extremely rarely - liver infarcts. Most often, an increase in the liver is associated with venous congestion with right heart failure. In the absence of ascites, congestion is recognized retrospectively by a decrease in liver size after treatment with cardiac glycosides and diuretics. Treatment. Treatment of IE should be as early and etiotropic as possible, taking into account bacteriological data. Before antibacterial drugs found their widespread use in medical practice, most patients with IE died from infection and its complications. More than 80% are now successfully cured. But for nearly 20%, drug treatment fails and they soon develop heart failure, which is nearly untreatable. In this regard, a combination of conservative and surgical treatment is advisable. For the treatment of IE in any age group, antibiotics are primarily used that have a bactericidal effect on microorganisms, preferably in individualized doses depending on the concentration of the antibiotic in the blood and the sensitivity of the pathogen to it. The drug of first choice is still penicillin. It has low toxicity, which allows it to be used for a long time at relatively high dosages. The daily dose - up to 20 IU is administered intravenously and intramuscularly. However, one should not exclude the fact that in elderly and senile patients, when treated with penicillin and other antibiotics in high doses, a cardiotoxic effect is often observed: the appearance or intensification of heart failure, pain in the heart, tachycardia. When the dose is reduced or the drug is changed, these phenomena stop. With an unknown etiology, treatment begins with high doses of benzylpenicillin intramuscularly or intravenously up to 18-000 units or more, a combination with streptomycin up to 000 g / m per day or aminoglycosides (gentamicin, tobramycin at the rate of 20-000 mg / day) is used. kg per day). In the absence of effect or after determining the pathogen, semi-synthetic penicillins are used (oxacillin, methicillin or ampicillin intramuscularly up to 000 g / day). Cephalosporins are also basic drugs used for the treatment of IE: the most commonly used are claforan, cefamisin (1-4 g/day, intramuscularly and intravenously), as well as zeporin (6-12 g/day) and kefzol (up to 4-10 g intravenously). and etc.). Fusidin has a good anti-staphylococcal effect, in some cases it is effective in the resistance of microorganisms to other antibiotics (10-16 g / day). Antibiotic treatment is prescribed for a long time in a course of 1,5-2 months, until the infection is completely eliminated. After the elimination of the infection, the general condition of the patient improves, the vegetation disappears according to echocardiography and microbiological confirmation. With reduced immunoreactivity of the organism, antibacterial agents are combined with passive immunotherapy (for example, with staphylococcal endocarditis - with antistaphylococcal plasma or antistaphylococcal α-globulin), using immunomodulators (thymalin, T-activin, etc.). To prevent thrombosis, for example, with endocarditis that has developed against the background of angiogenic sepsis, controlled hypocoagulation is created using heparin (20-000 IU intravenously or subcutaneously). For inhibition of proteolytic enzymes, contrical is used (up to 25-000 IU intravenously). When valvular IE contributed to the formation of valvular heart disease or the manifestations of the disease do not disappear despite massive antibiotic therapy, it is advisable to perform surgical treatment. An additional argument in favor of surgical intervention is repeated embolism from the heart valve leaflets destroyed by infection. Sometimes the infection goes beyond the boundaries of the valve ring, while forming abscesses, which is also an indication for surgical treatment. The main goal of the operation is to preserve the patient's own valve. Sometimes they are limited to removing vegetations, suturing ruptures of the valves, etc. If the valve is almost completely destroyed under the influence of infection, it is replaced with an artificial one (prosthesis) using mechanical and biological prostheses. Prevention. Prevention of IE consists of timely sanitation of chronic foci of infection in the oral cavity, tonsils, nasopharynx, paranasal sinuses, and the use of active antibacterial therapy for acute streptococcal and staphylococcal diseases (angina, etc.). It is recommended to harden the body. All patients with valvular heart disease, as well as with valve prostheses, should take antibiotics prophylactically the day before and shortly after any intervention, after which an infection can enter the bloodstream. Dispensary observation of persons who have had acute streptococcal, staphylococcal infections is necessary. LECTURE No. 6. Diseases of the respiratory system. Bronchial asthma An exhaustive definition of asthma does not exist to date, however, the most complete definition of this disease was given by G. B. Fedoseev in 1982. Bronchial asthma (BA) is an independent, chronic, recurrent disease with a predominant lesion of the respiratory tract, the main and obligatory pathogenetic mechanism of which is an altered bronchial reactivity due to specific (immunological) and (or) non-specific, congenital or acquired mechanisms, and the main (mandatory) clinical sign is an asthma attack and (or) an asthmatic condition (asthmatic status) due to spasm of bronchial smooth muscles, hypersecretion, dyscrinia and edema of the bronchial mucosa. Etiology. A combination of several factors plays an important role in the occurrence of asthma. In this regard, there are 2 forms of asthma - atopic (from the Latin athopia - “hereditary predisposition”) and infectious-allergic. Hereditary predisposition is due to the association of certain histocompatibility antigens (HLA) with the severity of asthma, and an increase in the severity of the disease is especially often observed in carriers of B antigens35 and B40. Internal factors in the development of the disease are biological defects in the immune, endocrine systems, autonomic nervous system, bronchial sensitivity and reactivity, mucociliary clearance, pulmonary vascular endothelium, rapid response system (mast cells, etc.), metabolism of arachidonic acid, etc. External factors include: 1) infectious allergens (viruses, bacteria, fungi, yeast, etc.); 2) non-infectious allergens (pollen, dust, industrial, medicinal, food; allergens of ticks, insects and animals); 3) mechanical and chemical irritants (metal, wood, silicate, cotton dust; vapors of acids, alkalis; fumes, etc.); 4) meteorological and physico-chemical factors (changes in air temperature and humidity, fluctuations in barometric pressure, the Earth's magnetic field, physical effort, etc.); 5) stressful, neuropsychic effects and physical activity. Infectious agents can have not only an allergenic effect, but also reduce the body's sensitivity threshold to non-infectious (atopic) allergens, increase the permeability of the respiratory mucosa for them; to form a change in the reactivity of target cells (mast cells, basophils, monocytes, etc.) and effector systems. Pathogenesis. Altered bronchial reactivity is a central link in the pathogenesis of the disease and can be primary or secondary. In the first case, changes in reactivity can be congenital or acquired due to direct exposure to chemical, mechanical, physical factors and infection. Secondary changes in bronchial reactivity are a manifestation of changes in the reactivity of the body's immune, endocrine, and nervous systems. Thus, speaking about the pathogenesis of AD, we can distinguish 2 groups of mechanisms: immunological and non-immunological. Immunological mechanisms in the vast majority of cases are dominant in the course of the disease. Violations of the immunocompetent system in the mucous membrane of the respiratory tract, occurring according to types I, III and IV of hypersensitivity reactions, i.e. with a change in humoral and cellular immunities, lead to a change in bronchial reactivity. At the same time, there is a decrease in secretory IgA, the phagocytosis system is disturbed, the T-suppressor function of lymphocytes decreases, the production of interferon decreases, which ultimately leads to a decrease in the body's antiviral defense. Type I (atopic, reaginic, or anaphylactic). In response to the ingestion of exoallergen antigens (pollen, animal and plant proteins, bacteria and drugs) into the body, there is an increased production of IgE (reagins), which are fixed and accumulate on mast cells (primary effector cells). This is the immunological stage of AD. Following this, the pathochemical stage of the process develops - degranulation of mast cells with the release of vasoactive, bronchospastic and chemotactic substances (histamine, serotonin, various chemotactic factors, etc.). These are primary mediators acting on vessels and target cells (secondary effector cells) - eosinophils, neutrophils, platelets, macrophage monocytes. The latter, when exposed to primary mediators, secrete secondary mediators (leukotrienes, prostaglandins, thromboxanes, platelet-activating factor and other substances belonging to the group of eicosanoids). Under the influence of biologically active substances, the pathophysiological stage of pathogenesis begins: the permeability of the microcirculatory bed increases, which leads to the development of edema, serous inflammation, and bronchospasm. Clinically, this is manifested by an acute violation of bronchial patency and the development of an asthma attack. Type III reaction (immunocomplex type, or Arthus phenomenon) develops under the influence of exoallergens and endoallergens (autoallergens, which are formed by the denaturation of proteins of bronchioles and alveoli as a result of infectious or allergic inflammation and the action of various irritants). The reaction occurs in the zone of excess antigen with the participation of precipitating antibodies belonging to the immunoglobulins of classes O and M. The damaging effect of the formed antigen-antibody complex is realized through complement activation, the release of lysosomal enzymes. There is damage to the basal membranes, spasm of smooth muscles of the bronchi, vasodilation, and the permeability of the microvasculature increases. Type IV (cellular, delayed-type hypersensitivity) is characterized by the fact that sensitized lymphocytes have a damaging effect. In this case, the mediators of the allergic reaction are lymphokines (act on macrophages, epithelial cells), lysosomal enzymes, and an activated kinin system. Under the influence of these substances, the development of edema, swelling of the mucous membrane, bronchospasm, hyperproduction of viscous bronchial secretions occur. The consequence is an acute violation of the patency of the bronchi, manifested by an attack of suffocation. Non-immunological mechanisms are the primary change in bronchial reactivity as a result of congenital and acquired biological defects. Non-immunological mechanisms act on primary or secondary effector cells or on the receptors of the smooth muscles of the bronchi, blood vessels, cells of the bronchial glands. This changes the reactivity of target cells and, above all, mast cells, which is accompanied by excessive production of biologically active substances (histamine, leukotrienes, etc.). In response to their release, bronchospasm, swelling of the mucous membrane, hyper- and discrinia of the bronchial glands develop. All this dramatically changes the patency of the bronchi and causes an asthma attack. Bronchial resistance can change conditionally and unconditionally as a reflex. For example, obstruction arising from exposure to cold air, inhalation of irritating gases and dust, and physical activity is caused by bronchospasm through the vagal reflex. The causes of bronchospasm can also be damage to the effector zones of the vagal bronchoconstrictive reflex or blockade of β-adrenergic receptors. Recently, they talk about a special role in the pathogenesis of violations of bronchial patency of glucocorticoid insufficiency and disovarian disorders. Insufficiency of glucocorticosteroids leads to the development of hyperreactivity of mast cells, a decrease in the synthesis of catecholamines, and activation of prostaglandins F2a, as well as a violation of the immunocompetent system (here we talk about the complex participation in the pathogenesis of AD and immunological and non-immunological mechanisms). Hyperestrogenemia and hypoprogesteronemia act on α- and β-adrenergic receptors, increasing the activity of the former and reducing the activity of the latter. Classification. The predominance of one or another mechanism in the pathogenesis of asthma allows us to identify its various pathogenetic features. Currently, the classification proposed by G. B. Fedoseev (1982) is used. Stages of AD development. I - pre-asthma (conditions that threaten development: acute and chronic bronchitis, acute and chronic pneumonia with elements of bronchospasm in combination with vasomotor rhinitis, urticaria). II - clinically formed BA (considered as such after the first attack or immediately onset of status asthmaticus). BA forms: 1) immunological; 2) non-immunological. Pathogenetic mechanisms (clinical and pathogenetic variants) of AD: 1) atopic; 2) infection-dependent; 3) autoimmune; 4) dishormonal; 5) neuropsychic imbalance; 6) adrenergic imbalance; 7) cholinergic imbalance; 8) primary altered bronchial reactivity. In one patient, a combination of several clinical and pathogenetic variants is possible. In such a situation, it is necessary at the time of the examination to highlight the main variant for this patient, which is important for adequate therapy. In the course of a long course of BA, a change in the pathogenetic mechanism is possible. Severity of BA: 1) mild course (exacerbations are rare, 2-3 times a year, short-term asthma attacks are stopped by taking various bronchodilator drugs inside); 2) moderate (more frequent exacerbations 3-4 times a year, asthma attacks are more severe and stopped by injections of drugs); 3) severe course (characterized by frequent and prolonged exacerbations, severe attacks, often turning into an asthmatic state). The division of BA according to the severity of the course is conditional. So, with a mild course of BA, the patient may die from a suddenly developed status asthmaticus. Phases of the course of BA: 1) exacerbation (the presence of recurrent attacks of asthma or asthmatic condition); 2) subsiding exacerbation (attacks become more rare and mild, physical and functional signs of the disease are less pronounced than in the exacerbation phase); 3) remission (typical manifestations of BA disappear: asthma attacks do not occur; bronchial patency is fully or partially restored). Complications: 1) pulmonary: emphysema, pulmonary insufficiency, atelectasis, pneumothorax, status asthmaticus, etc.; 2) extrapulmonary: cor pulmonale (compensated and decompensated with the development of right heart failure), myocardial dystrophy, etc. clinical picture. The most characteristic sign of asthma is complaints of attacks of suffocation (difficulty breathing mainly during exhalation), shortness of breath and cough of various types (from dry, paroxysmal or with the release of viscous sputum). The development of bronchopulmonary infection causes an increase in body temperature. The resulting difficulty in nasal breathing is a manifestation of allergic rhinosinusopathy (vasomotor rhinitis, polyposis), which usually occurs during the pre-asthma phase. History data helps to establish a connection between the development of seizures and exposure to certain allergens and other factors. Most often it is a respiratory tract infection, especially in an exacerbation of the disease. From the anamnesis, they learn about the influence of physical effort (such as brisk walking, laughter, etc.), changes in meteorological factors (such as cold, high humidity, etc.), disovarial disorders, professional factors on the occurrence of asthma attacks. The study of an allergic history contributes to the diagnosis of an atopic variant of BA. In such cases, exacerbations of the disease are seasonal (more often in spring and summer), accompanied by rhinitis, conjunctivitis. Such patients have urticaria, Quincke's edema; food intolerance, a number of medicinal substances are detected; there is a hereditary predisposition to allergic diseases. History data often allow to establish the presence of the so-called aspirin asthma. In this case, there is no hereditary form of allergic diseases. Such patients are concerned about impaired nasal breathing (polypous growths), and the most characteristic symptom is intolerance to non-steroidal anti-inflammatory drugs (acetylsalicylic acid, indomethacin, etc.), which cause asthmatic attacks. In this case, it is already possible to assume a prostaglandin mechanism of AD. Data on the development of asthmatic status in the past indicate the severity of the course of the disease and indicate the need for corticosteroid therapy. Diagnostics. Of great importance is the identification of extrapulmonary manifestations of allergies, signs of broncho-obstruction, complications of asthma, and other diseases accompanied by bronchospasm attacks. When examining the skin, allergic manifestations can be detected: urticaria, papular erythematous rashes, which indicates an immunological variant of BA. The combination of asthma with eczema, neurodermatitis, psoriasis predisposes to severe asthma. It is often possible to identify a violation of nasal breathing. Rhinitis and polyps are considered pre-asthma. Sinusitis and other sinusitis can cause choking. Physical examination of the lungs, often due to underlying chronic bronchitis, may reveal signs of emphysema leading to the development of chronic respiratory failure and cor pulmonale. Auscultatory signs of bronchial obstruction are detected: a change in breathing (long expiration, dry, mostly wheezing, wheezing), forced expiration, which reveals latent bronchospasm (appearance or increase of dry wheezing). Auscultation of the lungs must be carried out in the position of the patient lying down: the number of dry rales increases with their "vagal" mechanism. Constantly listened to in a certain area, moist voiced ("crackling") fine bubbling rales may indicate a developed pneumosclerosis. An objective examination of the patient reveals symptoms of other diseases ("butterfly" on the skin of the face, lymphadenopathy in combination with an increase in the liver and spleen, a persistent increase in blood pressure, persistent fever, etc.), in which attacks of bronchospasm occur, manifested by suffocation (systemic lupus erythematosus, nodular periarteritis). Then the alleged diagnosis of AD becomes unlikely. Spirography reveals the characteristic signs of obstructive bronchial obstruction: a decrease in forced expiratory volume in the first second (FEV1), a decrease in the Tiffno coefficient (FEV1 to VC as a percentage) and the percentage of FEV1 to FZhEL. During exacerbation of BA, the residual lung volume (RLV) and functional residual capacity (FOC) exceed the initial level by 100% or more. When analyzing the spirogram, signs of tracheobronchial dyskinesia are found, contributing to the violation of bronchial patency, by the presence of a notch in the upper part of the descending color of the spirogram (Kolbet-Wyss symptom). Pneumotachometry shows the predominance of inspiratory power over expiratory power, which is characteristic of bronchial obstruction. According to pneumotachography with the construction of the "flow - volume" curve, a violation of bronchial patency is diagnosed separately at the level of large, medium and small bronchi. The appearance of increased bronchial resistance, recorded using spirography, pneumotachometry and pneumotachography, in response to physical activity, inhalation of cold air, irritating gases and acetylcholine indicates an altered bronchial reactivity. Allergological testing is carried out using a set of various non-infectious and infectious allergens, it is carried out only outside the exacerbation of the disease. To assess the provoking effect of the allergen, skin allergic tests are performed (application, scarification and intradermal methods of applying the allergen), the allergen can be applied to the conjunctiva of the eye, the nasal mucosa. The most reliable is the specific diagnosis of asthma - the identification of specific bronchial hyperreactivity with the help of inhalation provocative tests. However, one should not lose sight of the fact that this route of administration can provoke a severe attack of asthma or the development of status asthmaticus. For the specific diagnosis of AD, for example, when it is impossible to conduct an allergological test, a radioimmunosorbent test is also used, which makes it possible to quantify IgE antibodies. Laboratory studies help confirm the proposed diagnosis, evaluate the evolution of the disease and the effectiveness of the treatment. The main diagnostic criterion for AD is the appearance of eosinophils in the sputum, but this is a non-specific sign, it can serve as a manifestation of a general allergic reaction of the body. Also of diagnostic importance is the detection of Kurshman spirals and Charcot-Leiden crystals in sputum. Laboratory studies prove the presence of an active inflammatory process and the degree of its severity in terms of an increase in acute phase indicators. With an increase in respiratory failure in case of exacerbation of asthma and status asthmaticus, it is important to study the acid-base state and blood gas composition. X-ray examination diagnoses foci of infection (in the paranasal sinuses, teeth, gallbladder) and the presence of acute (pneumonia) or exacerbation of a chronic inflammatory process in the lungs, emphysema and pneumosclerosis. ECG data prove signs of the development of compensated cor pulmonale - hypertrophy of the right heart. Differential diagnostics. BA is differentiated from cardiac asthma (see Table 8). Table 8 Differential diagnosis of AD
It is also necessary to differentiate infectious-allergic and atopic asthma (see Table 9). Table 9 Infectious-allergic and atopic asthma
Treatment. In the treatment of asthma, a stepwise approach is recommended, which is explained by the variable severity of its course in different people and in the same patient. Stage 1 is the least severe asthma, stage 4 is the greatest. Step 1: A mild intermittent course in which asthma symptoms appear on exposure to a trigger (eg, pollen or animal hair) or due to exercise. Long-term use of anti-inflammatory drugs in the treatment of such patients is not indicated. Treatment consists of prophylactic medication if necessary (inhaled β2agonists, cromoglycate, nedocromil, or anticholinergics). Occasionally, more severe and prolonged exacerbations require a short course of oral corticosteroids. If asthma manifests itself with more frequent symptoms, an increase in the need for bronchodilators, then it becomes necessary to move to the next stage. Stage 2. Slight persistent course. Primary therapy includes anti-inflammatory drugs, inhaled corticosteroids, sodium cromoglycate, or nedocromil sodium. The dosage of corticosteroids is 200-500 micrograms of beclomethasone dipropionate or budesonide per day. For symptomatic treatment, inhaled β2-agonists, but not more than 3-4 times a day. For more severe and prolonged exacerbations, a short course of oral corticosteroids is given. If symptoms persist despite an initial dose of inhaled corticosteroids, the dose of beclomethasone dipropionate should be increased to 750-800 micrograms per day. However, an alternative to increasing the dose of inhaled hormones, especially to control nocturnal attacks of asthma, is the addition of long-acting bronchodilators taken at night (at a dose of inhaled corticosteroids of at least 500 mcg). Stage 3 is characterized by moderate severity of BA. Such patients require daily intake of prophylactic anti-inflammatory drugs. The dose of inhaled corticosteroids is 800-2000 mcg in combination with long-acting bronchodilators. You can use long-acting theophyllines (with constant monitoring of their concentration no more than 5-15 µg / ml), oral and inhaled β2long-acting agonists. Symptomatically appoint β2-short-acting agonists or alternative drugs (stage 2). Stage 4. Severe asthma, when it is not completely controlled. In this case, the goal of treatment is to achieve the best possible results. Primary treatment involves high-dose inhaled corticosteroids (between 800 and 2000 micrograms per day of beclomethasone dipropionate) in combination with long-acting bronchodilators. If necessary, inhaled β is indicated to relieve symptoms.2-short-acting agonists (not more than 3-4 times a day). A more severe exacerbation may require a course of treatment with oral corticosteroids, which are prescribed in minimal doses or every other day. To prevent the development of side effects, high doses of inhaled corticosteroids are administered through a spacer. Step 5 involves reducing supportive medication. This is possible if the asthma remains under control for at least 3 months, which helps to reduce the risk of side effects and increases the patient's susceptibility to the planned treatment. "Reduction" of treatment is carried out under the constant control of symptoms, clinical manifestations and indicators of respiratory functions by gradually reducing (cancelling) the last dose or additional drugs. Stopping attacks. A mild attack can be treated at home with short-acting bronchodilators. Treatment is carried out until the symptoms disappear completely. Moderate and severe attacks require not only adequate doses of short-acting bronchodilators (inhaled β2-short-acting agonists), but also the appointment of systemic corticosteroids. If the patient has hypoxemia, oxygen should be administered. For the treatment of asthma attacks in a medical center or hospital, high doses of inhaled β2agonists through a nebulizer. The use of a metered-dose aerosol inhaler through a spacer is very effective. Preferably, corticosteroids are administered orally, not intravenously. When using theophylline or aminophylline in combination with high doses of β2-agonists additional bronchodilating effect is not provided, but the risk of side effects increases. Theophyllines can only be used in the absence of β2-agonists, however, they can be administered intravenously at the rate of 6 mg/kg aminophylline (or 5 mg/kg theophylline) with a constant dose of 0,5-1,0 mg/kg per hour for 24 hours. Alternatively, β2Short-acting agonists can also use epinephrine, but significant side effects are possible with its use. Inhaled mucolytic drugs, sedatives and antihistamines, magnesium sulfate, chest physiotherapy, hydration with large volumes of fluids for adults and older children are not recommended for the treatment of asthma attacks to avoid increased coughing. Prevention. Primary prevention of asthma includes treatment of patients in a state of pre-asthma, identification of biological defects in practically healthy individuals with a family history that pose a threat to the occurrence of asthma, elimination of potentially dangerous allergens, irritants and other factors from the environment of patients that can lead to the development of the disease. In the treatment of patients in a state of preasthma, it is necessary to sanitize the foci of infection, treat allergic rhinosinusopathy, apply various methods of non-drug treatment, including acupuncture and psychotherapy, exercise therapy, barotherapy, and spa treatment. Carrying out specific and nonspecific hyposensitization is shown. LECTURE No. 7. Diseases of the respiratory system. Chronical bronchitis Chronic obstructive bronchitis is a diffuse non-allergic inflammatory lesion of the bronchial tree, caused by prolonged irritating effects on the bronchi of various agents, which has a progressive course and is characterized by obstructive pulmonary ventilation, mucus formation and the draining function of the bronchial tree, which is manifested by cough, sputum and shortness of breath. According to the WHO definition, if a patient coughs up sputum on most days for at least 3 consecutive months for more than 2 consecutive years, the disease is considered chronic bronchitis (CB). Chronic bronchitis is divided into primary and secondary. Primary chronic bronchitis is an independent disease that is not associated with other bronchopulmonary processes or damage to other organs and systems, in which there is a diffuse lesion of the bronchial tree. Secondary CB develops against the background of other diseases - both pulmonary (tuberculosis, bronchiectasis, etc.) and extrapulmonary (uremia, congestive heart failure, etc.). Most often it is local in nature (segmental). Consider primary HB. Etiology. Both exogenous factors (tobacco smoke, air pollution, unfavorable professional conditions, climatic and infectious factors) and endogenous factors (pathology of the nasopharynx, impaired breathing through the nose, repeated acute respiratory diseases, acute bronchitis and focal infection of the upper respiratory tract) play a role in the development of CB. pathways, hereditary predisposition, metabolic disorders (obesity)). Pathogenesis. Under the influence of exogenous and with the participation of endogenous factors in the tracheobronchial tree, the structural and functional properties of the mucous membrane and submucosal layer change, inflammation of the mucous membrane develops, and the patency and drainage function of the bronchi are disrupted. Structural and functional changes in the mucous membrane and submucosal layer are expressed in hyperplasia and hyperfunction of goblet cells, bronchial glands, hypersecretion of thick and viscous mucus, which leads to disruption in the mucociliary transport system. The amount of secretory IgA-lysozyme and lactoferrin produced is reduced. Edema of the mucous membrane develops, and then - atrophy and metaplasia of the epithelium. Inflammation of the mucous membrane is caused by various irritants in combination with infection (viral and bacterial). Chemical substances (pollutants) contained in the air have a damaging effect on the respiratory tract, swelling of the mucous membrane occurs and inhibition of the activity of the ciliated epithelium occurs. This leads to a violation of the evacuation and a decrease in the barrier function of the bronchial mucosa. Catarrhal contents are replaced by catarrhal-purulent, and then purulent. The spread of the inflammatory process to the distal sections of the bronchial tree disrupts the production of surfactant and reduces the activity of alveolar macrophages that phagocytize foreign particles. If the bronchospasm that occurs in case of inflammation is pronounced, then a bronchospastic (non-allergic) component develops. The associated infection during exacerbation of inflammation contributes to the development of an asthmatic (allergic) component, which makes it possible to attribute such CB to pre-asthma. Obstructive syndrome develops due to a combination of a number of factors: 1) spasm of smooth muscles of the bronchi as a result of irritating effects of exogenous factors and inflammatory changes in the mucous membrane; 2) hypersecretion of mucus, changes in its rheological properties, leading to disruption of mucociliary transport and blockage of the bronchi with a viscous secret; 3) epithelium metaplasia from cylindrical to stratified squamous and its hyperplasia; 4) violations of the production of surfactant; 5) inflammatory edema and mucosal infiltration; 6) collapse of small bronchi and obliteration of bronchioles; 7) allergic changes in the mucous membrane. If large-caliber bronchi are involved in the process (proximal bronchitis), bronchial obstruction is not expressed. But in case of damage to small and medium bronchi, a pronounced violation of bronchial patency occurs. However, with an isolated lesion of small bronchi (distal bronchitis), devoid of cough receptors, shortness of breath may be the only evidence of developed bronchitis, and cough appears when larger bronchi are involved in the process. Various ratios of changes in the mucous membrane cause the formation of a certain clinical form: 1) with catarrhal non-obstructive bronchitis, superficial changes in the structural and functional properties of the mucous membrane prevail; 2) with mucopurulent (purulent) bronchitis, the processes of infectious inflammation predominate. However, a situation is also possible when long-term catarrhal bronchitis due to the addition of an infection can become mucopurulent, etc. In the non-obstructive variant of all clinical forms of chronic bronchitis, ventilation disorders are slightly pronounced; 3) obstructive disorders initially appear only against the background of an exacerbation of the disease and are caused by inflammatory changes in the bronchi, hyper- and dyskrinia, bronchospasm (reversible components of obstruction), but then they persist constantly, while the obstructive syndrome grows slowly. In obstructive chronic bronchitis, thickening of the mucous membrane and submucosal layer, edema and hypersecretion predominate, and persistent ventilation disorders are also characteristic. Developed obstruction of the small bronchi leads to emphysema. In its course, HB undergoes a certain evolution. As a result of the development of emphysema and pneumosclerosis, uneven ventilation of the lungs is noted, hyper- and hypoventilated areas are formed. In combination with local inflammatory changes, this leads to impaired gas exchange, respiratory failure, arterial hypoxemia and pulmonary hypertension, followed by the development of the main life-threatening condition - right ventricular failure. Classification. There is currently no generally accepted classification of CB. It is important to divide CB into obstructive and non-obstructive variants, with each of which a catarrhal (mucous), catarrhal-purulent or purulent inflammatory process can develop. The classification also includes rare forms - hemorrhagic and fibrinous CB. According to the level of bronchial damage, they distinguish: with a predominant lesion, large bronchi (proximal bronchitis) and with a predominant lesion of small bronchi (distal bronchitis) (N. R. Paleev, 1985). clinical picture. The main symptoms of CB are cough, sputum production, and shortness of breath. During an exacerbation of the disease or due to hypoxia with the development of pulmonary failure and other complications, general symptoms are identified (sweating, weakness, increased body temperature, fatigue, etc.). Cough is the most typical manifestation of the disease. Based on the nature and consistency of the sputum, one can assume a variant of the course of the disease. In the non-obstructive version of catarrhal bronchitis, the cough is accompanied by the release of a small amount of mucous, watery sputum (usually in the morning, after exercise or due to increased breathing). At the beginning of the disease, the cough does not bother the patient; the appearance of paroxysmal cough indicates the development of bronchial obstruction. The cough takes on a barking tone and is paroxysmal in nature with pronounced expiratory collapse of the trachea and large bronchi. With purulent and mucopurulent bronchitis, patients are more concerned about coughing up sputum. In the event of an exacerbation of the disease, sputum acquires a purulent character, its amount increases, sometimes sputum is excreted with difficulty (due to bronchial obstruction during exacerbation). In the obstructive variant of bronchitis, the cough is unproductive and hacking, accompanied by shortness of breath, with a small amount of sputum. Shortness of breath occurs in all patients with chronic bronchitis at various times. The appearance of shortness of breath in "long-term coughing" patients initially with significant physical exertion indicates the addition of bronchial obstruction. As the disease progresses, shortness of breath becomes more pronounced and constant, i.e., respiratory (pulmonary) insufficiency develops. In the non-obstructive variant, CB progresses slowly, shortness of breath usually appears 20-30 years after the onset of the disease. Such patients almost never fix the onset of the disease, but only indicate the appearance of complications or frequent exacerbations. There is a history of hypersensitivity to cold, and most patients report long-term smoking. In a number of patients, the disease is associated with occupational hazards at work. When analyzing a cough history, it is necessary to make sure that the patient has no other pathology of the bronchopulmonary apparatus (tuberculosis, tumors, bronchiectasis, pneumoconiosis, systemic diseases of the connective tissue, etc.), accompanied by the same symptoms. Sometimes a history indicates hemoptysis due to mild vulnerability of the bronchial mucosa. Recurrent hemoptysis indicates a hemorrhagic form of bronchitis. In addition, hemoptysis in chronic, long-term bronchitis may be the first symptom of lung cancer or bronchiectasis. Diagnostics. Auscultation reveals hard breathing (with the development of emphysema it can become weakened) and dry wheezing of a scattered nature, the timbre of which depends on the caliber of the affected bronchi (wheezing, well audible on exhalation, is characteristic of damage to small bronchi). Changes in auscultation data will be minimal in chronic non-obstructive bronchitis in remission and most pronounced during exacerbation of the process (wet rales of various calibers that may disappear after a good cough and sputum production). With an exacerbation of obstructive bronchitis, shortness of breath increases, the phenomena of respiratory failure increase. A purulent viscous secret further complicates the patency of the bronchi. The obstructive component that has joined both the catarrhal and mucopurulent forms of bronchitis, and during the period of exacerbation or in the course of their evolution, significantly aggravates the course of bronchitis. Signs of bronchial obstruction: prolongation of the expiratory phase with calm and especially forced breathing; wheezing on expiration (better auscultated with forced breathing and in the supine position); symptoms of obstructive pulmonary emphysema. In advanced cases of chronic bronchitis and with the addition of complications, signs of emphysema of the lungs, respiratory and cardiac (right ventricular) insufficiency - decompensated pulmonary heart appear: acrocyanosis, pastosity or swelling of the legs and feet, changes in the nails in the form of watch glasses, and the terminal phalanges of the hands and feet - in in the form of drumsticks, swelling of the cervical veins, pulsation in the epigastric region due to the right ventricle, accent of the II tone in the II intercostal space to the left of the sternum, liver enlargement. Affects the picture of the disease and the addition of an asthmatic (allergic) component, when there is a resemblance to bronchial asthma. Laboratory and instrumental indicators have a different degree of significance depending on the stage of the process. In the initial period of the disease or in the remission phase, there may be no changes. However, these indicators are of great importance for identifying the activity of the inflammatory process; clarification of the clinical form of the disease; identifying complications; differential diagnosis with diseases that have similar clinical symptoms. X-ray examination of the chest organs is performed in all patients with chronic bronchitis, however, as a rule, there are no changes in the lungs on plain radiographs. There may be a mesh deformation of the lung pattern, due to the development of pneumosclerosis. With a long course of the process, signs of emphysema are revealed. With the development of the pulmonary heart, a bulging of the trunk of the pulmonary artery appears on the left contour of the shadow of the heart, expansion of the basal arteries, followed by their cone-shaped narrowing and a decrease in the diameter of peripheral branches. X-ray examination plays an important role in the diagnosis of complications (acute pneumonia, bronchiectasis) and in the differential diagnosis with diseases with similar symptoms. Bronchography is used only to diagnose bronchiectasis. Bronchoscopy is of great importance in the diagnosis of chronic bronchitis and its differentiation from diseases that manifest a similar clinical picture. It confirms the presence of an inflammatory process; clarifies the nature of inflammation (the diagnosis of hemorrhagic or fibrinous bronchitis is made only after this study); reveals functional disorders of the tracheobronchial tree (it is especially important to identify expiratory collapse - dyskinesia of the trachea and large bronchi); helps in identifying organic lesions of the bronchial tree. In addition, bronchoscopy allows you to get the contents of the bronchi or washings for microbiological, parasitological and cytological studies. The study of the function of external respiration is carried out to identify restrictive and obstructive disorders of pulmonary ventilation. According to the spirogram, the Tiffno index is calculated (the ratio of forced expiratory volume in 1 s - FEV1 to the vital capacity of the lungs - VC as a percentage) and an indicator of air velocity - PSV (the ratio of maximum ventilation of the lungs - MVL to VC). With the development of obstructive syndrome, there is a decrease in the absolute speed indicators of external respiration (MVL and FEV1), exceeding the degree of reduction of VC; the Tiffno index decreases and the bronchial resistance on expiration increases. According to pneumotachometry, the predominance of inspiratory power over expiratory power is revealed as an early sign of bronchial obstruction. Identification of violations of bronchial patency at different levels of the bronchial tree is possible with the help of special pneumotachographs, which make it possible to obtain a "flow-volume" curve. Peripheral obstruction is characterized by a significant decrease in the flow-volume curve in the area of low volume. The joint assessment of bronchial resistance and lung volumes also helps to determine the level of obstruction. In the case of obstruction at the level of the large bronchi, there is an increase in the residual volume of the lungs (RLV), and the total lung capacity (TLC) does not increase. With peripheral obstruction, a more significant increase in TRL and an increase in TRL are observed. To identify the proportion of bronchospasm in the total proportion of bronchial obstruction, ventilation and respiratory mechanics are studied after a series of pharmacological tests. After inhalation of bronchodilator aerosols, ventilation performance improves in the presence of a spastic component of airway obstruction. Radiopulmonography using the radioactive isotope 133Xe is performed to detect uneven ventilation associated with obstruction of the small bronchi. This is the earliest diagnostic sign of this type of bronchial obstruction. Electrocardiography is necessary to detect hypertrophy of the right ventricle and right atrium developing in pulmonary hypertension. A pronounced deviation of the QRS axis to the right, a shift of the transition zone to the left (R / S < 1 in V4-V6), S-type ECG are detected; high sharp P wave in leads VF, III, II. A clinical blood test reveals secondary erythrocytosis resulting from chronic hypoxia with the development of severe pulmonary insufficiency. "Acute phase" indicators are expressed moderately: ESR is normal or moderately increased, leukocytosis is small, as well as the shift of the leukocyte formula to the left. As evidence of allergic manifestations, eosinophilia is possible. The study of sputum and bronchial contents helps to establish the severity of inflammation. With severe inflammation, the contents are purulent or purulent-mucous, contain many neutrophils and single macrophages, dystrophically altered cells of the ciliated and squamous epithelium are poorly represented. For moderate inflammation, the contents are closer to mucopurulent; the number of neutrophils is reduced, the number of macrophages, mucus and bronchial epithelial cells increases. With mild inflammation, the bronchial contents are mucous, desquamated cells of the epithelium and bronchi predominate; macrophages and neutrophils are few. Microbiological examination of sputum and bronchial contents is important to identify the etiology of exacerbation of chronic bronchitis and the choice of antimicrobial therapy. Differential diagnostics. Table 10 Differential diagnostic criteria for CB
Treatment. Includes a set of measures that differ during the period of exacerbation and remission of the disease. During the period of exacerbation of chronic disease, two directions of treatment are distinguished: etiotropic and pathogenetic. Etiotropic treatment is aimed at eliminating the inflammatory process in the bronchi: therapy with antibiotics, sulfanilamide drugs, antiseptics, phytoncides, etc. is indicated. Treatment is started with antibiotics of the penicillin series (penicillin, ampicillin) or a group of cephalosporins (cefamesin, tseporin), and in the absence of effect, antibiotics of the group are used reserve (gentamicin, etc.). The most preferred route of administration is intratracheal (aerosol or fill with a laryngeal syringe through a bronchoscope). Pathogenetic treatment is aimed at improving pulmonary ventilation; restoration of bronchial patency; control of pulmonary hypertension and right ventricular failure. The restoration of pulmonary ventilation, in addition to the elimination of the inflammatory process in the bronchi, is facilitated by oxygen therapy and exercise therapy. The main thing in the treatment of chronic bronchitis - the restoration of bronchial patency - is achieved by improving their drainage and eliminating bronchospasm. To improve bronchial drainage, expectorants are prescribed (hot alkaline drink, decoctions of herbs, mukaltin, etc.), mucolytic drugs (acetylcysteine, bromhexine; with purulent viscous secretion - aerosols of proteolytic enzymes - chymopsin, trypsin); therapeutic bronchoscopy is used. To eliminate bronchospasm, eufillin is used (intravenously, in suppositories, tablets), ephedrine, atropine; single appointments in an aerosol of sympathomimetic drugs are possible: fenoterol, orciprenaline sulfate (asthmopenta) and a new domestic drug "Soventol", anticholinergic drugs: atrovent, troventol. Effective preparations of prolonged aminophylline (teopec, teodur, theobelong, etc.) - 2 times a day. In the absence of the effect of such therapy, small doses of corticosteroids are administered orally (10-15 mg of prednisolone per day) or intratracheally (hydrocortisone suspension - 50 mg). As an additional therapy, appoint: 1) antitussive drugs: with an unproductive cough - libexin, tusuprex, bromhexine, with a hacking cough - codeine, dionin, stoptussin; 2) drugs that increase the body's resistance: vitamins A, C, group B, biogenic stimulants. Currently, in the treatment of chronic bronchitis, immunocorrective drugs are increasingly being used: T-activin or thymalin (100 mg subcutaneously for 3 days); inside - catergen, sodium nucleinate or pentoxyl (within 2 weeks), levamisole (decaris). Physiotherapy treatment: prescribe diathermy, calcium chloride electrophoresis, quartz on the chest area, chest massage and breathing exercises. With moderate and severe bronchitis, along with anti-relapse and sanatorium treatment, many patients are forced to constantly receive supportive drug treatment. Maintenance therapy is aimed at improving bronchial patency, reducing pulmonary hypertension and combating right ventricular failure. The same drugs are prescribed as in the period of exacerbation, only in smaller doses, in courses. Forecast. The prognosis for complete recovery is unfavorable. The least favorable prognosis is for obstructive CB and CB with predominant damage to the distal bronchi, which quickly leads to the development of pulmonary failure and the formation of cor pulmonale. The most favorable prognosis is for superficial (catarrhal) CB without obstruction. LECTURE No. 8. Diseases of the respiratory system. Pneumonia Pneumonia is an acute infectious and inflammatory disease of a focal nature, in which the respiratory sections and interstitial connective tissue of the lungs are involved in the pathological process. Classification by E. V. Gembitsky (1983). By etiology: 1) bacterial (indicating the pathogen); 2) viral (indicating the pathogen); 3) cornitic; 4) rickettsial; 5) mycoplasma; 6) fungal; 7) mixed; 8) infectious-allergic; 9) unknown etiology. By pathogenesis: 1) primary (independent acute inflammatory process); 2) secondary (complication of diseases of the cardiovascular system with circulatory disorders in the pulmonary circulation, chronic diseases of the kidneys, blood systems, metabolism, infectious diseases or develop against the background of chronic respiratory diseases). Clinical and morphological characteristics: 1) parenchymal (for pneumococcal pneumonia): croupous; focal; 2) interstitial. By localization and extent: unilateral; bilateral. By severity: extremely severe; heavy; moderate; mild and abortive. Downstream: sharp; protracted (radiological and clinical resolution of pneumonia). Etiology. Most pneumonia is of infectious origin. Allergic pneumonia and those caused by physical or chemical factors are rare. Bacterial pneumonia is diagnosed more often in middle-aged and elderly people; viral pneumonia - in young people. In the etiology of primary bacterial pneumonia, the leading role belongs to pneumococci. During an influenza epidemic, the role of viral-bacterial associations (usually staphylococci), as well as opportunistic microorganisms, increases. In secondary pneumonia, the leading etiological role is played by gram-negative bacteria (klebsiella pneumoniae and influenza bacillus); in the occurrence of aspiration pneumonia, the importance of anaerobic infection is great. Pathogenesis. The infectious pathogen enters from the outside into the respiratory sections of the lungs through the bronchi: inhalation and aspiration (from the nasopharynx or oropharynx). By hematogenous route, the pathogen enters the lungs mainly during secondary pneumonia or during the thrombotic genesis of pneumonia. Lymphogenous spread of infection with the occurrence of pneumonia is observed only with wounds to the chest. There is also an endogenous mechanism for the development of inflammation in the lung tissue, due to the activation of the microflora in the lungs. Its role is great in secondary pneumonia. The development of pneumonia is facilitated by unfavorable factors of the external and internal environment, under the influence of which there is a decrease in the general nonspecific resistance of the body (suppression of phagocytosis, the production of bacteriolysins, etc.) and suppression of local defense mechanisms (impaired mucociliary clearance, a decrease in the phagocytic activity of alveolar macrophages and neutrophils, etc.) . Significant importance in the pathogenesis of pneumonia is also attached to allergic and autoallergic reactions. Saprophytes and pathogenic microorganisms, becoming antigens, contribute to the production of antibodies that are fixed on the cells of the mucous membrane of the respiratory tract, where the antigen-antibody reaction occurs, which leads to tissue damage and the development of the inflammatory process. In the presence of common antigenic determinants of microorganisms and lung tissue, or when lung tissue is damaged by viruses, microorganisms, toxins and toxic substances, leading to the manifestation of its antigenic properties, autoallergic processes develop. These processes contribute to a longer existence of pathological changes and a protracted course of the disease. clinical picture. Main syndromes: 1) intoxication (general weakness, fatigue, headaches and muscle pain, shortness of breath, palpitations, pallor, loss of appetite); 2) a syndrome of general inflammatory changes (feeling hot, chills, fever, changes in acute phase blood counts: leukocytosis with a shift of the leukocyte formula to the left, an increase in ESR, fibrinogen level, α2-globulins, the appearance of C-reactive protein); 3) a syndrome of inflammatory changes in the lung tissue (appearance of cough and sputum, shortening of percussion sound), increased voice trembling and bronchophony, changes in the frequency and nature of breathing, the appearance of moist rales, radiological changes; 4) syndrome of involvement of other organs and systems. The severity of these manifestations characterizes the severity of the course of pneumonia (see Table 11). Table 11 Symptoms and course of pneumonia
At various stages of the course of pneumonia, the clinical picture may change from the addition of certain complications: pulmonary and extrapulmonary. Pulmonary: abscess formation; pleurisy (para- and metapneumonic), less often - pleural empyema; accession of an asthmatic component, the formation of pulmonary edema and the development of acute respiratory failure is possible. Extrapulmonary complications: infectious-toxic shock (with symptoms of acute vascular, acute left ventricular and renal failure, ulceration of the mucous membrane of the digestive tract and bleeding, the development of disseminated intravascular coagulation; infectious-allergic myocarditis; infective endocarditis; pericarditis; meningitis or meningoencephalitis; nephritis; hepatitis In severe croupous pneumonia, intoxication psychoses may develop, and in confluent total pneumonia - acute pulmonary heart. The main complaints of a patient with pneumonia: cough, sputum production, chest pain, aggravated by breathing and coughing, shortness of breath, impaired general well-being, fever. Cough may be dry or with sputum (mucous, mucopurulent, purulent-mucous, bloody). "Rusty" sputum is characteristic of lobar pneumonia, bloody - for pneumonia caused by Klebsiella (Fridlander's bacillus) and viral pneumonia; purulent bloody sputum indicates pneumonia of streptococcal origin. Persistent cough with a small amount of mucopurulent sputum is observed with mycoplasmal pneumonia, which is also characterized by a feeling of soreness in the throat. Pain in the side, aggravated by deep breathing and coughing, is characteristic of lobar pneumococcal pneumonia, as well as involvement of the pleura in the pathological process. With the localization of pneumonia in the lower parts of the lungs and the involvement of the diaphragmatic pleura in the process, the pain can radiate to the abdominal cavity, simulating a picture of an acute abdomen. If the upper or lower reed segment of the left lung is involved in the process, the pains are localized in the region of the heart. In 25% of patients, the complaint of shortness of breath is one of the main ones, especially with pneumonia that developed against the background of chronic respiratory diseases and heart failure. The severity of shortness of breath increases in parallel with the violation of general well-being. Symptoms of severe intoxication are most characteristic of cornitosis and mycoplasmal pneumonia, and are also observed in staphylococcal, influenza and pneumococcal (croupous) pneumonia. The patient may be disturbed by chills and an increase in body temperature to febrile. Against the general background of intoxication and febrile temperature, local symptoms appear. Diagnostics. To make an etiological diagnosis, a correct assessment of the symptoms of the disease at its very beginning is important. Hoarseness or inability to speak is characteristic of pneumonia caused by the parainfluenza virus. Lachrymation, pain in the eyes, sore throat when swallowing, copious discharge from the nose without changing other parts of the respiratory tract occur with pneumonia caused by adenovirus. The most significant for the diagnosis is the presence of a syndrome of inflammatory changes in the lung tissue. This syndrome consists of the following symptoms: 1) lag in breathing of the affected side of the chest; 2) shortening of percussion sound in the area of the projection of the lesion over a greater or lesser extent; 3) increased voice trembling and bronchophony in the same area; 4) change in the nature of breathing (hard, bronchial, weakened, etc.); 5) the appearance of pathological respiratory noises (wet, voiced fine bubbling rales and crepitus). The nature of breathing can change in different ways. In the initial stage of croupous pneumonia, breathing can be weakened, with an extended exhalation; in the hepatization phase, along with an increase in the dullness of the percussion sound, bronchial breathing is heard; with the resolution of the pneumonic focus with a decrease in percussion dullness, breathing becomes hard. With focal pneumonia, the most constant symptoms are hard breathing and moist, ringing fine bubbling rales. However, with central hilar pneumonia, physical data are presented very poorly, and recognition of pneumonia is possible only after an X-ray examination. Mycoplasma pneumonias are distinguished by the scarcity of physical data. Severe intoxication, combined with a very small number of wheezing, is observed in pneumonia caused by Klebsiella pneumonia. In some cases, during auscultation, a large number of bass and treble dry rales, uncharacteristic of the inflammatory infiltration syndrome, may come to the fore. This occurs with pneumonia that has developed against the background of chronic bronchitis; pneumonia caused by Pfeiffer's stick; in case of accession to pneumonia of an allergic component. Symptoms help to make an etiological diagnosis: 1) the detection of a small-spotted, as with rubella, rash in combination with lymphadenopathy is characteristic of adenovirus infection; 2) local enlargement of the lymph nodes indicates perifocal pneumonia; 3) fungal pneumonia combined with lesions of the mucous membranes, skin and nails; 4) hepatolienal syndrome and slight jaundice are found in cornitic and Curickettsial pneumonias; 5) for typical croupous pneumonia, the appearance of the patient is characteristic: a pale face with a feverish blush on the side of the lesion, herpetic eruptions, swelling of the wings of the nose when breathing. The most important method to clarify the presence of pneumonia and the degree of involvement of the lung tissue in the process is large-frame fluorography and X-ray examination of the chest organs. Staphylococcal pneumonias are distinguished by a clear segmentation of lung lesions with the involvement of several segments in the process. Their characteristic radiological sign is the formation of multiple cavities in the lungs of the pneumocele type on the 5-7th day from the onset of the disease, and later - necrotic cavities with the presence of fluid. Unlike true abscesses, the configuration and number of cavities change rapidly. Lobar lesion is a manifestation of croupous pneumonia or pneumonia caused by Klebsiella. The upper lobe, mainly the right lung, is most commonly affected. X-ray examination reveals an effusion in the pleural cavity. Often such an effusion occurs with streptococcal pneumonia, with pneumonia caused by Pfeiffer's stick, which is localized in the lower lobe and in 2/3 of patients captures more than one lobe of the lung. X-ray examination data are especially important in detecting pneumonia with mild auscultatory changes (interstitial and hilar pneumonia). In some cases, to clarify the diagnosis, tomography and bronchography are indicated, which help to clarify the diagnosis in cases of delayed regression of infiltrative changes, with a complicated course (abscess, effusion in the pleural cavity). They are used to exclude other pathological processes with similar clinical and radiological presentations. Bronchography reveals decay cavities in the lung tissue, as well as the presence of bronchiectasis, around which infiltrative changes (perifocal pneumonia) are possible during exacerbation. In the diagnosis of infarct pneumonia, a radionuclide study of pulmonary blood flow plays a certain role, revealing its violations. Bacteriological examination of sputum (or bronchial washings) before the appointment of antibiotics helps to detect the pathogen and determine its sensitivity to antibiotics. Not always identified microorganism is the causative agent of pneumonia. A more precise etiological diagnosis can be made using immunological studies: complement fixation reaction (RCC) and hemagglutination inhibition reaction (HITA) with viral and bacterial antigens. In the diagnosis of viral and viral-bacterial pneumonia, virological and serological studies are important (the results of a culture study of sputum, including a biological test on mice, a method of cultivating viruses in a developing chicken embryo, an immunofluorescence method, a serological method using paired sera against viruses, attach importance to only 4 -fold increase in antibody titer). Sputum examination helps to clarify the nature of pneumonia. A large number of eosinophils indicates allergic processes, the presence of atypical cells indicates pneumonia of cancerous origin; Mycobacterium tuberculosis is found in tuberculosis; elastic fibers - evidence of the collapse of lung tissue. With mycosis pneumonia, along with the detection of fungi, there is a lack of pyogenic flora due to the inhibitory effect of the waste products of fungi. According to the microscopy of Gram-stained sputum smears, we can talk about Gram-negative or Gram-positive microorganisms that live in the bronchi already on the first day of the patient's stay in the hospital. The severity of the inflammatory process is judged by the severity of acute-phase blood parameters and their dynamics (leukocytosis with a shift in the leukocyte formula, an increase in ESR, an increased content of α2-globulins, fibrinogen, the appearance of SRV, an increase in the level of sialic acids). With a prolonged course of pneumonia and the development of complications, the immunological reactivity of the body is studied. A decrease in humoral (IgM) and cellular (delayed migration of leukocytes, changes in tests characterizing the T-lymphocyte system) immunity requires immunomodulatory therapy. Treatment. Immediately after diagnosis, it is necessary to begin etiotropic therapy for pneumonia. Empirical ideas about a possible pathogen are of great importance, since bacteriological examination of sputum is carried out for quite a long time and in most patients, even with a modern approach to this study, gives uncertain and sometimes erroneous results. At the moment, penicillins have lost their importance as the drug of choice in the treatment of pneumonia. This is due to the fact that etiologically significant for the development of pneumonia, in addition to pneumococcus and Haemophilus influenzae, are obligate intracellular microorganisms - Mycoplasma pneumoniae and Chlamydia pneumoniae, which are resistant to the bactericidal effects of antibiotics of the β-lactam group. It is impossible to lose sight of the fact that hypersensitivity to these drugs quickly develops in patients. In connection with the above, in the treatment of pneumonia, much attention is paid to macrolides, which have proven effective not only against pneumococcus, but also against Mycoplasma pneumoniae, Chlarnydia pneumoniae. However, it is important not to lose sight of the fact that erythromycin, which is the standard of this group of drugs due to its low stability in an acidic environment (and hence low bioavailability), as well as the widespread prevalence of pneumococcal strains resistant to erythromycin, is losing its clinical value. meaning. As drugs of choice, it was replaced by other drugs of the macrolide class - azithromycin, roxithromycin, rovamycin, etc. A number of macrolides are also used for oral and parenteral use (for example, rovamycin). As a result, their use is justified in the severe course of the inflammatory process in the lung (for example, initially rovamycin is administered intravenously for 2-3 days, and subsequently, with a positive dynamics of the pathological process, the patient switches to taking this drug inside). The advantage of rovamycin is undeniable, since it does not interact with theophyllines, while preventing the possibility of an overdose of these drugs, since theophyllines and rovamycin are used together in the treatment of patients with chronic obstructive pulmonary diseases. It is also known that this subgroup of macrolides (16-membered macrolides) are drugs with a minimum level of side effects. In patients over 65 years of age, due to the heterogeneity of the etiological spectrum of pneumonia and with concomitant chronic obstructive pulmonary diseases, semi-synthetic penicillins can be used for initial antibiotic therapy, and in the absence of a positive effect after this therapy for 3-4 days, the use of cephalosporins is justified. It is important to recall that the spectrum of action of I and some II generation cephalosporins is gram-positive and gram-negative microorganisms, and III generation cephalosporins act mainly on gram-negative pathogens. I generation cephalosporins are represented by cephalothin (keflin), cefazolin (kefzol), etc. II generation drugs include cefuroxime (ketocef), cefoxitin (boncefin) and others. III generation cephalosporins: cefotaxime (claforan), cefoperazone (cefobid), ceftriaxone (longacef ). Aspiration pneumonia is associated with anaerobic or gram-negative microflora, which determines the use of aminoglycosides or III generation cephalosporins in combination with metronidazole-semisuccinate (500 mg intravenously 2-3 times a day). Immunodeficiency states also affect the nature of the selected drugs, which in this case depends on the nature of the pathogen. In such cases, the applied scheme consists of aminoglycosides and modern cephalosporins. The duration of effective antibiotic therapy for a patient with pneumonia is 7-10 days. When prescribing treatment, it should be taken into account that in 7-15% of cases there may be no effect from this therapy. This indicates the need to replace antibiotics, based on the results of a microbiological study. Another option is the use of alternative drugs, the so-called second-choice antibiotics: modern cephalosporins, imipenem, monobactams, fluoroquinolones. Fluoroquinolones (ofloxacin, pefloxacin, ciprofloxacin) are effective against gram-negative pathogens, including Pseudomonas aeruginosa, and some gram-positive cocci (Staphylococcus aureus), but are inactive when exposed to anaerobes. Fluoroquinolones can justifiably be considered as an alternative to macrolides in chlamydia, legionella and mycoplasma infections. Monobactam antibiotics in their modern form are represented by aztreonam (azactam), which is active mainly against gram-negative aerobes (Salmonella, Shigella, Proteus, Escherichia coli, Klebsiella, etc.); and is also stable under the action of β-lactamases. Imipenem - an antibacterial drug of the carbapenem group, is prescribed only in combination with cilastatin, which inhibits the metabolism of imipenem. The drug is highly effective against many anaerobes, gram-positive cocci and gram-negative rods. Dosing of antibiotics used in the treatment of pneumonia. 1) Penicillins: benzylpenicillin (500-000 IU intravenously every 1-000 hours or 000-6 IU every 8 hours intramuscularly), ampicillin (500-000-1 g intramuscularly every 000-000 hours or 4 g every 0,5 hours intravenously), amoxicillin (1,0-2,0 g every 6 hours orally or 8-0,5 g every 6-0,5 hours intramuscularly, intravenously), oxacillin ( 1,0 g every 8-0,5 hours orally, intramuscularly, intravenously). 2) Cephalosporins: I generation - cephalothin (keflin) (0,5-2,0 g every 4-6 hours intramuscularly, intravenously), cefazolin (kefzol) (0,5-2,0 g, every 8 hours intramuscularly, intravenously ), II generation - cefuroxime (zinacef, ketocef) (0,75-1,5 g every 6-8 hours intramuscularly, intravenously), III generation - cefotaxime (claforan) (1,0-2,0 g, maximum up to 12 g / day every 12 hours intramuscularly, intravenously), ceftriaxone (longacef, rocefin) (1,0-2,0-4,0 g every 24 hours intramuscularly, intravenously). 3) Aminoglycosides: genetamycin (80 mg every 12 hours intramuscularly, intravenously), amikacin (10-15 mg/kg every 12 hours intramuscularly, intravenously), tobramycin (brulamycin) (3-5 mg/kg every 8 hours intramuscularly, intravenously) . 4) Macrolides: erythromycin (0,5 g every 6-8 hours orally or 0,5-1,0 g every 6-8 hours intravenously), rovamycin (3,0 million IU every 8-12 hours orally or 1,5. 3,0-8 million IU every 12-XNUMX hours IV). 5) Fluoroquinolones: pefloxacin (leflacin) (400 mg every 12 hours orally, IV), ciprofloxacin (cyprobay) (500 mg every 12 hours orally or 200-400 mg every 12 hours intravenously), ofloxacin (zanocin, tarivid) (200 mg every 12 hours orally). 6) Tetracyclines: doxycycline (vibramycin) (200 mg on day 1, on subsequent days - 100 mg every 24 hours orally), minocycline (minocin) (200 mg on day 1, on subsequent days - 100 mg every 12 hours orally), aztreonam (azactam) (1,0-2,0 g every 8-12 hours), imipenem/cilstatin (thienam) (500 mg every 6-8 hours intramuscularly). It is also significant that, as a rule, a protracted or progressive course of the disease is due to inadequate initial antibiotic therapy. However, in addition to this, there are a number of local and systemic causes that lead to a long and persistent course of inflammation in the lungs: these are local airway obstruction (cancer, adenoma, mucoid blockage, etc.); bronchiectasis (congenital, acquired); cystic fibrosis; immune system defects (acquired); recurrent aspiration (achalasia, esophageal cancer, etc.); activation of latent tuberculosis infection; developing lung abscess; inadequate antibiotic therapy. LECTURE No. 9. Diseases of the digestive tract. Diseases of the esophagus. Esophagitis and peptic ulcer of the esophagus 1. Acute esophagitis Acute esophagitis is an inflammatory lesion of the mucous membrane of the esophagus lasting from several days to 2-3 months. Etiology and pathogenesis. Etiological factors: infectious diseases, injuries, burns, poisoning, allergic reactions, nutritional errors. Of the infectious agents, the most characteristic of acute esophagitis are diphtheria, scarlet fever, typhoid and typhus, influenza, parainfluenza, adenovirus infection, mumps. Physical and chemical damaging factors are represented by ionizing radiation, chemical burns, hot and very cold food, and spices. Classification. There is no single classification. It is possible to use a working classification of acute esophagitis. Morphologically, the listed types of acute esophagitis are distinguished: catarrhal, edematous, erosive, pseudomembranous, hemorrhagic, exfoliative, necrotic, phlegmonous. By etiology: infectious, chemical, physical, alimentary. By endoscopic stages: 1st - edema and hyperemia of the mucosa, 2nd - the appearance of single erosions on the tops of the edematous mucosal folds, 3rd - significant edema and hyperemia of the mucosa with foci of eroded and bleeding mucous membranes, 4th - "weeping "- diffusely eroded mucous membrane, bleeds at the slightest touch of the endoscope. clinical picture. Catarrhal esophagitis is the most common form of acute esophagitis. It occurs against the background of errors in nutrition: when eating spicy, cold, hot foods, with minor injuries, alcohol burns. It is clinically manifested by burning and pain behind the sternum, forcing patients to refuse food for several days. Endoscopically noted esophagitis I-II degree, x-ray - hyperkinesia of the esophagus. Erosive esophagitis occurs with infectious diseases (finn, typhus, sepsis, fungal processes) and allergies. It also appears with chemical burns and injuries of the esophagus. In fact, this form of esophagitis is a phase of the evolution of catarrhal esophagitis. The main clinical picture consists of the symptoms of the underlying disease. Clinical symptoms are similar to those of catarrhal esophagitis: significant pain in the chest during the passage of food; heartburn, belching, hypersalivation, putrid odor from the mouth (cacosmia). Endoscopically ascertain signs of esophagitis II-III degree. Histological examination revealed hyperemia, mucosal edema, hemorrhage, erosion. An X-ray examination shows an abundance of mucus in the esophagus, a restructuring of the relief with the formation of flat depots of barium of a longitudinal shape up to 1 cm long, and hyperkinesia of the walls of the esophagus. Hemorrhagic esophagitis is a rare clinical form of erosive esophagitis. The etiology is the same as in erosive esophagitis. Intense pain syndrome and hematemesis are clinically typical. Endoscopy reveals grade III-IV inflammation with a predominance of the hemorrhagic component. There is a detachment of the bleeding mucous membrane in the form of narrow thin strips. Fibrinous (pseudomembranous) esophagitis. Etiological factors in it are scarlet fever, diphtheria, blood diseases, fungal diseases, the effects of radiation therapy. The clinic is dominated by dysphagia and intense pain, aggravated after eating, nausea, vomiting. With vomit, fibrin films are released, there may be hemoptysis. Endoscopically, on the affected areas of the mucosa, gray and yellow-gray fibrinous plaques are found, formed by layers of fibrin and detritus covering the surface of the mucosa. With the rejection of pseudomembranes, flat slowly healing erosions are formed, sometimes bleeding ulcers. After a severe infectious process, membranous stenoses remain in the esophagus, which disappear after repeated bougienage. Membranous (exfoliative) esophagitis by etiology is chemical (burns of the esophagus), infectious (causes are sepsis, shingles, smallpox, generalized herpes infection). The clinic of the disease is variable - from mild forms, diagnosed endoscopically, to severe ones. In the clinic of severe membranous esophagitis, intoxication, dysphagia and pain syndrome prevail. Possible bleeding, perforation of the esophagus, mediastinitis, which, as a rule, end in death. In endoscopic examination, damage to all layers of the esophagus is observed, the epithelium of which is rejected by layers. When the underlying disease subsides, symmetrical and asymmetric membranous or rough cicatricial stenoses sometimes remain in the esophagus. Necrotizing esophagitis is a rare form of acute inflammation of the esophagus. Its development is facilitated by reduced immunity in such serious diseases as sepsis, typhoid fever, candidiasis, end-stage renal failure. The clinic is characterized by painful dysphagia, vomiting, general weakness, bleeding, frequent development of mediastinitis, pleurisy, pneumonia. After the treatment of the underlying disease, strictures remain in the esophagus, diagnosed as facultative precancerous changes. Septic esophagitis is a rare local or diffuse inflammation of the walls of the esophagus of streptococcal etiology or occurs when the mucosa is damaged by a foreign body, with burns, ulcerations, and can pass from neighboring organs. Sometimes acute phlegmonous esophagitis occurs as a complication of any form of acute esophagitis, leading to purulent fusion of the walls of the esophagus. The collapse of the walls is accompanied by a breakthrough of pus into the tissue of the mediastinum, the development of mediastinitis, pleurisy, purulent bronchitis, pneumonia, spondylitis, rupture of the aorta or other great vessels. Accession of an anaerobic infection can lead to mediastinal emphysema or spontaneous pneumothorax. The clinical picture is characterized by severe intoxication, high fever, pain behind the sternum and in the neck, vomiting. On examination, there is swelling in the neck, mobility in this part of the spine is limited. The position of the head is forced, with an inclination to one side. The disease often transforms into purulent mediastinitis. In blood tests - hyperleukocytosis, accelerated ESR. Instrumental examination (X-ray, endoscopic) in the acute stage is not indicated. During the period of scarring, an x-ray examination is mandatory due to the risk of developing gross deformities and cicatricial stenosis of the esophagus. Treatment. Principles of treatment of acute esophagitis: etiotropic, pathogenetic and symptomatic. Etiotropic treatment - treatment of the underlying disease. In infectious diseases complicated by acute esophagitis, antibiotics are used (parenterally). With pronounced necrotic and hemorrhagic changes in the esophagus, it is recommended to refrain from eating for 2-3 weeks. During this period, parenteral nutrition, intravenous administration of protein hydrolysates, mixtures of amino acids, intralipid, vitamins, and detoxification therapy are indicated. After reducing inflammation, thermally and chemically sparing foods are prescribed: warm milk, cream, vegetable soups, liquid cereals. To reduce local symptoms of inflammation - inside solutions of tannin 1%, collargol - 2%, novocaine - 1-2% before meals. Astringents are taken in a horizontal position with the head of the bed lowered low. In the absence of the effect of local administration of astringent preparations, non-narcotic analgesics are prescribed parenterally. To reduce the effects of esophageal dyskinesia, prokinetic drugs (cerucal, raglan, cisapride) are used orally before meals. With multiple erosions, bismuth preparations (denol, vikair), injections of solcoseryl are indicated. With hemorrhagic esophagitis, complicated by bleeding, aminocaproic acid preparations, vikasol, dicynone are used. With massive bleeding, a blood or plasma transfusion is prescribed. With purulent, necrotic esophagitis, the patient should be on parenteral nutrition for a long time, massive therapy with several antibiotics is used, and the abscess is drained. Esophageal strictures are corrected by bougienage. In rare cases, a gastrostomy is placed. Forecast. The prognosis for catarrhal and erosive esophagitis is favorable. Spontaneous disappearance of the symptoms of esophagitis is possible provided that the underlying disease is adequately corrected. The prognosis of pseudomembranous, ecfoliative, and phlegmonous esophagitis is serious. In all cases, subject to recovery from the underlying disease, esophagitis ends with the formation of scar strictures, which subsequently require correction. Patients with severe forms of esophagitis complicated by esophageal strictures are unable to work. Prevention of acute esophagitis consists in adequate and timely diagnosis and treatment of the underlying disease. 2. Chronic esophagitis Chronic esophagitis is a chronic inflammation of the mucous membrane of the esophagus lasting up to 6 months. The most common variant is peptic esophagitis (reflux esophagitis), which can be complicated by peptic ulcer of the esophagus. Etiology and pathogenesis. The main cause of the disease is constant reflux of gastric contents into the esophagus, sometimes bile and intestinal contents, i.e. peptic esophagitis is an aseptic burn of the esophagus by stomach acid. In the pathogenesis of reflux esophagitis, regurgitation of acidic contents and a violation of the purification and emptying of the esophagus from it are important. The rate of clearance of the esophagus from chemical irritation is called esophageal clearance. With normal clearance, single reflux of aggressive secretions does not cause reflux esophagitis. Hot food, alcohol, smoking and other exogenous factors reduce the clearance of the esophagus. These factors include fast food, in which a significant amount of air is swallowed along with food. The quality of food also matters: fatty meat, lard, pasta, spicy spices help delay the evacuation of food from the stomach, followed by the reflux of the contents into the esophagus. Drugs significantly reduce the tone of the lower esophageal sphincter and promote reflux: calcium antagonists, nitrates, narcotic analgesics, anticholinergic drugs, theophylline and its analogues, drugs from the prostaglandin group. There are five criteria for the pathogenicity of reflux in the genesis of peptic esophagitis: frequency, volume, regurgitation, chemical composition, condition of the esophageal mucosa and sensitivity to a chemical factor (inflammation of the walls reduces sensitivity), emptying rate (clearance), which depends mainly on active peristalsis, alkalizing action saliva and mucus. The occurrence of reflux esophagitis is promoted by hernia of the esophageal opening of the diaphragm, duodenal ulcer, post-gastroresection disorders, and allergies. Allergic predisposition also matters. Morphological examination of patients with peptic esophagitis reveals edema, hyperemia of the mucosa, infiltration of the submucosa of the supradiaphragmatic segment of the esophagus. There are two options for the spread of chronic inflammation - total and local reflux esophagitis. With involvement in the process of more than 2/3 of the esophageal mucosa, the development of reflux tracheitis, reflux bronchitis is possible. At the top of the esophageal folds, erosions, small ulcers occur (in places of maximum irrigation with gastric contents). Chronic inflammation of the esophagus leads to spastic contracture and shortening of the organ. clinical picture. Typical signs of reflux esophagitis include a burning sensation behind the sternum, heartburn, regurgitation, which worsens when lying down, dysphagia, and the positive effect of taking antacids. Pain in the chest may occur after eating, reminiscent of angina pectoris. The occurrence of pain in reflux esophagitis is associated with peptic irritation of the esophageal wall and its spasms during regurgitation of acidic gastric contents, as well as with infringement of the prolapsed mucosa. Distinctive features of this pain: its long, burning character, localization in the xiphoid process, irradiation along the esophagus, less often to the left half of the chest, no noticeable effect from taking antacids, antispasmodics, increased in a horizontal position, especially after eating. Particular attention in clinical diagnosis should be given to minor symptoms of dysphagia, such as a feeling of a lump behind the sternum, a feeling of hot food passing through the esophagus. A sign of gradually beginning esophagitis may be salivation and the habit of drinking water with food. Physical examination of patients with reflux esophagitis does not provide diagnostically significant information. The complications of reflux esophagitis include bleeding, ulceration, strictures, shortening of the esophagus, and malignancy. Chronic reflux esophagitis can lead to the development of axial hiatal hernia. Diagnosis and differential diagnosis. The most valuable research method for this pathology is endoscopy, during which hyperemia, edema, and thickening of the folds of the mucous membrane are noted. A whitish coating covering the mucous membrane is reliable, which in the initial stages of the disease can be thin, barely noticeable, but with a long process - massive white or dirty gray. In some areas, against a background of white plaque, the bright red mucous membrane of the esophagus is often visible. In some cases, erosive and ulcerative defects in the form of stripes are detected. Changes in the mucous membrane can correspond to any of the four stages of esophagitis: from hyperemia to “crying” mucous membrane. With severe esophagitis, a lot of saliva and mucus accumulate in the lumen. pH-metry, unlike endoscopy, makes it possible to more objectively assess esophageal clearance. X-rays reveal gastroesophageal reflux. It is necessary to differentiate reflux esophagitis with peptic ulcer of the stomach and duodenum, coronary heart disease, chronic cholecystitis and pancreatitis. The leading symptom in the differential diagnosis is pain. Differentiation with peptic ulcer is helped by the absence of late and "hungry" pains in esophagitis, as well as data obtained from endoscopy of the esophagus and stomach. Coronary pain, in contrast to esophagitis, is characterized by a connection with physical and emotional stress, the effect of nitrates, signs of ischemia on the ECG, including those according to bicycle ergometry. Ultrasound data of the abdominal organs help to exclude the pathology of the gallbladder and pancreas as the cause of the pain syndrome. Treatment. Therapy for reflux esophagitis includes treatment of the diseases that caused it and the prescription of antireflux therapy. Patients are advised to avoid lifting weights, bending over. It is necessary to take the correct position during rest and sleep (the headboard is raised by 15-20 cm, at an angle of 30-50 °). It is recommended to normalize body weight, eat fractionally (the last meal - 3 hours before bedtime). Alcohol and spicy foods are excluded from the diet. Assign adsorbents and alkalizing drugs that have a protective effect on the mucous membrane. These substances include Venter, which is administered orally at a dose of 1 g (preferably in the form of a suspension) 30-40 minutes before meals 3 times a day and the 4th time on an empty stomach at bedtime. The course of treatment is 8-10 weeks. Almagel, phosphalugel, maalox, gastal have a similar effect. These drugs are used in the interdigestive period (1/2-2 hours after meals and at night) until complete remission occurs. Phosphalugel and Maalox are prescribed 1-2 packets 2-3 times a day, gastal - 2-3 tablets a day. Tea soda, a mixture of Bourget, white clay due to insufficient efficiency is not advisable to use. Enveloping and astringent action has bismuth nitrate 1 g 3-4 times a day. A high antireflux activity of a new antacid, topalkan, was noted. Mineral waters - "Borjomi", "Essentuki No. 4", "Jermuk", "Smirnovskaya" have an alkalizing effect. To reduce acidic gastric secretion, H blockers are prescribed.2histamine receptors (cimetidine, ranitidine, famotidine), Ka-K-ATPase inhibitors (omeprazole), a selective blocker of M-cholinergic receptors of parietal cells, its analogue buscopan. Cimetidine is prescribed 400 mg 2 times a day, ranitidine - 300 mg and famotidine - 40 mg once in the evening after dinner. Omeprazole is recommended for resistant forms of erosive and ulcerative reflux esophagitis. It is prescribed at 30-40 mg per day for 3-4 weeks. To normalize motor-evacuation disorders in reflux disease, metoclopramide (cerucal, raglan, perinorm, biomral), prepulsid (sizepride, motilium, domperidone, coordinax) are prescribed. Metoclopramide and its 2nd generation analogues increase the tone of the lower esophageal sphincter, reduce intragastric pressure, and accelerate evacuation from the stomach. Assign metoclopramide 1 tablet 3-4 times a day before meals or 2 ml intramuscularly 2 times a day. The drug is usually well tolerated. When using it, dry mouth, drowsiness, tinnitus are possible, which decrease after eating. Sizepride is a novel gastrointestinal prokinetic agent. It increases the tone of the lower esophageal sphincter, improves esophageal clearance, enhances the motor-evacuation function of the digestive tract, and suppresses pathological refluxes (gastroesophageal and duodenogastric). The drug, unlike metoclopramide, does not block donamine receptors, is not a direct stimulant of anticholinergic receptors, and is devoid of side effects inherent in cerucal and its analogues. It is prescribed orally at 5 or 10 mg 2-3 times a day. The course of treatment lasts from 2-3 weeks to 2-3 months. Cesapride with reflux esophagitis can be used as a monotherapy. Prognosis and prevention. The prognosis for life and work is favorable. In complicated cases, the prognosis is determined by the timeliness and quality of medical care. Patients with severe disease are assigned a disability group. Patients with chronic reflux esophagitis should be under the supervision of a gastroenterologist. Endoscopic and morphological studies are indicated at least 2 times a year due to the possibility of malignancy. 3. Peptic ulcer of the esophagus Peptic ulcer of the esophagus is an acute or chronic disease characterized by ulceration of the mucosa of the distal segment of the esophagus under the influence of active gastric juice. Etiology and pathogenesis. Chronic peptic ulcers of the esophagus are complications of reflux esophagitis and hiatal hernia. Their occurrence is facilitated by an internal short esophagus, focal metaplasia of the mucosa, heterotopia of the gastric mucosa into the esophagus, reflux disease with cardia insufficiency, diseases accompanied by frequent vomiting (post-vagotomy syndrome, afferent loop syndrome, chronic alcoholism). Acute ulcers of the esophagus are possible with pathological dryness of the esophageal mucosa (xerosis), drug allergies, the use of NSAIDs, fungal infections, viral infections, skin burns and diseases of the central nervous system. These ulcers are considered symptomatic. clinical picture. Some patients have a combined ulcerative lesion of the mucous membrane of the esophagus and gastroduodenal zone. Symptoms of a peptic ulcer of the esophagus resemble the clinical picture of peptic esophagitis: persistent heartburn, worsening after eating, when bending the body, in a lying position, regurgitation, pain when swallowing, and impaired passage of solid food occur. Complications typical of esophageal ulcers: perforation, bleeding, penetration, stricture. Bleeding is manifested by hematemesis, melena, hypochromic anemia, and a decrease in cardiac activity. Perforation of the esophagus is diagnosed extremely rarely. The clinical symptoms of perforation are indistinguishable from the symptoms of acute penetrating and non-penetrating mechanical injury by foreign bodies. Approximately 14% of esophageal ulcers penetrate into the surrounding tissues. Diagnosis and differential diagnosis. It is extremely difficult to suspect a peptic ulcer based on clinical symptoms. The diagnosis is verified during instrumental and laboratory studies. The most informative is x-ray and endoscopic examination. Radiologically, the ulcer appears as a niche in the supracardiac esophagus with slight perifocal edema of the mucous membrane. The esophagus in the area of the ulcer is spastically contracted, and a slight suprastenotic expansion is detected above it. The ulcer is accompanied by signs of hyperkinesia and reflux esophagitis, and symptoms of hiatal hernia are very common. Sometimes the ulcer resembles a small epiphrenic diverticulum, but the latter does not have a typical clinical course and is not combined with cardial insufficiency, hernia, or esophagitis. It is more difficult to distinguish a peptic ulcer of the esophagus from ulcerated endophytic cancer, which is accompanied by rigidity of the walls and relief of the mucous membrane, and an asymmetric shaft, by radiological signs. The most reliable information in the verification of peptic ulcer of the esophagus is provided by endoscopy and multiple biopsy from the edges of the ulcer. When advancing the endoscope to the peptic ulcer, signs of stage I-IV esophagitis, motor dysfunction of the esophagus, perifocal edema and hyperemia of the mucous membrane are revealed. An acute ulcer is usually round or oval, with steep edges, covered with a whitish or green coating. A chronic ulcer has a flat bottom with dense and uneven walls, gentle edges, purulent-fibrinous deposits, foci of granulations and cicatricial overlays. To exclude malignancy, 4-6 biopsies are taken from the edges of the ulcer. Endoscopic examination reveals single peptic defects, elongated along the axis of the esophagus. Their length varies within 1-10 cm, but more often does not exceed 1 cm. The ulcer is often shallow, its bottom is covered with a whitish coating. Hyperemia, mucosal edema and single erosions often reflect a moderate perifocal inflammatory reaction. After healing of a peptic ulcer, a rough linear or stellate scar or a rough diverticulum-like deformity of the wall and narrowing of the lumen remain in the esophagus. It is necessary to differentiate peptic ulcers of the esophagus with ulcerations of a specific nature (with tuberculosis, syphilis). In these situations, specific serological tests, the results of histological and bacteriological studies significantly help. The combination of the pathology of the esophagus with damage to the lungs and other organs makes it necessary to purposefully examine the patient in relation to a specific process. Treatment. Treatment includes a diet: mechanically and chemically gentle food is recommended, which is taken in small portions 5-6 times a day. To prevent reflux of contents from the stomach into the esophagus, the patient's position in bed should be with the head of the bed elevated. Medicines are taken lying down. Monotherapy is prescribed with a drug from one of the following pharmacological groups: antisecretory, including antacids and adsorbents, stimulants of the motor-evacuation function of the stomach (prokinetics), drugs - mucus simulators. Therapy is carried out for a long time - 1,5-3 months. Indications for surgical treatment - lack of healing within 6-9 months, complicated course (perforation, penetration, stenosis, bleeding). Prognosis and prevention. The course of the disease is relapsing. The prognosis for life and work is favorable. Periodic (1-2 times a year) examination on an outpatient basis by a gastroenterologist using endoscopy and biopsy is recommended. Seasonal (spring - autumn) prevention of reflux esophagitis is carried out. LECTURE No. 10. Diseases of the digestive tract. Diseases of the stomach. Chronic gastritis Chronic gastritis is a disease that is clinically characterized by gastric dyspepsia, and morphologically - by inflammatory and degenerative changes in the gastric mucosa, impaired cell renewal processes, and an increase in the number of plasma cells and lymphocytes in the mucous membrane's own membrane. Etiology and pathogenesis. At the present stage of development of gastroenterology, it has been established that the appearance of chronic gastritis is facilitated by the microbial expansion of Helicobacter pylori (HP), which causes antral gastritis in 95% of cases and pangastritis in 56% of cases. In turn, the so-called etiological factors for the occurrence of chronic gastritis can be attributed with a high degree of certainty to risk factors (irregular unbalanced diet, smoking, alcohol intake, hypersecretion of hydrochloric acid and pepsin). The leading role in the development of the disease also belongs to autoimmune mechanisms, accompanied by the accumulation of antibodies to the parietal cells of the gastric mucosa, aggravated heredity, as well as the use of drugs that have a damaging effect on the gastric mucosa. Classification. In 1990, at the IX International Congress of Gastroenterologists in Australia, a new systematization of chronic gastritis, called the Sydney system, was adopted. Histological bases of classification. 1) Etiology: chronic gastritis associated with HP, autoimmune, idiopathic, acute drug-induced gastritis. 2) Topography: antral, fundic, pangastritis. 3) Morphology: acute, chronic, special forms. Endoscopic basis of classification: 1) gastritis of the antrum of the stomach; 2) gastritis of the body of the stomach; 3) pangastritis; 4) changes in the gastric mucosa: edema, erythema, mucosal vulnerability, exudate, flat erosions, elevated erosions, fold hyperplasia, fold atrophy, visibility of the vascular pattern, supramucosal hemorrhages. clinical picture. Chronic gastritis is one of the most common diseases in the clinic of internal medicine. Its frequency among the world's inhabitants ranges from 28 to 75%. Chronic gastritis is more often manifested by symptoms of gastric dyspepsia and pain in the epigastric region. Rarely, it is asymptomatic. The pain is usually localized in the epigastric region. There is a clear connection between its occurrence with food intake and the localization of the inflammatory process in the stomach. In patients with gastritis of the subcardial and cardial sections of the stomach, pain in the epigastric region occurs 10-15 minutes after a meal, with pathology of the body of the stomach - 40-50 minutes after a meal. "Late", "hungry", pains are typical for gastritis of the output section of the stomach, or duodenitis. "Two-wave" pain - after eating and on an empty stomach - is observed with gastritis of the subcardiac and antrum. With a diffuse process, pain is localized in the epigastric region, occurs after eating and is of a pressing nature. They say about the asymptomatic course of gastritis when it is not possible to establish the relationship between pain in the epigastric region and the lesion, which occurs when it is endogenous in origin (gastritis becomes secondary to the pathology of other organs and systems). An equally important place in the clinical picture of chronic gastritis is dyspeptic syndrome: nausea, belching (sour, bitter, rotten), heartburn, constipation or diarrhea, unstable stools. With isolated antral gastritis, complaints of heartburn and constipation, arising from the hypersecretion of hydrochloric acid and pepsin, become paramount. With pangastritis with signs of severe atrophy, nausea, belching "rotten", unstable stools or diarrhea predominate, which is typical for hyposecretion of hydrochloric acid and pepsin. Persistent nausea is characteristic of secondary gastritis in chronic pancreatitis, chronic cholecystitis, occurring with hypomotor dyskinesia of the gallbladder. Diagnostics. Chronic gastritis lasts a long time, with an increase in symptoms over time. Exacerbations are provoked by nutritional disorders. The physical picture of chronic gastritis is rather poor. In 80-90% of patients during an exacerbation of the disease, an objective study determines only local pain in the epigastric region. When chronic gastritis is combined with duodenitis, cholecystitis or pancreatitis, localization of pain that is not typical for gastritis, but characteristic of the pathology of another organ, can be determined. General blood and urine tests, biochemical parameters of blood in patients with chronic gastritis do not differ from the corresponding parameters in healthy individuals. In a scatological study, there are no changes in the analyzes, or there may be signs of a digestive disorder. When studying the gastric contents of acid secretion by pH-metry, both signs of acid hypersecretion and a decrease in acid production are noted. Indicators of pepsin formation in chronic gastritis are more persistent and decrease against the background of persistent anacidity in diffuse organ damage. An x-ray examination is more likely to exclude other diseases of the stomach (ulcer, cancer), help in the diagnosis of Menetrier's disease than to confirm the diagnosis of chronic gastritis. Due to the paucity of clinical manifestations of the disease, as well as the non-specificity of laboratory tests, the diagnosis of chronic gastritis is based on the results of endoscopic and morphological studies. Endoscopy reveals changes in the gastric mucosa of varying severity: edema, erythema, mucosal vulnerability, exudate, flat erosions, raised erosions, hyperplasia or atrophy of the folds, visibility of the vascular pattern, submucosal hemorrhages. They speak of chronic gastritis with an increase in the number of plasma cells and lymphocytes in the own membrane of the mucous membrane (in contrast to acute gastritis, when polymorphonuclear leukocytes appear). In connection with the foregoing, the morphological identification of inflammation in gastritis may not coincide with the interpretation of the clinician's data. The activity of inflammatory changes in the gastric mucosa is assessed morphologically and morphometrically according to the degree of leukocyte infiltration of the lamina propria or epithelium. We must not lose sight of the fact that autoimmune gastritis is not active. Morphological changes (weak, moderate and severe) - inflammation, activity, atrophy, metaplasia - and the degree of HP contamination are quantified. Clinical manifestations characteristic of gastritis are also observed in other diseases of the digestive system, therefore, in the process of diagnosis, ultrasound of the abdominal cavity, a thorough endoscopic and morphological examination of the digestive organs are necessary. Differential diagnostics. The most difficult is the differential diagnosis of gastritis with functional diseases of the stomach, peptic ulcer of the stomach and duodenum, chronic cholecystitis and pancreatitis and stomach cancer. Functional diseases of the stomach, similar to chronic gastritis, can occur latently or be accompanied by pain and dyspeptic symptoms. They are characterized by a short duration, the presence of general neurotic symptoms that prevail in the clinical picture of the disease (such as weakness, fatigue, irritability, headache, unstable mood, sweating). With disorders of the function of the stomach, the pain does not depend on the quality of the food, or it occurs after the use of a strictly defined product. Often there is a syndrome of acidism (heartburn, sour eructation, sour taste in the mouth), which, unlike gastritis with increased secretory function, does not increase after eating, but with excitement, long breaks in food. Vomiting in functional pathologies of the stomach develops according to the mechanism of a conditioned reflex, brings relief to the patient and does not lead to a significant deterioration in the general condition. In chronic gastritis, it usually occurs during an exacerbation and does not bring relief to the patient. A frequent symptom of dysfunction of the stomach is a loud eructation of air. In chronic gastritis, it is associated with impaired digestion of food or gastric motility and may be acidic if secretion is preserved, or with the smell of rotten eggs if it is reduced. In the study of gastric secretion in gastritis, normal values of secretion are detected at the beginning of the disease, and in the future, a tendency to a decrease in the secretion of gastric juice. With functional diseases of the stomach, heterochilia is often observed. X-ray examination of the stomach makes it possible to confirm such forms of gastritis as rigid, angraal, giant hyperplastic, polyposis, and in case of violations of the motor-evacuation function of the stomach (gastroptosis, hypotension) indicates the functional nature of the disease. The most valuable research method for the differential diagnosis of chronic gastritis and functional diseases of the stomach is gastroscopy, which allows, in controversial cases, to ascertain changes in the gastric mucosa characteristic of gastritis or functional diseases of the stomach. The differential diagnosis of chronic gastritis with peptic ulcer is described in the next lecture. Gastric cancer has a very similar picture with gastritis with reduced secretory function. Early diagnosis of gastric cancer on the basis of clinical signs is difficult, especially in patients suffering from gastritis for a long time. Of great importance for the diagnosis of cancer are the appearance of persistent persistent pain, little dependent on food intake, unmotivated general weakness and fatigue, appetite perversion, as well as a progressive decrease in the patient's body weight. Detection of a tumor on palpation refers to the later stages of the cancer process. Symptoms such as a change in the patient's well-being, a rapid decrease in the acidity of gastric juice, a "deficiency" of hydrochloric acid, the appearance of atypical cells in the gastric juice, a positive reaction to occult blood in the feces should cause the doctor to suspect gastric cancer. Of decisive importance in the differential diagnosis are X-ray and gastroscopic studies with targeted biopsy of the gastric mucosa. In patients with chronic gastritis with reduced secretory function, X-ray examination reveals atrophy of its mucous membrane, which is also confirmed by gastroscopy. With targeted biopsy in such cases, structural changes and atrophy of the mucous membrane are revealed. For gastric cancer, X-ray examination is characterized by the presence of a filling defect, the absence of mucosal folds or a change in their nature, and the absence of peristalsis in certain areas. Endoscopy of the stomach makes it possible to detect a tumor at the earliest stage of its development, when the tumor is still within the gastric mucosa, and surgical treatment leads to recovery in more than 90% of cases. Chronic cholecystitis. In chronic cholecystitis, the pain is localized in the right hypochondrium and is dull in nature. With calculous cholecystitis, the pain is acute, colicky, radiating to the right subscapular region. The onset of pain is associated with eating fatty foods or jolting driving. In chronic gastritis, the pain in the epigastrium is diffuse, dull, there is no irradiation, it occurs immediately after eating dry food or in violation of the diet. With gastritis and cholecystitis, pain is accompanied by dyspeptic symptoms, but a feeling of heaviness in the epigastrium, fullness, belching of food or air, a metallic taste in the mouth are more characteristic of gastritis. Vomiting in chronic gastritis is rare. Objectively, in chronic cholecystitis, especially calculous, one finds tension in the anterior abdominal wall, hyperesthesia of the skin in the right hypochondrium, which is uncharacteristic of chronic gastritis. On palpation of the abdomen in the case of chronic cholecystitis, pain is noted in the localization of the gallbladder. Chronic gastritis is characterized by diffuse soreness. In patients with chronic cholecystitis, bile examination reveals an increase in the amount of mucus and leukocytes. Chronic gastritis is characterized by a normal picture of bile against the background of changes in the secretion and acidity of gastric juice, as well as other functions of the stomach (absorption, motor). X-ray examination of the gallbladder in patients with chronic cholecystitis reveals a change in its evacuation function, as well as stones. Chronic pancreatitis. In chronic pancreatitis, the pain is localized in the left half of the abdomen, radiating to the left subscapular region, to the lower back, and to the surrounding area. The occurrence of pain is associated with the consumption of abundant, often fatty foods, and alcohol. If chronic gastritis is characterized by a long, monotonous course of the disease, then in chronic pancreatitis it is stepwise. An objective examination in the case of chronic pancreatitis reveals hyperesthesia of the skin in the left hypochondrium, pain topographically corresponds to the location of the pancreas. In a laboratory study of pancreatic juice in chronic pancreatitis, a persistent change in alkalinity and enzymes is found: the level of diastase in the blood and urine may change, which is not the case with chronic gastritis. Radiologically, chronic pancreatitis is characterized by an increased reversal of the duodenal ring, a sharp increase in its major papilla (Frostberg's symptom), and sometimes the presence of areas of calcification of the pancreas. Intranosological diagnostics of various forms of chronic gastritis should also be carried out. Thus, the disease associated with HP clinically proceeds with symptoms of duodenal ulcers, and in some cases it can proceed latently. Endoscopic and morphological examination reveals antropylorhoduodenitis. Erosions in Helicobacter pylori gastritis are usually localized in the area of severe inflammation (anthropyloric zone of the stomach). Autoimmune chronic gastritis is clinically characterized by a feeling of heaviness in the epigastric region, an unpleasant aftertaste in the mouth, rotten belching, and nausea. Due to insufficient production of hydrochloric acid, diarrhea appears. In 10% of cases, against the background of autoimmune gastritis, symptoms are found B12- deficiency anemia: weakness, pallor of the skin and mucous membranes, brittle nails, in blood tests - hyperchromic megaloblastic anemia. Special forms of the disease include granulomatous, eosinophilic, hypertrophic (Menetrier's disease), lymphocytic gastritis. Granulomatous gastritis acts as an independent form of the disease or more often - one of the components of a more serious pathology (Crohn's disease, tuberculosis, sarcoidosis). The diagnosis is always confirmed by the results of histological examination of biopsy specimens of the gastric mucosa. Eosinophilic gastritis is extremely rare and is caused by systemic vasculitis. A history of allergic reactions is mandatory. Histological examination reveals eosinophilic infiltration of the gastric mucosa. Hypertrophic gastritis (Menetrier's disease) is clinically manifested by pain in the epigastric region and nausea. Some patients may experience weight loss due to diarrhea. In endoscopic, radiological and morphological studies, giant hypertrophied mucosal folds are found, resembling the convolutions of the brain. Lymphocytic gastritis is clinically asymptomatic; morphologically, this form is characterized by a pronounced infiltration of the gastric mucosa by lymphocytes. Treatment. Patients with gastritis need general medical measures: regular balanced nutrition, normalization of work and rest schedules, leveling out stressful situations in everyday life and work. Drug therapy is indicated only in the presence of clinical manifestations of chronic gastritis. Patients with gastritis associated with HP are treated with a peptic ulcer program (see next lecture). Individuals with autoimmune gastritis need vitamin B supplementation12 (500 mcg once a day subcutaneously for 1 days, followed by a repetition of courses of treatment), folic acid (30 mg per day), ascorbic acid (up to 5 g per day). If necessary, substitution therapy is carried out with enzyme preparations (mezim-forte, festal, enzistal, creon, pancitrate, acidin-pepsin). The pain syndrome is usually stopped by the appointment of antacids (maalox, almagel, gastal) or H-histamine receptor blockers (ranitidine, famotidine) in medium therapeutic doses. With special forms of gastritis, treatment of the underlying disease is necessary. Prognosis and prevention. The prognosis for life and work is favorable. Patients with chronic gastritis should be registered with a gastroenterologist. They are examined clinically and endoscopically with a biopsy at least once a year to exclude tumor transformation. The most dangerous in terms of cancerous degeneration are hypertrophic, diffuse atrophic gastritis with epithelial dysplasia. In erosive forms of the disease complicated by bleeding, as well as in the decompensated form of Menetrier's disease, the prognosis is determined by the timeliness and adequacy of surgical treatment. Prevention of gastritis is reduced to rational nutrition, compliance with the regime of work and rest, limiting the intake of NSAIDs. LECTURE No. 11. Diseases of the digestive tract. Diseases of the stomach. peptic ulcer Peptic ulcer (peptic ulcer) is a chronic, relapsing disease, clinically manifested by a functional pathology of the gastroduodenal zone, and morphologically - by a violation of the integrity of its mucous and submucosal layers, and therefore the ulcer always heals with the formation of a scar. Etiology. The main etiological factor of peptic ulcer disease is the microbial expansion of HP on the surface of the gastric epithelium. The significance of bacterial aggression in the etiology of the disease has been studied since 1983, when J. Warren and B. Marshall reported the discovery of a large number of S-spiral bacteria on the surface of the epithelium of the antrum of the stomach. Helicobacteria are able to exist in an acidic environment due to the production of the urease enzyme, which converts urea (from the bloodstream) into ammonia and carbon dioxide. The products of enzymatic hydrolysis neutralize hydrochloric acid and create conditions for changing the pH of the environment around each bacterial cell, thus providing favorable conditions for the vital activity of microorganisms. Total HP colonization occurs on the surface of gastric epithelial cells, which is accompanied by damage to the epithelium under the action of phospholipases. The latter provide the formation of toxic lecithins and proteinases from bile, causing the destruction of protective protein complexes and mucus. Against the background of "alkalinization" of epithelial cell membranes with ammonia, the membrane potential of the cells changes, the reverse diffusion of hydrogen ions increases, the death and desquamation of the epithelium of the gastric mucosa. All these changes lead to the penetration of HP into the depth of the gastric mucosa. No less important in the development of peptic ulcers are neuropsychic effects, hereditary predisposition, infectious agents, alimentary errors and the intake of certain medications, and bad habits. For the first time, the neurogenic concept of the onset of the disease was formulated by Bergman, who argued that hereditary-constitutional disorders of the autonomic nervous system lead to spasm of the muscles and blood vessels in the stomach wall, ischemia, and a decrease in the resistance of the mucous membrane to the aggressive effects of gastric juice. This theory was further developed by K. N. Bykov and I. T. Kurtsin (1952). They substantiated the corticovisceral theory of ulcerogenesis, which is based on data on changes in higher nervous activity resulting from chronic neuropsychic traumatization. Supplemented and detailed by the doctrine of the biochemical and hormonal links in the regulation of gastric secretion, motility and trophism, this theory of ulcerogenesis has again won many supporters in recent years. Popular among researchers are hereditary factors: the inertia of the main nervous processes, group-specific properties of blood, immunological and biochemical features, hereditary burden syndrome. In the occurrence of peptic ulcer, essential importance was attached to alimentary violations. However, clinical and experimental studies conducted in the last two decades in most cases did not reveal the damaging effect of food products on the gastroduodenal mucosa. The prevalence of peptic ulcer disease among significant contingents of people with different dietary habits also testifies against the leading importance of nutritional factors. Disturbances in the rhythm and regularity of nutrition, long breaks between meals, untimely eating are essential for the occurrence of peptic ulcers. Researchers have expressed relatively conflicting views about the role of alcohol in ulcerogenesis. Alcohol is known to cause atrophic changes in the gastric mucosa. These observations are in conflict with the general concept of ulceration. However, the frequent use of alcohol is accompanied by violations of the diet, qualitative changes in the composition of food, which ultimately can cause peptic ulcer of the stomach and duodenum. The role of medicinal effects in ulcerogenesis is being actively studied. The results of studies published in the literature and our own data indicate that non-steroidal anti-inflammatory drugs and glucocorticoid hormones have the most pronounced ulcerogenic properties. Pathogenesis. The pathogenesis of peptic ulcer disease is still not fully understood. When considering the processes of ulcerogenesis, it is necessary to highlight a number of postulates: 1) characterized by seasonality of exacerbations of peptic ulcer; 2) there is a predominant localization of peptic ulcers in the antropyloroduodenal zone; 3) the presence of hydrochloric acid and pepsin in gastric juice was noted; 4) a high frequency (up to 70%) of spontaneous healing of gastric and duodenal ulcers is noticeable; 5) there is chronic antral gastritis associated with HP; 6) the anthropyloric part of the stomach and the initial part of the duodenum are the "hypothalamus" of the gastrointestinal tract; 7) there is a hereditary predisposition to the occurrence of peptic ulcers; 8) the occurrence of an ulcer, its recurrence and remission are possible in the presence of all of the above factors. Thus, the unified concept of ulcerogenesis is as follows. In a patient with a hereditary predisposition to peptic ulcer in the presence of chronic bacterial gastritis during the period of autumn or spring dishormonosis, only hyperplasia and hyperfunction of endocrine cells secreting gastrin, histamine, melatonin and serotonin are noted. The main hormones and biogenic amines produced by the anthropyloruduodenal zone are involved both in stimulating gastric secretion and changing trophism and cell proliferation, primarily in this zone. Against the background of active bacterial gastritis and duodenitis, favorable conditions arise for ulcer formation. With the formation of a peptic defect, the functional activity of endocrine cells decreases. This leads to a decrease in acid-peptic aggression, an improvement in tissue trophism in the anthropyloroduodenal zone, and the creation of conditions for the healing of gastric and duodenal ulcers, even against the background of the ongoing microbial expansion of HP. In the acute period of peptic ulcer, hyperplasia of α-endorphin-producing cells, which are universal cytoprotectors, is noted. They act as the main protective mechanisms in peptic ulcers and provide the process of self-limitation of the ulcer and its healing, both directly and by stimulating the immune system. At the same time, antibodies against HP, synthesized in the submucosa of the stomach and duodenum, effectively bind to bacterial cells and neutralize HP toxins and contribute to their death. All of the above contributes to the creation of a balance between the so-called factors of aggression and protection factors and the healing of a peptic defect in the gastroduodenal zone. Classification. Classification (Panfilov Yu. A., Osadchuk M. A., 1991) Localization of the peptic defect: 1) gastric ulcer (subcardial and cardiac sections, pyloric part and pyloric canal, lesser and greater curvature); 2) duodenal ulcer (bulb and postbulbar section); 3) ulcers of the stomach and duodenum. The course of peptic ulcer. 1. Easy. The exacerbation of the ulcer is not more than 1 time in 1-3 years, the healing of the peptic defect ends by the 5-6th week from the start of the therapy, the severity of pain and dyspeptic syndromes is moderate. 2. Moderate. Recurrence at least 2 times a year, ulcer epithelialization - within 7-12 weeks, the severity of pain and dyspeptic syndromes. 3. Heavy. Remission periods do not exceed 3-4 months. In addition to severe pain, there are complications. Phases of the disease: 1) exacerbation of ulcer recurrence or functional disorders of the gastroduodenal system; 2) complete remission (in clinical, radiological, endoscopic and functional aspects); 3) incomplete (with the preservation of functional or structural disorders in the gastroduodenal zone). The condition of the mucous membrane of the stomach and duodenum: 1) chronic gastritis; 2) chronic duodenitis. Functional state of the gastroduodenal system Secretion: normal, increased, reduced. Motility: normal, accelerated, slow; evacuation: normal, accelerated, delayed, duodenostasis. Complications: bleeding, perforation, penetration, perigastritis, periduodenitis, cicatricial deformity of the stomach and duodenum. clinical picture. The clinical picture of peptic ulcer is polymorphic. Symptoms depend on the gender and age of the patient, time of year, location and size of the ulcer, personal and social characteristics of the patient, and his professional qualities. The clinic is determined by a combination of signs: the chronic course of the disease from the moment of its onset, the presence of signs of exacerbation and remission of the disease, healing of the defect in the gastric and duodenal mucosa with the formation of a scar. Peptic ulcer is represented by two clinical and morphological variants: gastric ulcer and duodenal ulcer. Traditionally, pain and dyspeptic syndromes are distinguished. The leading clinical sign is pain in the upper abdomen. By the nature of the pain syndrome, it is almost impossible to distinguish between chronic bacterial gastritis and peptic ulcer. Pain in the epigastric region, on an empty stomach, mainly in spring and autumn, is equally common in both peptic ulcer and chronic bacterial gastritis. Relief of pain syndrome with food and medicinal antacids is achieved both in chronic bacterial gastritis and peptic ulcer. Distinctive for duodenal ulcer is only the presence of pain in the epigastric region at night. Vomiting with peptic ulcer is rare. Nausea is much more common with stomach ulcers and duodenal ulcers. Constipation accompanies chronic duodenal ulcer. Symptoms of peptic ulcer disease are determined by the number of ulcerative defects and their localization. Multiple stomach ulcers are 3 times more common in men. The clinical picture in this case depends on the localization of peptic defects. With ulcers in the body of the stomach, dull pain in the epigastrium without irradiation, which occurs 20-30 minutes after eating, and nausea are noted. With ulcers of the subcardial region, dull pains under the xiphoid process, radiating to the left half of the chest, are characteristic. Combined gastric ulcers and duodenal ulcers are a combination of an active gastric ulcer and a healed duodenal ulcer. They are characterized by long-term preservation of the pain syndrome, persistent course of the disease, frequent relapses of the disease, slow scarring of the ulcer and frequent complications. Extrabulbous ulcers include ulcers located in the region of the bulboduodenal sphincter and distal to it. Their clinical picture has its own characteristics and has much in common with duodenal ulcers. They occur mainly in patients aged 40-60 years. Postbulbar ulcers are severe and prone to frequent exacerbations, accompanied by massive bleeding. Pain localized in the right upper quadrant of the abdomen, radiating to the back or under the right shoulder blade, occurs in 100% of cases. The intensity, severity of pain, which subsides only after taking narcotic analgesics, brings patients to severe neurasthenia. Seasonality of exacerbations in extra-bulbous ulcers is recorded in almost 90% of patients. In many patients, gastrointestinal bleeding becomes a cardinal symptom. Ulcers of the pyloric canal are characterized by a symptom complex called the pyloric syndrome: epigastric pain, nausea, vomiting, and significant weight loss. The exacerbation of the disease is very long. Against the background of intensive antiulcer therapy, the ulcer scars within 3 months. Abundant blood supply to the pyloric canal causes massive gastric bleeding. Diagnostics. In the uncomplicated course of a peptic ulcer, there are no changes in the general blood test; a slight decrease in ESR and slight erythrocytosis are possible. When complications arise in blood tests, anemia appears, leukocytosis - when the peritoneum is involved in the pathological process. There are no changes in the general analysis of urine. In the biochemical analysis of blood in cases of complicated course of peptic ulcer, changes in the parameters of the sialic test, C-reactive protein, DPA reaction are possible. The traditional method of research in the pathology of the stomach is the determination of the acidity of gastric contents. Various indicators are possible: elevated and normal, in some cases even reduced. A duodenal ulcer occurs with high acidity of gastric juice. In X-ray examination, a peptic ulcer is a "niche" - a depot of barium suspension. In addition to such a direct radiographic symptom, indirect signs of a peptic defect are important in the diagnosis: hypersecretion of the contents of the stomach on an empty stomach, evacuation disorders, duodenal reflux, cardia dysfunction, local spasms, convergence of mucosal folds, cicatricial deformity of the stomach and duodenum. Gastroduodenoscopy with biopsy is the most reliable method for diagnosing peptic ulcer. It allows you to assess the nature of changes in the mucous membrane in the edge of the ulcer, in the periulcerous zone and guarantees the accuracy of the diagnosis at the morphological level. In endoscopic and morphological studies, it was found that most stomach ulcers are located in the area of the lesser curvature and antrum, much less often - on the greater curvature and in the area of the pyloric canal. 90% of duodenal ulcers are located in the bulbar region. A peptic ulcer is typically round or oval in shape. Its bottom consists of necrotic masses, under which there is granulation tissue. The presence of dark blotches on the bottom indicates bleeding. The ulcer healing phase is characterized by a decrease in hyperemia of the mucous membrane and an inflammatory shaft in the periulcerous zone. The defect becomes less deep, gradually cleared of fibrinous plaque. The scar looks like a hyperemic area of the mucous membrane with linear or stellate retractions of the wall. In the future, during endoscopic examination at the site of the former ulcer, various violations of the relief of the mucous membrane are determined: deformations, scars, narrowing. At endoscopy, a mature scar due to the replacement of a defect with granulation tissue has a whitish appearance, there are no signs of active inflammation. A morphological study of a biopsy specimen obtained from the bottom and edges of the ulcer reveals cellular detritus in the form of an accumulation of mucus with an admixture of decaying leukocytes, erythrocytes and desquamated epithelial cells with collagen fibers located underneath. Differential diagnostics. With the widespread use of endoscopy, the differential diagnosis of ulcerations of the stomach and duodenum (symptomatic ulcers, specific ulcerations in tuberculosis, syphilis, Crohn's disease, primary ulcerative cancer, secondary malignant ulcers) becomes especially important. For symptomatic ulcers, there must be a cause that caused them (extreme exposure, clinical and morphological signs of endocrine diseases, cardiovascular and respiratory disorders, rheumatic diseases). More than for peptic ulcer, they are characterized by a multiplicity of lesions, predominant localization in the stomach, and significant size. With peptic ulcer, pain syndrome prevails, and with chronic gastritis - dyspeptic phenomena. In chronic gastritis, pain is mild or absent, there is no seasonality of the disease and limited pain on palpation; the aggravation of the disease often depends on the nature of the food. The state of the secretory function of the stomach with gastritis can be different. Of decisive importance are gastroscopy and gastrobiopsy, in which mucosal changes characteristic of gastritis and an ulcer in peptic ulcer are detected. Hiatus hernia (HH) is also often accompanied by pain in the epigastrium. However, unlike peptic ulcer disease, this disease is characterized mainly by the elderly age of patients, the relationship of pain with the position of the body (pain increases in the supine position, weakens in the upright position). The diagnosis of HH is confirmed by the results of X-ray examination. Chronic cholecystitis is characterized by pain in the right hypochondrium and epigastrium, often radiating to the right shoulder blade, to the shoulder, to the angle of the lower jaw on the right. With acalculous cholecystitis, they have a dull, monotonous, pressing character, and with calculous cholecystitis, they acquire the character of colic. Nausea, constipation, flatulence are noted. Persistent subfebrile condition is possible. With prolonged obstruction of the bile ducts, jaundice may join. The diagnosis of damage to the biliary system is verified by the data of abdominal ultrasound, X-ray examination (cholecystography), endoscopic retrograde cholepancreatography (ERCP), as well as the results of duodenal sounding, which is indicated only for a stoneless process. In acute pancreatitis and exacerbation of chronic pain, they are localized in the left half of the epigastric region, are shingles in nature, provoked by the intake of any food. In the anamnesis - pathology of the biliary system, alcohol abuse, long-term use of pancreatic drugs. Objectively reveal weight loss, polyfecal, steatorrhea, creatorrhea. The diagnosis is confirmed by the results of a biochemical blood test for pancreatic enzymes, feces - for digestibility, as well as instrumental data. Treatment. Rational therapy for peptic ulcers should include a regimen, appropriate nutrition, drug treatment, psychotherapy, physical and spa treatment methods. During the period of exacerbation of peptic ulcer disease, it is necessary to strictly observe a fractional diet (from 4 to 6 times a day with a small volume of each portion of food taken at certain hours). Food products must have good buffering properties and contain sufficient protein (120–140 g). Psychotherapy is essential for stopping or reducing psychoneurotic reactions arising from persistent pain syndrome and its expectation. Medicines used to treat peptic ulcers are divided into 5 groups: 1) drugs that affect the acid-peptic factor (antacids and H2histamine blockers, other antisecretory agents); 2) drugs that improve the gastric mucosal barrier; 3) drugs that increase the synthesis of endogenous prostaglandins; 4) antibacterial and antiseptic agents; 5) drugs that normalize motor-evacuation disorders of the stomach and duodenum. Antacids: 1) soluble (absorbable) - bicarbonate of soda, calcium carbonate (chalk) and magnesium oxide (burnt magnesia); 2) insoluble (non-absorbable): magnesium trisilicate and aluminum hydroxide. Soluble antacids have a fast, energetic, but short-term alkalizing effect, but often cause side effects, which is why they are not used in the treatment of peptic ulcers. Insoluble antacids based on aluminum hydroxide and magnesium hydroxide (Almagel, Phosphalugel, Gelusillac, Topaal, Maalox, etc.) provide long-term neutralization of hydrochloric acid, envelop the mucous membrane, protecting it from the damaging effects of acid and food. In addition to neutralizing hydrochloric acid, they help reduce the proteolytic activity of gastric juice, bind lysolecithin and bile acids, and have a universal cytoprotective effect. Antacids should be taken 1-2 hours after meals and at night. Maalox is prescribed in suspension (15 ml 4 times a day) or tablets (1-2 tablets 4 times a day), phosphalugel - in the form of a gel (16 g 3-4 times a day). One of the main side effects of nonabsorbable antacids is stool disturbance. Aluminum hydroxide preparations cause constipation, and magnesium hydroxide preparations (Maalox) have a dose-dependent laxative effect. A new era in the treatment of peptic ulcer began with the advent of H2- histamine blockers. Under physiological conditions, histamine mediates extragastric nerve and humoral stimuli that cause acid production. Stimulation of the production of hydrochloric acid by histamine is due to an increase in the activity of cAMP, which acts on the enzyme adenylcyclase contained in the acid-producing region of the stomach, which enhances the secretion of hydrogen ions. The data obtained were the basis for the synthesis of drugs that interrupt the participation of histamine in the secretory process at the cellular level, such as cimetidine, ranitidine, famotidine, nizatidine, etc. In addition, H antagonists2Histamine receptors prevent microcirculation disorders in the gastric mucosa and thus prevent the development of ulcers. In addition, they reduce the production of pepsin, increase the secretion of bicarbonates, normalize gastroduodenal motility, increase the number of DNA-synthesizing epithelial cells, stimulating reparative processes and accelerating the healing of chronic gastric and duodenal ulcers. However, 1st generation drugs (cimetidine, cinamet, belomet, tagamet) can cause changes in the nervous system, toxic hepatitis, rhythm and conduction disturbances in the cardiovascular system, and changes in the hematopoietic organs. H blockers2subsequent generations of histamine receptors - ranitidine (zantak, ranisan, gistak), famotidine (kvamatel, lecedil, gastrosidin), nizatidine (roxatidine) differ from cimetidine in good tolerance. Ranitidine is prescribed at a dose of 150 mg 2 times a day, famotidine - 20 mg 2 times a day for 4-6 weeks. To prevent withdrawal syndrome after ulcer healing, it is recommended to continue taking ranitidine (150 mg) or famotidine (20 mg) at night for 2-3 months. In recent years, a new antisecretory drug omeprazole (omenrol, omez, losek), which belongs to benzimidazole derivatives, has appeared. It blocks the enzyme H + -K + -ATPase of the proton pump of the parietal cell. The short half-life (about 1 hour) and long duration of action (18-24 hours) make it possible to take this drug once. Omeprazole is prescribed 20 mg at night 1 time per day for 2-3 weeks. Omeprazole ranks first in terms of the severity of the antisecretory effect among modern antiulcer drugs. Side effects of the drug are not very pronounced. Widespread use in the treatment of peptic ulcers has found gastrocepin (nirenzepine, gastrozepine), which belongs to anticholinergic drugs. The drug selectively blocks muscarinic acetylcholine receptors located in the cells of the gastric mucosa that produce hydrochloric acid and pepsin. Gastrocepin has an inhibitory effect on basal and stimulated gastric secretion, inhibits the production of pepsin, slows down evacuation from the stomach, causes inhibition of gastrin production, reduces the level of pancreatic polypeptide, has a cytoprotective effect by increasing the production of gastric mucus glycoproteins, as well as by improving the blood supply to the mucous membrane of the gastroduodenal region . Assign it to 50 mg 2 times a day 30 minutes before meals. The course of treatment is an average of 4 weeks. Medicines that strengthen the mucous barrier of the stomach include preparations of colloidal bismuth (denol), which forms a protective film on the mucous membrane, reduces the peptic activity of the stomach, forming an insoluble compound with pepsin, enhances mucus formation, has a cytoprotective effect, increasing the content of prostaglandins in the stomach wall. Denol has the ability to inhibit the activity of HP in the gastric mucosa. The drug is prescribed 2 tablets (240 mg) 2 times a day half an hour before meals or 2 hours after meals. To avoid the accumulation of bismuth salts in the body, it is not recommended to carry out therapy with these drugs for more than 8 weeks. For the purpose of antibacterial therapy for gastric and duodenal ulcers, tetracycline, amoxicillin, and clarithromycin are used. They are used in combination with other antiulcer drugs. Several schemes of combination therapy (two-, three-, four-component) have been proposed. Two-component therapy: amoxicillin 1000 mg 2 times a day for 2 weeks; omeprazole 40 mg twice a day. The three-component scheme includes the preparation of colloidal bismuth 2 mg 120 times a day; tetracycline 4 mg 250 times a day; metronidazole 4 mg 250 times a day. The therapy cycle is 4 days. The four-component scheme involves omeprazole 20 mg 2 times a day from the 1st to the 10th day; de-nol 120 mg 4 times a day from the 4th to the 10th day; tetracycline 500 mg 4 times a day from the 4th to the 10th day; metronidazole 500 mg 3 times a day from the 4th to the 10th day. The four-component scheme for the treatment of peptic ulcer of the stomach and duodenum is recognized as the most effective. 6 weeks after it, the healing of the peptic defect is observed in 93-96% of patients. After scarring of a peptic ulcer of the stomach and duodenum, two types of treatment are traditionally used. 1) Continuous maintenance therapy is carried out with antisecretory drugs at half the daily dose for a period of up to one year. 2) Therapy "on demand", involves the use of one of the antisecretory agents in half the daily dose for two weeks when symptoms of peptic ulcer appear. Prognosis and prevention. Uncomplicated forms of the disease have a favorable prognosis for life and work. In case of complications of peptic ulcer disease, the prognosis is determined by the timeliness of surgical care. Prevention of peptic ulcer recurrence includes dynamic monitoring with mandatory follow-up examinations by a doctor 2 times a year. Examinations should include clinical and endoscopic, and, if necessary, morphological examination. As a preventive measure, it is recommended to normalize sleep and rest, give up bad habits, limit the intake of ulcerogenic medications, rational five meals a day and use two- or three-component therapy for a week every 3 months. LECTURE No. 12. Diseases of the digestive tract. Diseases of the intestines. Diseases of the small intestine. Chronic enteritis Chronic enteritis is a disease of the small intestine, characterized by a violation of its functions (digestion and absorption) against the background of dystrophic and dysregenerative changes, culminating in the development of inflammation, atrophy and sclerosis of the mucous membrane of the small intestine. Etiology and pathogenesis. This is a polyetiological disease that can be the result of acute inflammation of the small intestine or a primary chronic process. In recent years, Yersinia, Helicobacteria, Proteus, Pseudomonas aeruginosa, rotaviruses, numerous representatives of protozoa and helminths (giardia, ascaris, tapeworms, opisthorchia, cryptosporidium) have been given great importance as an etiological factor in chronic enteritis. Of great importance in the occurrence of chronic enteritis are alimentary factors - overeating, eating dry food, unbalanced, predominantly carbohydrate foods, abuse of spices. Enteritis is caused by ionizing radiation, exposure to toxic substances, and drugs. Among the common pathogenetic mechanisms of chronic diseases of the small intestine, there are changes in the intestinal microflora against the background of a decrease in local and general immunity. Changes in the immune status - a decrease in the content of secretory IgA, an increase in the level of IgE, a decrease in blast transformation of lymphocytes and inhibition of leukocyte migration - lead to colonization of the small intestine by representatives of opportunistic microflora and a decrease in normal anaerobic flora. Bacterial colonization of the small intestine enhances intestinal secretion due to the activation of epithelial cell cAMP, which increases intestinal permeability, enhances the production of electrolytes and water by cells. The secretion of water and electrolytes leads to a violation of water-salt metabolism. Under the influence of microbial flora, the enterohepatic circulation of bile is disturbed. Fatty acids bind calcium ions, forming sparingly soluble soaps that are excreted in the faeces. Violation of calcium metabolism is promoted by changes in the metabolism of vitamin D, which reduces the absorption of calcium. Under the influence of metabolic disorders of fat-soluble vitamins, the content of microelements in the blood decreases. Prolonged dysbiosis promotes sensitization to microbial and food antigens, causes immune inflammation of the mucous membrane, which results in the formation of tissue antigens. The increased permeability of the mucous barrier is accompanied by the resorption of unsplit protein macromolecules, which become allergens, and immunological reactivity is impaired. With allergies, biologically active substances are released that increase the permeability of the intestinal wall, change the functional properties of enterocytes. Violations of the microstructure of the enterocyte cytoplasmic membrane lead to inhibition of lactase activity first, and then maltase and sucrase activity. With dystrophic, dysregenerative changes in epitheliocytes, the synthesis of enzymes and their sorption on the membranes of epitheliocytes - disaccharidases, peptidases, enterokinase, alkaline phosphatase - are reduced, which causes disturbances in both membrane and cavity digestion. All this becomes the basis of the malabsorption syndrome. In the early stages of the disease, lipid metabolism disorders develop due to a decrease in fat absorption, its loss with feces, and changes in the intestinal phase of enterohepatic bile circulation. Violation of bile metabolism, in turn, leads to a violation of lipid metabolism, which affects the structure and function of cell membranes. In connection with insufficient absorption of fat, a violation of the synthesis of steroids occurs, which induces a violation of the functions of the endocrine glands. Morphologically, chronic enteritis is manifested by inflammatory and dysregenerative changes in the mucous membrane of the small intestine. If the process progresses, its atrophy and sclerosis are observed. Classification (Zlatkina A. R., Frolkis A. V., 1985). 1) Etiology: intestinal infections, helminthic invasions, alimentary, physical and chemical factors, diseases of the stomach, pancreas, biliary tract. 2) Phases of the disease: exacerbation; remission. 3) Degree of severity: mild; moderate; heavy. 4) Current: monotonous; recurrent; continuously recurring; latent. 5) Character of morphological changes: eunit without atrophy; jeunitis with moderate partial villous atrophy; jeunitis with partial villous atrophy; eunit with total villous atrophy. 6) The nature of functional disorders: disorders of membrane digestion (disaccharidase deficiency), malabsorption of water, electrolytes, trace elements, vitamins, proteins, fats, carbohydrates. 7) Complications: solaritis, nonspecific mesadenitis. clinical picture. The clinical picture of chronic enteritis consists of local and general enteric syndromes. The first is caused by a violation of the processes of parietal (membrane) and cavity digestion (maldigestion). Patients complain of flatulence, pain in the paraumbilical area, cap-shaped bloating, loud rumbling, diarrhea, and, less commonly, constipation. Palpation reveals pain in the mesogastrium, as well as to the left and above the navel (positive Porges sign), splashing noise in the area of the cecum (Obraztsov sign). The feces take on a clayey appearance, and polyfecal matter is characteristic. General enteral syndrome is associated with impaired absorption of food ingredients (malabsorption), resulting in disorders of all types of metabolism, changes in homeostasis. Characterized by multifaceted metabolic disorders, primarily protein, which is manifested by a progressive loss of body weight. Changes in carbohydrate metabolism are less pronounced, which is manifested by bloating, rumbling in the abdomen and increased diarrhea while taking dairy products. To a large extent, the deficiency of body weight in patients is due not only to protein, but also to lipid imbalance. Changes in lipid metabolism are closely related to metabolic disorders of fat-soluble vitamins and minerals (calcium, magnesium, phosphorus). The characteristic signs of calcium deficiency are a positive symptom of the muscle roller, convulsions, recurrent "unmotivated" bone fractures, osteoporosis, osteomalacia. There are also swelling of the face, cyanosis of the lips, glossitis, irritability, poor sleep. Violations of the water and electrolyte balance are manifested by general weakness, physical inactivity, muscle hypotension, nausea, vomiting, and changes in the central nervous system. Symptoms of polyhypovitaminosis become typical for chronic enteritis of moderate and severe severity. Hypovitaminosis C is clinically manifested by bleeding gums, repeated nasal, uterine bleeding, bruising on the skin. Hypovitaminosis B is accompanied by pallor of the skin, glossitis, angular stomatitis (cheilez). Signs of deficiency of fat-soluble vitamins (A, O, E, K): poor twilight vision, dry skin and mucous membranes, increased bleeding of the gums. Severe forms of chronic enteritis occur with symptoms of endocrine dysfunction (pluriglandular insufficiency). Hypocorticism is manifested by arterial hypotension, cardiac arrhythmias, anorexia, and skin pigmentation. A decrease in the activity of the gonads is accompanied by ovarian dysfunction, menstrual disorders, in men - impotence, gynecomastia, hair loss. Thyroid dysfunction is characterized by general weakness, dry skin, bradycardia, decreased performance, and intellectual-mnestic disorders. Diagnosis and differential diagnosis. A general blood test reveals micro- and macrocytic anemia, an increase in ESR, and in severe cases - lympho- and eosinopenia. If the disease is of parasitic origin, lymphocytosis and eosinophilia may be observed in the blood. A scatological examination reveals an intestinal type of steatorrhea due to fatty acids and soaps, creatorrhea, amylorrhea. The content of enterokinase and alkaline phosphatase in feces increases. The daily mass of feces increases significantly. Bacteriological analysis of feces reveals dysbacteriosis of varying degrees. There is a decrease in lacto- and bifidobacteria, enterococci, strains of Escherichia coli with altered enzymatic properties appear. In the general analysis of urine in severe form of chronic enteritis, microalbuminuria and migrohematuria are noted. In a biochemical blood test, hypoproteinemia, hypoalbuminemia, hypoglobulinemia, hypocalcemia, a decrease in the level of magnesium, phosphorus, and other microelements, electrolyte metabolism disorders in the form of a decrease in the level of sodium and potassium are detected. Lipid metabolism disorders are accompanied by changes in the lipid spectrum: the level of cholesterol, phospholipids decreases, and the spectrum of bile acids, phospholipids and triglycerides also changes. The results of an x-ray study allow us to clarify the motor function of the small intestine and the relief of the mucosa, dystonic and dyskinetic changes in the form of a slowdown or acceleration of the passage of a suspension of barium sulfate through the small intestine, and the relief of the mucosa changes in the form of uneven thickening, deformation and smoothing of the folds. Gastroduodenoscopy reveals atrophic gastritis and duodenitis. The morphological picture of a mild form of chronic enteritis is characterized by thickening of the villi, their deformation, a decrease in the depth of the notches, a decrease in the tone of smooth muscles, subepithelial edema, degenerative changes in the surface of the epithelium, thinning of the brush border of cells, a decrease in the number of goblet cells in the region of the villi, an increase in the number of crypts, infiltration of the own layer mucosa with lymphoplasmacytic elements, a decrease in Paneth cells in the area of the bottom of the crypts. For the moderate form, partial atrophy of the villi, a decrease in the number of crypts, thinning of the mucous membrane, a decrease in the brush border, and lymphoplasmacytic infiltration of the submucosal and muscular layers are typical. The severe form of the disease is characterized by progressive villous atrophy, diagnosed by histological, histochemical, and morphometric criteria. The process of proliferation of enterocytes prevails over their differentiation, an abundance of immature, defective cells appears. Differential diagnosis in chronic enteritis is carried out with celiac enteropathy, Crohn's disease, Whipple's disease, intestinal amyloidosis, diverticular disease, lymphoma, tumors of the small intestine. Common to all these conditions are clinical syndromes of indigestion, absorption and dysbacteriosis. The final diagnosis is confirmed by morphological examination of the mucous membrane of the small intestine. So, for celiac enteropathy, an anamnestic indication of the relationship of exacerbations of the disease with the use of gliadin-containing products is typical. The clinic of celiac enteropathy resembles chronic enteritis. Most often, the upper intestines are affected and there are no changes in the ileum. The optimal site for taking biopsy specimens is the area of the mucous membrane near the ligament of Treitz. Morphological examination reveals a decrease in the number of goblet cells and an increase in the number of interepithelial lymphocytes, subtotal villous atrophy, and inflammatory cell infiltration of its own layer. With celiac enteropathy, morphological changes on the background of a gluten-free diet are reversible, in contrast to banal chronic enteritis, in which morphological changes are irreversible. In Crohn's disease, clinical polymorphism is noted, due to the autoimmune genesis of the disease and its characteristic systemic manifestations (such as autoimmune thyroiditis, polyarthritis, iritis, hepatitis, frequent combination of enteritis and distal colitis). Endoscopic and morphological tests have a high resolution in the verification of Crohn's disease, revealing the mosaic nature of the intestinal lesion, typical changes of the "cobblestone pavement" type, which alternate with areas of intact mucosa. X-ray, endoscopic examination can detect intestinal strictures, sometimes intestinal fistulas are formed. Morphological diagnostics states inflammatory cell infiltration of all layers of the intestinal wall with maximum damage to the submucosal layer and minimal changes in the mucosa. In the submucosal layer, lymphocytic sarcoid-like granulomas, pathognomonic for this disease, are found. For Whipple's disease, in addition to signs of enteritis, extraintestinal manifestations in the form of fever, arthritis, lymphadenopathy, arterial hypotension, and skin pigmentation are characteristic. The most informative morphological criteria of the disease. Biopsy specimens taken from the small intestine reveal intracellular and extracellular fat accumulation in the small intestinal mucosa and mesenteric lymph nodes; infiltration of its own layer by large microphages containing CHIC-positive fat-free granules, and the presence of bacilli in the mucosa. Treatment. Treatment of chronic enteritis should be comprehensive, including agents that affect etiological factors, pathogenetic mechanisms, as well as local and general symptoms of the disease. The basis is dietary nutrition, which helps to reduce the increased osmotic pressure in the intestinal cavity, reduces secretion, and normalizes the passage of intestinal contents. Exclude products containing coarse vegetable fiber (raw vegetables, fruits, rye bread, nuts, pastry, canned food, spices, spicy dishes, whole milk, beer, kvass, carbonated and alcoholic drinks). The use of table salt is limited. Fractional meals are needed, up to 5-6 times a day. During the period of remission, some vegetables and fruits are introduced into the diet, up to 100-200 g per day. Assign lettuce, ripe peeled tomatoes, soft pears, sweet apples, oranges, tangerines, raspberries, strawberries, wild strawberries. Food should be boiled or steamed. Drug therapy should be etiotropic, pathogenetic and symptomatic. Etiotropic treatment: for grade II-IV dysbiosis, antibacterial drugs are prescribed: metronidazole (0,5 g 3 times a day), clindamycin (0,5 g 4 times a day), cephalexin (0,5 g 2 times a day). day), biseptol (0,48 g 2 times a day), sulgin (1 g 3-4 times a day), furazolidone (0,1 g 4 times a day). After using antibacterial drugs, eubiotics are prescribed - bifidumbacterin or bificol 5 doses 3 times a day 30 minutes before meals, coli-bacterin or lactobacterin 3 doses 3 times a day before meals, hilakforte 40 drops 3 times a day before meals. Treatment with bacterial preparations is carried out for a long time: 3 courses of 3 months each year. For staphylococcal dysbacteriosis, an antistaphylococcal bacteriophage is prescribed (20 ml 3 times a day for 15-20 days), for proteus dysbacteriosis - coliprotean bacteriophage orally, 20 ml 3 times a day, the course of treatment is 2-3 weeks. As an antidiarrheal symptomatic agent, imodium (loperamide) is prescribed 1 capsule 2-3 times a day before meals for 3-5 days. To improve the digestion process, enzymes are recommended: pancreatin, panzinorm forte, festal, digestal, pankurmen, mezim forte, trienzyme, the doses of which are selected individually (from 1 tablet 3 times a day to 3-4 tablets 4 times a day) and which are prescribed directly before or during meals for 2-3 months. If necessary, enzyme replacement therapy is continued for a longer time. To normalize the general condition of patients with enteritis and eliminate metabolic disorders, substitution therapy is indicated. In order to compensate for the deficiency of vitamins, vitamins B and B are prescribed for 4-5 weeks.6 50 mg each, PP - 10-30 mg, C - 500 mg each. For steatorrhea, parenteral administration of vitamin B is indicated.2 (100-200 mcg) in combination with fat-soluble vitamins. Riboflavin 0,02 g, folic acid 0,003 g once a day, vitamin E 3300 IU 2 times a day are prescribed inside. In chronic enteritis occurring with severe protein deficiency, along with a diet, parenteral administration of plasma, 150-200 ml of protein hydrolysates and mixtures of amino acids (aminopeptide, alvesin, polyamine, intrafusin, 250-500 ml intravenously for 20 days) in combination with anabolic hormones (retabolil 2,0 ml 1 time in 7-10 days for 3-4 weeks) and fatty mixtures such as intralipid. The appointment of steroids is indicated only with significant protein deficiency, hypoproteinemia, the presence of adrenal insufficiency. To correct water and electrolyte disorders, intravenous administration of panangin 20-30 ml, calcium gluconate 10% 10-20 ml in 200-400 ml of isotonic solution or glucose solution, polyionic solutions "Disol", "Trisol", "Quartasol" are indicated. Electrolyte solutions are administered intravenously for 10-20 days under the control of the acid-base state and the level of blood electrolytes. Prognosis and prevention. The prognosis for life and ability to work is favorable in most cases. Prognostically unfavorable signs are a continuously relapsing course of the disease, sudden significant weight loss, anemia, endocrine disorder syndrome (decreased libido, dysmenorrhea, infertility). Prevention of chronic enteritis consists in the timely treatment of acute intestinal infections and concomitant diseases of the gastroduodenal zone, in observing the diet, in the prophylactic administration of bacterial preparations during X-ray and radiotherapy. LECTURE No. 13. Diseases of the digestive tract. Diseases of the intestines. Crohn's disease Crohn's disease is a chronic bowel disease with systemic manifestations; the morphological basis of which is granulomatous autoimmune inflammation of the gastrointestinal tract. Etiology and pathogenesis. The etiology and pathogenesis of the disease have not been sufficiently studied. The most popular are the infectious and immune concepts of the occurrence of the disease. In recent years, reports have appeared on the etiological role of microorganisms of the genus Yersinia. However, it is difficult to determine whether these microbial agents are pathogens or commensals. At the same time, changes in the intestinal microflora play an important role in the pathogenesis of the disease. Typically, a decrease in bifidum-type bacteria with a simultaneous increase in enterobacteria with signs of pathogenicity. Autoimmune mechanisms play a role in the development of the disease. In Crohn's disease, autoantibodies (IgC, IgM) appear against intestinal tissues. The morphological substrate of the disease is an autoimmune inflammatory process that occurs initially in the submucosal layer, spreads to the entire thickness of the intestinal wall and is characterized by the presence of granulomatous infiltrates followed by ulceration of the mucous membrane, the development of abscesses and fistulas that heal with the formation of scars and narrowing of the intestinal lumen. With an increase in the duration of the disease, the extent of the lesion increases and symptoms of extraintestinal disorders appear. Classification. Classification (F.I. Komarov, A.I. Kazanov, 1992). 1) Course: acute; chronic. 2) Characteristics of the process: lesion within the small intestine; lesion within the ileocecal region; lesion within the colon. 3) Complications: narrowing of the intestine; toxic dilatation of the colon; fistulas; amyloidosis; nephrolithiasis, cholelithiasis; AT12-deficiency anemia. clinical picture. The clinical picture of Crohn's disease is characterized by significant diversity, which is determined by the localization and extent of the pathological process in the intestine, the form of the disease and the addition of complications. The onset of the disease can be acute, when the disease progresses from the very beginning, and chronic, when the disease begins gradually. In the first case, the diagnosis is often made during laparotomy performed for suspected appendicitis, or intestinal obstruction that developed for no apparent reason in young people. At the same time, a hyperemic area of the small intestine, enlarged lymph nodes of the mesenteric root, characteristic of Crohn's disease, are found. Patients complain of pain in the abdomen without a specific localization, loosening of the stool without visible pathological impurities, weight loss, low-grade body temperature. An objective study pays attention to the pallor of the skin, which correlates with the severity of anemia, swelling in the legs due to impaired absorption and protein metabolism. On palpation of the abdomen, flatulence and rumbling are noted. When the process is localized in the large intestine, alternating constipation with diarrhea, cramping abdominal pain, liquid or semi-formed stools containing an admixture of blood are noted. When the upper gastrointestinal tract is affected, symptoms resembling chronic esophagitis, chronic gastritis, and chronic duodenitis occur. There may be pain behind the sternum during the passage of food through the esophagus, night and "hungry" pain in the epigastrium, pain on palpation in the pyloroduodenal zone. During physical examination of the patient, pallor of the skin, subfebrile condition, body weight deficiency are determined, palpation reveals spasmodic bowel loops, pain in the paraumbilical zone, in the right iliac region. In Crohn's disease, extraintestinal signs of the disease are noted: aphthous stomatitis, phlegmon and fistulas of the oral cavity, arthritis, resembling rheumatoid arthritis in the clinic, with characteristic symptoms of symmetrical lesions of small joints, stiffness in the morning. Typical changes in the eyes: iritis, iridocyclitis, maculopathy. The skin may develop erythema nodosa and pyoderma gangrenosum. Diarrhea is characterized by an increase in the frequency of stools up to 10 times a day or more, polyfecal matter. The volume of the stool is determined by the anatomical localization of the process: with damage to the proximal small intestine, the volume of feces is much larger than with damage to the distal parts. Weight loss is noted in all patients. Diagnosis and differential diagnosis. A clinical blood test during an exacerbation reveals leukocytosis, anemia, and an increase in ESR. Changes in the general urine analysis appear in severe forms, characterized by the addition of renal amyloidosis (proteinuria). A biochemical blood test reveals hypoproteinemia, hypoalbuminemia, an increase in α-globulins, a decrease in the content of iron, vitamin B12, folic acid, zinc, magnesium and potassium. The data of scatological examination allow to indirectly assess the level of the lesion. In the coprogram with small intestinal localization of the process, polyfecal matter, steatorrhea, creatorrhoea are found; with the colon - an admixture of mucus, leukocytes, erythrocytes. X-ray diagnostics allows you to establish the localization and prevalence of the pathological process in the intestine. Areas of the affected intestine alternate with areas of the unchanged intestine. The altered loops become rigid, the picture is mosaic with small filling defects and with the penetration of contrast beyond the intestinal wall in the form of pockets. The intestine in the affected area acquires the character of finely fringed, with the formation of pseudodiverticula. The contractile capacity of the intestinal wall is reduced or completely lost, the evacuation of barium slows down. An uneven narrowing of the intestinal lumen is observed, as a result, it becomes so narrow that it takes on the form of a lace. Above the zone of narrowing, the intestine expands. Endoscopic diagnosis is of decisive importance in the verification of the diagnosis. For Crohn's disease, the most characteristic is the change in the antrum of the stomach and the initial section of the duodenum. Endoscopically, it is possible to detect a circular narrowing of the antrum, resembling tumor stenosis. The initial period of Crohn's disease is characterized by poor endoscopic data: a dull mucous membrane, against which erosions of the aphthae type are visible, surrounded by whitish granulations. The vascular pattern is absent or smoothed out. In the lumen of the intestine and on its walls, purulent mucus is determined. In clinical remission, the described changes may disappear completely. As the disease progresses, the mucosa becomes unevenly thickened, has a whitish color, and large superficial or deep fissure ulcers are noted. The intestinal lumen narrows, making it difficult to advance the colonoscope. Colonoscopy makes it possible to perform a targeted biopsy of the mucous membrane in any part of the colon and in the terminal ileum. In Crohn's disease, the pathological process begins in the submucosal layer, so the biopsy should be performed in such a way that a portion of the submucosal layer enters the biopsy material. In connection with the above, in 54% of cases the morphological substrate of the disease is not detected. It is necessary to differentiate Crohn's disease from nonspecific ulcerative colitis, gastrointestinal tuberculosis, ischemic colitis, Whipple's disease, diverticular disease, pseudomembranous colitis, lymphogranulomatosis, primary small intestinal amyloidosis, chronic enteritis. Common to all of these diseases are the syndrome of intestinal dyspepsia and some systemic lesions. However, ulcerative colitis is characterized by a change in the distal parts of the colon with the obligatory involvement of the rectum and sigmoid in the process. In nonspecific ulcerative colitis, there is no segmentation of the lesion; less often than in Crohn's disease, systemic manifestations are determined, and malabsorption syndrome is less pronounced. However, the most accurate diagnosis of Crohn's disease is confirmed by endoscopy with targeted biopsy. Gastrointestinal form of tuberculosis is distinguished from Crohn's disease by frequent localization in the ileum, endoscopic findings that allow the detection of ulcers with raised, exfoliated edges filled with grayish contents. Such ulcers heal with the formation of a short scar, which is not observed in Crohn's disease. In the elderly, there is a need to differentiate Crohn's disease and ischemic colitis. For the latter, attacks of intense pain in the abdomen after eating are typical, irrigoscopically detectable colitis changes in the splenic flexure, descending and sigmoid colon. The most important radiographic sign of ischemic colitis is the "thumbprint" symptom. Endoscopic and morphological examination reveals typical for ischemic colitis hemosiderin-containing cells and fibrosis in the biopsy material. The diagnosis of lymphogranulomatosis and primary intestinal amyloidosis is made on the basis of histological examination. In the first case, Berezovsky-Sternberg cells are found in the biopsy specimen from the mesenteric lymph node, in the second case, there are deposits of amyloid in the rectal mucosa. Treatment. A mechanically and chemically gentle diet with a high content of proteins, vitamins, microelements is prescribed, with the exclusion of milk if it is intolerant, and the limitation of coarse plant fiber. The use of liquid enteral hydrolysates is indicated. Salazopreparations and corticosteroids form the basis of pathogenetic drug therapy. The daily dose of drugs is 3-6 g. With the localization of the pathological process in the large intestine, the activity of sulfasalazine exceeds the activity of prednisolone. In the absence of the effect of the use of sulfasalazine, with lesions predominantly of the small intestine and pronounced signs of immune inflammation, as well as in the presence of systemic manifestations of the disease, the use of corticosteroids is indicated. The effect of their use is noted in the first 8 weeks from the start of treatment. Prednisolone is prescribed according to the following scheme: at the height of an exacerbation, 60 mg per day, then the dose is gradually reduced and, by the 6-10th week, is adjusted to a maintenance dose of 5-10 mg per day. Upon reaching clinical remission, the drug is gradually canceled. If remission is not achieved, treatment with prednisolone is continued on an outpatient basis until 52 weeks. In severe course of the disease, in case of complications in the form of torpid current rectovaginal, skin-enteric, enteroenteric fistulas, the appointment of 6-mercaptopurine orally at 0,05 g 2-3 times a day is indicated for 10-day courses with an interval of 3 days until clinical remission is achieved . Subsequently, they switch to taking maintenance doses of the drug during the year. The dose of 6-mercaptopurine in this case is 75 mg per day. The effect of treatment with immunosuppressants can be determined no earlier than after 3-4 months. Widespread use in the treatment of Crohn's disease was found by metronidazole, the main indications for which are perianal fistulas and fissures, the lack of effect of salazopreparations and glucocorticoids, as well as relapses of the disease after proctectomy. The drug is prescribed at a dose of 500-1000 mg per day. The duration of the continuous course should not exceed 4 weeks. Symptomatic therapy of Crohn's disease is reduced to the appointment of short courses (2-3 days each) of antidiarrheal drugs (imodium, loperamide). Doses are selected individually according to the clinical effect. Do not prescribe antidiarrheals for a long time (more than 5 days). Due to the presence of malabsorption syndrome in Crohn's disease, enzyme preparations that do not contain bile acids (pancreatin, mesimforte, solizim, somilase) are used in a dose of 2 to 6 tablets with each meal. According to the indications, anemia and hypoalbuminemia are corrected by prescribing iron preparations (parenterally) and administering Alvezin, protein hydrolysers, aminopeptide, aminoblood. Assign multivitamins in pills, Essentiale in capsules. Treatment of dysbacteriosis is carried out according to general rules. Prognosis and prevention. With Crohn's disease, the prognosis for life with timely diagnosis and effective follow-up is favorable, but for work it is uncertain. In patients with severe disease, in the presence of complications and systemic manifestations, disability group I or II is established. Crohn's disease is a precancerous disease. The patient needs to be familiarized in detail with the features of the course of the disease and warned about possible complications, describing their clinical manifestations in an accessible form. LECTURE No. 14. Diseases of the digestive tract. Diseases of the colon. Nonspecific ulcerative colitis Nonspecific ulcerative colitis is an inflammatory disease that affects the mucous membrane of the colon with ulcerative-destructive changes, which has a chronic relapsing course, often accompanied by the development of life-threatening complications. Etiology and pathogenesis. Nonspecific ulcerative colitis is an idiopathic disease. The reasons for its occurrence are not known. Of the many theories explaining the origin of the disease (infectious, enzymatic, allergic, immune, neurogenic, etc.), the infectious theory is of greatest interest, but attempts to isolate the pathogen from the contents of the colon were unsuccessful. The pathological process in chronic ulcerative colitis begins in the rectum and spreads in the proximal direction, capturing the overlying parts of the colon. Inflammation can be limited to the rectum (proctitis), rectum and sigmoid (proctosigmoiditis), spread to the entire left section (left-sided colitis), or affect the entire colon (total colitis). In functional terms, the length of the colon in nonspecific colitis is reduced by about 1/3. In the study of pathological material revealed diffuse inflammation of the mucous membrane of the colon (pronounced swelling and plethora, thickening of the folds). Ulcers of various sizes are formed in the mucosa, having an irregular shape, the bottom of which is located in the mucous membrane, less often in the submucosal layer, in the muscular and serous membranes. Morphologically, in the initial period, an infiltrate in the lamina propria of the mucous membrane is determined, consisting of lymphocytes with an admixture of polymorphonuclear leukocytes, dilation of blood vessels and swelling of the endothelium of these vessels. Violation of microcirculation is accompanied by the development of hypoxia, which exacerbates the violations of the structure and function of the mucosal epithelium. The stage of pronounced clinical manifestations is accompanied by leukocyte infiltration of the surface layer of the epithelium, the development of cryptitis, in which accumulations of neutrophils occur in the lumen of the crypts. The distal parts of the crypts are obliterated, crypt abscesses appear, in the formation of which an important role is played by impaired maturation of epitheliocytes. With necrosis of the epithelium lining the crypts, crypt abscesses open, ulcers form. During the period of remission, the mucous membrane is restored, but its atrophy, deformation of the crypts, and uneven thickening of the lamina propria remain. Classification (Yu. V. Baltaitis et al., 1986). Clinical characteristic. 1. Clinical form: 1) acute; 2) chronic. 2. Current: 1) rapidly progressing; 2) continuously relapsing; 3) recurrent; 4) latent. 3. Degree of activity: 1) exacerbation; 2) fading exacerbation; 3) remission. 4. Severity: 1) light; 2) moderate; 3) heavy. Anatomical characteristic. 1. Macroscopic characteristic: 1) proctitis: 2) proctosigmoiditis; 3) subtotal lesion; 4) total defeat. 2. Microscopic characteristic: 1) the predominance of destructive-inflammatory processes; 2) reduction of inflammatory processes with elements of reparation; 3) consequences of the inflammatory process. Complications. 1. Local: 1) intestinal bleeding; 2) perforation of the colon; 3) narrowing of the colon; 4) pseudopolyposis; 5) secondary intestinal infection; 6) disappearance of the mucous membrane; 7) toxic dilatation of the colon; 8) malignancy. 2. General: 1) functional hypocorticism; 2) sepsis; 3) systemic manifestations - arthritis, sacroiliitis, skin lesions, iritis, amyloidosis, phlebitis, sclerosing cholangitis, liver dystrophy. clinical picture. The clinical picture of ulcerative colitis is polymorphic and depends on the severity of the course and severity of the process. The course of the inflammatory process, often considered chronic, in some cases becomes acute. The extent of damage to the colon may also vary. Nonspecific ulcerative colitis is characterized by 3 leading symptoms: discharge of scarlet blood during bowel movements, intestinal dysfunction and abdominal pain. Isolation of blood (from streaks on the surface of feces to 300 ml or more) during defecation is the first sign of the disease. In the acute form of the disease, blood is secreted by a jet, which leads to a decrease in blood pressure up to the development of collapse and hemorrhagic shock. Intestinal dysfunction manifests itself in the form of complaints of repeated unstable stools, which is the result of extensive damage to the mucous membrane and a decrease in the absorption of water and salts. Most often, diarrhea occurs with severe ulcerative colitis. However, diarrhea is not a reliable indicator of the severity of the process. The severity of diarrhea in combination with the presence of red blood in the stool matters. In a significant number of patients with ulcerative colitis, blood and mucus are periodically found on the surface of the formed feces, which is often mistakenly regarded as a manifestation of hemorrhoids. Patients complain of pain in the lower abdomen of a cramping or persistent nature, which is more often localized in the hypogastrium or the left iliac region, increases before the act of defecation and disappears after it. Tenesmus is often noted. When the submucosal, muscular and serous layers of the intestine are involved in the process, pain increases; palpation of the abdomen appears defense of the muscles of the anterior abdominal wall. The mild course of nonspecific ulcerative colitis is characterized by a satisfactory condition of patients. Pain in the abdomen is moderate and short-term. The chair is decorated, speeded up, up to 2-3 times a day. Blood and mucus are found in the stool. The process is localized within the rectum and sigmoid colon. The clinical course is recurrent. The effect of treatment with salazopreparations is satisfactory. Relapses occur no more than 2 times a year. Remissions can be long (more than 2-3 years). The moderate course of the disease is diagnosed if the patient has diarrhea. The chair is frequent (up to 6-8 times a day), in each portion an admixture of blood and mucus is visible. Cramping pains in the abdomen are more intense. There are intermittent fever with a rise in body temperature up to 38 ° C, intense general weakness. There may also be extraintestinal manifestations of the disease (arthritis, uveitis, erythema nodosum). The course is continuously recurrent, the effect of salazopreparations is unstable, hormones are prescribed during exacerbations. The severe form of the disease is characterized by an acute onset. A total lesion of the large intestine rapidly develops with the spread of the pathological process deep into the intestinal wall. The patient's condition deteriorates sharply. The clinic is characterized by a sudden onset, high fever, profuse diarrhea up to 24 times a day, profuse intestinal bleeding, and a rapid increase in dehydration. Tachycardia appears, blood pressure decreases, extraintestinal manifestations of nonspecific ulcerative colitis increase. Conservative treatment is not always effective, and emergency surgery is often required. Diagnosis and differential diagnosis. In clinical blood tests in mild forms of the disease, slight neutrophilic leukocytosis, an increase in ESR, and red blood counts are not changed. As the severity of the course increases and the duration of exacerbation increases, anemia of mixed origin occurs (B12-deficient and iron-deficient), increased ESR. In the biochemical analysis of blood in moderate and severe forms, dysproteinemia, hypoalbuminemia, hypergammaglobulinemia, electrolyte imbalance, and acid-base state are noted. In the general analysis of urine, changes appear only when complications arise in the form of nephrotic syndrome against the background of amyloidosis, when characteristic changes in urine tests are noted - proteinuria, "dead" urinary sediment, there is also an increase in the blood and the level of creatinine, urea. The main role in the diagnosis is acquired by endoscopic examination with targeted biopsy, since in nonspecific ulcerative colitis, the colon mucosa is primarily affected. The rectum is always involved in the pathological process, i.e., erosive and ulcerative changes are detected during endoscopy immediately behind the anal sphincter during sigmoidoscopy. In ulcerative colitis, the rectosigmoid bend is not always possible to overcome due to severe spasm. An attempt to hold the tube of the proctoscope is accompanied by severe pain. In this situation, the proctoscope should be inserted to a depth of no more than 12-15 cm. Colonoscopy during a severe exacerbation of nonspecific ulcerative colitis is not safe to carry out. It should be used at high risk of malignancy. It should be noted the high information content of sigmoidoscopy. The endoscopic picture depends on the form of the disease. With a mild form, edematous dull mucous membrane, thick whitish overlays of mucus on the walls of the intestine, and slight contact bleeding are visible. The vascular pattern of the submucosal layer is not visually determined. In the moderate course of the disease, hyperemia and edema of the mucous membrane, severe contact bleeding, hemorrhages, erosions and irregularly shaped ulcers, thick overlays of mucus on the walls of the intestine are revealed. In a severe course of the disease, the mucous membrane of the colon is destroyed over a considerable extent. A granular, bleeding inner surface, extensive areas of ulceration with fibrinous deposits, pseudopolyps of various sizes and shapes, pus and blood in the intestinal lumen are found. Contraindications for colonoscopy and sigmoidoscopy are severe forms of ulcerative colitis in the acute stage of the disease. X-ray examination allows you to determine the extent of the lesion; clarify the diagnosis in case of insufficiently convincing endoscopy data; differential diagnosis with Crohn's disease, diverticular disease, ischemic colitis; timely detect signs of malignancy. Plain radiographs can reveal shortening of the intestine, lack of haustration, toxic dilatation, free gas under the dome of the diaphragm during perforation. Irrigoscopy should be carried out with great care. It can provoke a deterioration in the patient's condition. In some cases, the preparation of the patient for barium enema with enemas and laxatives has to be replaced with a special diet prescribed 2 days before the study. In some cases, the use of a contrast enema can accelerate perforation or cause toxic dilatation of the colon. Therefore, irrigoscopy is performed after the subsidence of acute phenomena. This method reveals unevenness and "graininess" of the mucosa, thickening of the intestinal wall, ulceration, pseudopolyposis, lack of haustration. Differential diagnosis of nonspecific ulcerative colitis is carried out primarily with acute intestinal infections. In the presence of an epidemic of intestinal infections, the diagnosis is easily established. But even in the case of sporadic morbidity in acute intestinal infections, the colitis syndrome flows without relapses, while ulcerative colitis has a relapsing course. The most accurate methods for identifying acute intestinal infection include bacteriological and serological. Often, ulcerative colitis is differentiated from Crohn's disease. In typical cases, Crohn's disease differs from nonspecific colitis in the absence of damage to the rectum, frequent involvement of the ileum in the pathological process, and segmental lesions of the intestinal wall. The definitive diagnosis can be made by detecting Crohn's disease-specific lymphoid granulomas in biopsy specimens. With granulomatous colitis, paraproctitis and pararectal fistulas are detected more often than with nonspecific ulcerative colitis. In some cases, it becomes necessary to distinguish between ulcerative colitis and intestinal tuberculosis. For intestinal tuberculosis, a certain localization of the process is characteristic (ileum, ileocecal region), segmental intestinal damage. But sometimes with intestinal tuberculosis, the rectum and the entire large intestine are affected. The colonoscopic picture of intestinal tuberculosis is characterized by the presence of ulcers with raised edges filled with grayish contents. Tuberculous ulcers tend to spread in a transverse direction and leave behind short scars in which ulcers reappear. With nonspecific ulcerative colitis, scars do not form at the site of former ulcers. In elderly and senile patients, ulcerative colitis should be differentiated from ischemic colitis. The latter is characterized by intense, paroxysmal pain in the abdomen 20-30 minutes after eating, while in ulcerative colitis pain occurs before the act of defecation. The most important radiological sign is the "thumbprint" symptom. The endoscopic picture of ischemic colitis is characterized by sharply defined boundaries of the lesion, submucosal hemorrhages, cyanotic pseudopolypous formations protruding into the intestinal lumen. Histological examination reveals hemosiderin-containing cells and fibrosis. The absence of contact bleeding at the time of the biopsy is also more indicative of ischemic colitis. Treatment. The absence of a single etiological factor and the complexity of the pathogenesis of nonspecific ulcerative colitis make the treatment of this disease difficult. Drugs that have anti-inflammatory and antibacterial effects are used: salazopyridazine, sulfasalazine, salazodimethoxin, salofalk. Sulfasalazine taken orally, with the participation of intestinal microflora, breaks down into 5-aminosalicylic acid and sulfapyridine. Unabsorbed sulfapyridine inhibits the growth of anaerobic microflora in the intestine, including clostridia and bacteriodes. And thanks to 5-aminosalicylic acid, the drug not only causes changes in the intestinal microflora, but also modulates immune reactions and blocks mediators of the inflammatory process. The drug is prescribed at a dose of 2-6 g per day for the entire period of active inflammation. When the colitic syndrome subsides, the dose of sulfasalazine is reduced gradually, bringing it to maintenance (on average 1-1,5 tablets per day). The appointment of 5-aminosalicylic acid derivatives (salofalk, mesacol, salosan, tidikol) is the basic method and can be used as monotherapy for mild and moderate forms of ulcerative colitis. The treatment is carried out against the background of diet therapy with the exception of dairy products, in the presence of a balanced content of proteins, fats, carbohydrates and vitamins in the diet. It is advisable to exclude fresh fruits, vegetables, canned food. Food should be mechanically and chemically gentle. Feed fractional 4-5 times a day. Vitamin imbalance disrupts the process of absorption of microelements and is compensated by the appointment of complex preparations in tablets ("Duovit", "Oligovit", "Unicap"). In severe diarrheal syndrome in persons with mild and moderate course of the disease, the appointment of sandostatin is indicated, which inhibits the synthesis of gastrointestinal hormones and biogenic amines (vasoactive intestinal peptide, gastrin, serotonin), the production of which is sharply increased in ulcerative colitis and Crohn's disease. And also the drug reduces secretion and improves absorption in the intestine, inhibits visceral blood flow and reduces motility. When using sandostatin (within 7 days at a dose of 0,1 mg 2 times, subcutaneously), diarrhea decreases, tenesmus practically disappears, and blood excretion with feces decreases. In a severe form of nonspecific ulcerative colitis, treatment is carried out against the background of parenteral nutrition. The protein content of these preparations should be approximately 1,5-2,0 g/kg of body weight. Corticosteroids, which are administered parenterally, are a pathogenetic treatment for a severe form of the disease: during the first day, prednisone is administered intravenously at intervals of 12 hours (90-120 mg or more), in the next 5 days - intramuscularly, gradually reducing the dose. With a positive effect, they switch to oral medication (prednisolone 40 mg per day). Long-term administration of hormones during a period of stable remission is not advisable. In patients with a severe course of the disease, a positive effect of hyperbaric oxygenation (HBO) was noted. The use of a course of HBO (7-10 procedures) during the period of remission can reduce the frequency of relapses. Indications for emergency surgical treatment: intestinal perforation, toxic dilatation, profuse intestinal bleeding, malignancy. In the moderate form of the course of nonspecific ulcerative ulcer, a strict diet is required with a restriction of fiber, dairy products and a high protein content. Prednisolone is administered orally at an initial dose of 20-40 mg per day. Treatment can be supplemented with sulfasalazine and its analogues, which are taken orally or administered in microclysters and suppositories into the rectum. The initial dose of sulfasalazine is 1 g per day, then it is increased to 4-6 g. As an auxiliary method of treatment, decoctions of herbs with anti-inflammatory and hemostatic effects (burnet root, nettle leaf, lichen, gray alder cones, licorice root) can be used, herbal medicine often allows you to reduce the dose of salazopreparations, prolong remission. Prognosis and prevention. In severe cases and the presence of systemic and local complications, the prognosis is serious. The patients are completely unable to work. In mild and moderate forms of the disease, the prognosis for life is favorable. Patients need to be transferred to light work. During the period of remission, maintenance treatment with salazopreparations, bacterial agents, psychotherapy, and diet therapy is recommended. Patients suffering from nonspecific ulcerative colitis for a long time (more than 5-7 years) should be assigned to the risk group for the occurrence of bowel cancer and put on dispensary records. These patients are shown once a year colonoscopy with targeted biopsy. LECTURE No. 15. Diseases of the kidneys. Acute glomerulonephritis Acute glomerulonephritis (AGN) is an acute diffuse kidney disease of an infectious-allergic nature, localized in the glomeruli. AGN can be an independent disease (primary) or be secondary as part of another disease, complicating the clinical picture and diagnosis of the latter. AGN usually affects young and middle-aged men. Etiology. AGN occurs most often after a coccal infection (influenza, acute tonsillitis, pharyngitis caused by so-called nephritogenic strains of microorganisms). In 60-80% of patients, group A β-hemolytic streptococcus is detected; in 1/3 of cases, the etiology of AGN cannot be established. Prolonged hypothermia, especially in conditions of high humidity, contributes to the development of AGN. Vaccination is also a factor in the onset of the disease, and in 75% of cases the kidneys are affected after the second or third injection. Pathogenesis. The pathogenesis of the disease has an immune mechanism: when antigens (streptococcal, medicinal, foreign proteins) enter the body, antibodies are formed in response, binding these antigens and, together with the 3rd fraction of complement, forming immune complexes circulating in the vascular bed. The complexes are capable of depositing on the outer side of the basement membrane of the glomerular capillaries, causing their damage through the release of complement breakdown products, which increase the permeability of the capillaries and cause local changes in the latter. Neutrophils rush to the sites of deposition of immune complexes, whose lysosomal enzymes aggravate damage to the endothelium and basement membrane, separating them from each other. Platelet degranulation causes the release of serotonin, leading to hemocoagulation and fibrin deposition on the basement membrane. The elimination of immune complexes from the body is facilitated by a macrophage reaction in the form of proliferation of mesangial and endothelial cells, with the effectiveness of this process, recovery occurs. clinical picture. The clinical picture of the disease consists of the following syndromes. urinary syndrome. 1. Proteinuria due to the passage of protein molecules through the spaces of the capillary wall of the glomerulus, formed during the deposition of immune complexes on them. Proteinuria is selective in nature, in which predominantly albumins pass through the glomerular "filter". 2. Hematuria due to involvement in the pathological process of capillary mesangium and interstitial tissue. Erythrocytes penetrate through the smallest breaks in the basement membrane, changing their shape. 3. Cylindruria - urinary excretion of cylindrical cells of the tubules. During dystrophic processes in the tubules of the disintegrated cells of the renal epithelium, granular cylinders are formed, consisting of a dense granular mass; waxy cylinders have sharp contours and a homogeneous structure; hyaline casts are proteinaceous formations. Hypertensive syndrome is observed due to: 1) sodium and water retention; 2) activation of the renin-angiotensin-aldosterone and sympathoadrenal systems; 3) decrease in the function of the depressor system of the kidneys. Edema syndrome is associated with the following factors: 1) a decrease in glomerular filtration due to their defeat; 2) a decrease in the filtration charge of sodium and an increase in its reabsorption; 3) water retention due to sodium retention in the body; 4) an increase in BCC; 5) secondary hyperaldosteronism; 6) an increase in the secretion of ADH and an increase in the sensitivity of the distal nephron to it, leading to fluid retention; 7) an increase in the permeability of the capillary walls and the release of plasma into the tissues; 8) a decrease in plasma oncotic pressure with massive proteinuria. Complaints presented in AGN are not specific and occur in various diseases. It is very important to indicate in the anamnesis a recent sore throat, exacerbation of chronic tonsillitis, hypothermia, etc. Some patients note a decrease in urine output, combined with some swelling (pasto) of the face in the morning. In 1/3-3/4 patients in the first days of the disease, there are not very strong, aching pains in the lumbar region associated with an increase in the size of the kidneys. There are also increased fatigue, headache, shortness of breath during physical exertion, a short-term increase in body temperature to subfebrile. Arterial hypertension, detected only in half of the patients, is characterized by an increase in numbers to 140-160 / 85-90 mm Hg. Art. (rarely - up to 180/100 mm Hg. Art.). Diagnostics. In 100% of cases, urine examination reveals proteinuria of varying severity, cylindruria and, what is most important for diagnosis, hematuria of varying severity - from microhematuria (up to 10 red blood cells in the field of view) to macrohematuria (albeit quite rare). However, if AGN is suspected, it is necessary to conduct a series of repeated urine tests or perform a Nechiporenko test (determining the number of formed elements in 1 μl), since red blood cells may not be detected in a single portion of urine. When examining the blood, acute phase indicators are detected (increase in the content of fibrinogen and α2-globulin, C-reactive protein, ESR acceleration), the number of leukocytes changes little, moderate anemia. In an uncomplicated course of AGN, the content of nitrogenous substances (creatinine, indican, urea) in the blood does not change. In the initial phase of the disease, a change in the Reberg test is observed - a decrease in glomerular filtration and an increase in tubular reabsorption, which normalizes as it recovers. An x-ray examination in patients with severe arterial hypertension may show a moderate increase in the left ventricle, which takes on the same size as the patient recovers. There are 3 clinical variants of AGN. 1) Monosymptomatic variant: minor complaints, absence of edema and arterial hypertension, there is only urinary syndrome; the most common variant of the course of the disease (86% of cases). 2) Nephrotic variant: edema, oliguria are pronounced, it is possible to increase blood pressure to relatively low numbers, it is detected in 8% of patients. 3) Extended version: arterial hypertension, reaching high numbers (180/100 mm Hg. Art.), moderately pronounced edema, circulatory failure, occurs in 6% of cases. Differential diagnostics. AGN must be distinguished from chronic glomerulonephritis, which is not difficult with the acute onset of AGN and subsequent complete reversal of symptoms. However, in the absence of an acute onset, as well as in the long-term persistence of certain signs of the disease, diagnosis becomes significantly more complicated. If differentiation is difficult, a puncture biopsy of the kidney is resorted to. It is difficult to differentiate AGN from pyelonephritis due to the presence of leukocyturia in both diseases. However, AGN is accompanied by more massive proteinuria and, in some cases, edema. Differential diagnosis is also helped by the clinical symptoms of pyelonephritis in the form of more pronounced pain in the lower back, accompanied by fever and dysuric disorders. Also of diagnostic value is the definition of bacteriuria in pyelonephritis, the identification of "active" leukocytes, as well as x-ray (deformation of the cups) and isotope-renographic (asymmetry of kidney function) studies. AGN as an independent disease must be differentiated from chronic diffuse connective tissue diseases, in which AGN is one of the manifestations of the disease. This situation usually occurs with the severity of urinary, hypertensive and edematous syndromes and insufficient clarity of other symptoms of the disease, more often with SLE (systemic lupus erythematosus). The correct diagnosis in SLE can be made by taking into account the articular syndrome, damage to the skin and other organs (heart), pronounced immunological changes (detection of anti-organ antibodies in high titer, lupus erythematosus cells, antibodies to DNA and RNA), as well as monitoring the dynamics of the clinical picture. Treatment. Treatment for AGN is complex and includes the following measures. 1. Mode. If AGN is suspected or immediately after the diagnosis is established, the patient should be immediately hospitalized. Strict bed rest must be observed for about 2-4 weeks until the elimination of edema and normalization of blood pressure. Staying in bed provides uniform warming of the body, which leads to a decrease in vasospasm (hence, to a decrease in blood pressure) and to an increase in glomerular filtration and diuresis. After discharge from the hospital, home treatment is indicated for up to 4 months from the date of onset of the disease, which is the best prevention of the transition of AGN to the chronic stage. 2. Diet. Depending on the severity of clinical symptoms, it is very important to restrict fluid and sodium chloride. With an expanded and nephrotic form, a complete fast is recommended for 1-2 days with fluid intake in an amount equal to diuresis. On the 2-3rd day, the consumption of food rich in potassium salts (rice porridge, potatoes) is shown. The total amount of water drunk per day should be equal to the volume of urine allocated for the previous day plus 300-500 ml. After 3-4 days, the patient is transferred to a diet with protein restriction (up to 60 g per day), and the total amount of salt is not more than 3-5 g / day. Such a diet is recommended until the disappearance of all extrarenal symptoms and a sharp improvement in urinary sediment. 3. Drug therapy includes, first of all, antibacterial therapy, which, however, should be carried out only if the infectious nature of AGN is reliably established (the pathogen has been isolated and no more than 3 weeks have passed since the onset of the disease). Usually prescribed penicillin or its semi-synthetic analogues in conventional dosages. The presence of obvious foci of chronic infection (tonsillitis, sinusitis, etc.) is also a direct indication for antibiotic therapy. Diuretics in the treatment of AGN are indicated only with fluid retention, increased blood pressure and the appearance of heart failure. The most effective furosemide (40-80 mg), used until the elimination of edema and hypertension. There is no need for a long-term prescription of these drugs, 3-4 doses are enough. In the absence of edema, but persistent hypertension or with an insufficient antihypertensive effect of saluretics, antihypertensive drugs (clophelin, dopegyt) are prescribed with a duration of administration that depends on the persistence of arterial hypertension. In the nephrotic form of AGN, immunosuppressive therapy is prescribed (corticosteroids - prednisone 60-120 mg per day, followed by a gradual decrease in dose, duration of use for 4-8 weeks). In case of AGN with severe edema and a significant decrease in diuresis, heparin is administered at 20-000 IU per day for 30-000 weeks, achieving an increase in blood clotting time by 4-6 times. With prolonged proteinuria, indomethacin or voltaren is prescribed at 75-150 mg per day (in the absence of hypertension and oliguria). The prognosis is favorable, however, with prolonged forms, there is a possibility that the process will become chronic. Prevention of AGN comes down to effective treatment of focal infection, rational hardening. In order to timely detect the onset of the disease after vaccination, transferred ARVI in all patients, it is necessary to examine the urine. LECTURE No. 16. Diseases of the kidneys. Pyelonephritis Pyelonephritis is an infectious disease in which the renal pelvis, its calyces and the substance of the kidneys are involved in the process, with a predominant lesion of the interstitial tissue. In this regard, pyelonephritis is interstitial (interstitial) nephritis. This is a broader concept than pyelonephritis. It denotes, firstly, a type of inflammation of the kidneys of any etiology with predominant involvement of the interstitium, and secondly, a special disease in which this inflammation is its only and main expression. Close to interstitial nephritis is the so-called tubulo-interstitial nephritis, in which there is a friendly lesion of the tubules and stroma of the kidneys. Classification. Based on clinical and morphological data, acute and chronic pyelonephritis is distinguished, which usually has a recurrent course in the form of attacks of acute pyelonephritis. Also, pyelonephritis can be one- and two-sided. According to the form of the course (for chronic pyelonephritis): recurrent form, latent chronic pyelonephritis, pyelonephritic wrinkled kidney. Etiology and pathogenesis. Pyelonephritis is an infectious disease. Its causative agents are infectious agents of a nonspecific nature: E. coli, enterococcus, staphylococcus and other bacteria, but in most cases we are talking about E. coli (40%) and mixed flora (38%). Attention is drawn to the L-forms of bacteria, protoplasts (the bodies of bacteria, devoid of membranes that can support infection), candida, which can cause chronic pyelonephritis. Sources of infection can be tonsillas, diseases of the genital organs and large intestine, i.e. infectious agents can penetrate the kidney, including the pelvis, with the blood stream (hematogenous descending pyelonephritis), which is observed in many infectious diseases (typhoid fever, influenza , angina, sepsis). More often, microbes are brought into the kidneys in an ascending way from the ureters, bladder, urethra (urogenic ascending pyelonephritis), which is facilitated by dyskinesia of the ureters and pelvis, increased intrapelvic pressure (vesicorenal and pyelorenal reflux), as well as reabsorption of the contents of the pelvis into the veins of the renal medulla ( pyelovenous reflux). Ascending pyelonephritis, as a rule, complicates those diseases of the genitourinary system, in which the outflow of urine is difficult (stones and strictures of the ureters, strictures of the urethra, tumors of the genitourinary system), so it often develops during pregnancy. Lymphogenic infection in the kidneys (lymphogenic pyelonephritis) is also possible, when the colon and genital organs are the source of infection. For the development of pyelonephritis, in addition to the penetration of infection into the kidneys, the reactivity of the body and a number of local causes that cause a violation of the outflow of urine and urinary stasis are of great importance. The same reasons explain the possibility of a recurrent chronic course of the disease. Infected microorganisms with functional and morphological changes in the urinary tract leading to urinary stasis, impaired venous and lymphatic outflow from the kidney, contributing to the fixation of infection in the kidneys, cause focal and polymorphic zones of inflammatory infiltrates and suppuration of the interstitium of one or both kidneys. The interstitial tissue of the tubules is affected, and then the nephrons. There are productive endarteritis, hyperplasia of the middle shell of the vessels, the phenomena of hyalinosis, arteriolosclerosis develop up to the secondary wrinkled kidney. In recent years, a certain role in the development of chronic pyelonephritis is assigned to autoimmune reactions: under the influence of bacterial antigens, immunoglobulin G and complement are deposited on the basement membrane of the glomerular capillaries, causing its damage. The transition of acute pyelonephritis to chronic is facilitated by: belated diagnosis of acute pyelonephritis, untimely hospitalization, the presence of chronic infections, diabetes mellitus, gout, and the abuse of analgesics - phenacetin. Chronic pyelonephritis is more common in women (50%), which is facilitated by pregnancies, especially repeated ones (estrogens cause atony of the smooth muscles of the urinary tract), in childhood in girls, which is associated with the structure of the urinary tract, their anomalies. clinical picture. As mentioned above, both acute and chronic course of pyelonephritis is possible. The clinical picture of the acute phase of the disease is characterized by a sudden, sharp increase in body temperature up to 39-40 ° C, the onset of weakness, headache, chills, combined with profuse sweating, nausea and vomiting may occur. Along with the rise in body temperature, pains appear in the lumbar region, which, as a rule, are noted on one side. The nature of the pain is dull, their intensity is different. In the case of the development of the disease against the background of urolithiasis, an attack of pyelonephritis is preceded by an attack of renal colic. In the absence of adequate therapy, the disease can become chronic, or this leads to the development of suppurative processes in the kidney, which are clinically manifested by a deterioration in the general condition of the patient and sudden changes in temperature (from 35-36 ° C in the morning to 40-41 ° C in the evening). Chronic pyelonephritis is, as a rule, a consequence of undertreated acute pyelonephritis, when it was possible to remove acute inflammation, but it was not possible to radically destroy all pathogens in the kidney, nor to restore the physiological outflow of urine from the kidney. Chronic pyelonephritis is disturbed by constant dull aching pains in the lumbar region, aggravated in damp cold weather. Also, chronic pyelonephritis is prone to periodic exacerbations, when the patient has all the signs of an acute process. Diagnostics. The problem of diagnosing the disease is due to the fact that the symptoms of pyelonephritis are similar to the symptoms of other diseases resulting from inflammation of the urinary tract. The diagnostic examination plan includes blood tests, urine tests, as well as studies showing the state of the urinary system: ultrasound of the kidneys, X-ray studies, PCR analysis for an infectious agent. To verify the type of infectious agent, it is necessary to conduct a bacteriological culture of a urine sample, and the method of computed tomography is used to exclude tumor processes. Thus, laboratory and special research methods are of great importance for the recognition of the disease. And in chronic pyelonephritis, the decisive, and sometimes the only manifestations are changes in the urine, blood and urinary tract. It is necessary to dynamically monitor blood pressure and weight of the patient. Leukocytosis, increased ESR, neutrophilic shift are noted in the blood, an increase in the level of residual nitrogen (at a norm of 20-40 mg), urea (norm 40-60 mg), creatinine (norm 53-106 μmol / l), indican (norm 1,41, 3,76-180 µmol/l), cholesterol (norm 200-83 mg), blood chlorides (norm XNUMX mmol/l). Important for the diagnosis of changes in the urine: a decrease in specific gravity, proteinuria (including daily), hematuria and cylindruria. However, methods for quantitative determination of the formed elements of urine sediment are gaining increasing diagnostic importance: Kakovsky-Addis (normal leukocytes up to 4 million; red blood cells - up to 1 million, cylinders - up to 2 thousand in 24 hours), Amburger (normal leukocytes up to 2000 , red blood cells - up to 1400, casts - up to 20 per 1 min), Nechiporenko (normal leukocytes up to 2500, red blood cells - up to 1000, casts - up to 20 in 1 ml of freshly released urine). The ratio of the absolute number of erythrocytes and leukocytes in the urine sediment with pyelonephritis changes dramatically towards a significant predominance of leukocytes by 10-20 times. In chronic pyelonephritis, Stenheimer-Malbin cells appear in the urine: large leukocytes, with Brownian movement of cytoplasmic granules, appearing with a decrease in the osmotic properties of urine (specific gravity below 10-14), stained blue with gentian violet and safronin, "active" leukocytes: altered leukocytes , possessing the Brownian motion of the protoplasm, revealed when stained with a 1% aqueous solution of methylene blue with the addition of distilled water. The diagnostic value of an increase in the number of "active" leukocytes and Stenheimer-Malbin cells (up to 40%), bacteriuria (microbial count more than 100 thousand per 1 ml of urine), nitrite test (with a microbial count of more than 100 thousand U, microbes decompose urine nitrites) are emphasized. , with the addition of sulfanilic acid and L-naphthylamine, a red color appears), a colorimetric TTX test (under the action of microbial dehydrogenases, triphenyltetrazolyte chloride is reduced to red insoluble triphenylformazan within 4-10 hours at a temperature of -37 ° C), a provocative prednisolone test (the patient collects in a sterile dish, the middle portion of urine is the control one, then 30 mg of prednisolone in 10 ml of saline is slowly injected into the vein and the middle portion of urine is collected three times at hourly intervals and after 24 hours; in chronic pyelonephritis, the number of leukocytes, bacteria doubles, "active" leukocytes appear , at least in one portion), antibiograms. Particular attention should be paid to the microscopy of tuberculosis of the kidneys (microscopy of smears stained according to Tsil, sowing urine on special media - the method of Preis and Shkolnikova, the biological method). If a unilateral process is suspected, it is necessary to conduct a urine test, separately taken from each kidney with special catheters. An important role in the diagnosis of chronic pyelonephritis is played by radiological research methods: survey radiography and tomography (characterize the position, size and shape of the kidneys), excretory and retrograde pyelography (decrease in the concentration and excretory ability of the kidneys, spasms, anomalies, deformities of the pelvis, calyces), pneumopyelography (for recognition of non-contrast stones), renal angiography (reveals a violation of vascular architectonics - arteries and veins). To determine the safety of the function, and the parenchyma of the kidneys, especially with a unilateral process, radioindication methods are used - renography (hippuran iodine 131) and scanography (using neohydride Hg 203). Puncture biopsy in the case of pyelonephritis due to the foci of the process may not provide information. Chromocystoscopy may indicate kidney damage. Treatment. Most often, therapy for pyelonephritis is conservative, however, if acute pyelonephritis is purulent, surgical intervention may be required. Conservative treatment consists of a regimen, diet, the use of antibiotics, as well as various drugs that stabilize the function of the kidneys and the patient’s body as a whole. In acute pyelonephritis, strict bed rest is indicated. The food should be consumed foods containing the optimal amount of proteins, fats and carbohydrates. In the acute period, it is necessary to alternate protein and plant foods. With severe intoxication, you need to drink plenty of water. Treatment of chronic pyelonephritis consists of the impact on the infection (etiotropic) in primary pyelonephritis and the elimination of one or another cause in secondary pyelonephritis, pathogenetic mechanisms and treatment of complications. The most effective treatment is after determining the antibiogram. Continuous (at least 2 months) treatment with antibacterial drugs is carried out. Immediately upon admission, an antibiotic, sulfanilamide or nitrofuran drug is prescribed. After 1-10 days, the drugs are changed, the treatment is carried out until the persistent disappearance of leukocyturia and bacteriuria. As soon as the exacerbation is eliminated, intermittent treatment with one of the antibacterial agents is carried out for 4-5 months: the drug is given for 7 days, then a break is taken for 8-10 days, or the drug is given for 10 days with an interval of 15-20 days, or the drug is given for 15 days, the interval is made for 15 days, then antimicrobial therapy is prescribed again. The duration of treatment and intervals is determined by clinical symptoms and laboratory control. It should be pointed out that in case of pyelonephritis that has developed in a patient with chronic tonsillitis, antibiotics of the penicillin series are most effective; in case of genital infections in men and women, broad-spectrum antibiotics are used (see Table 12). In the presence of gram-negative flora, treatment with nalidixic acid gives good results (blacks, ievigramon - 1,0 g 4 times a day for 7 days, but its preparations should be prescribed less frequently than other drugs (2 times)). Of the sulfa drugs, etazol (1,0 g 4 times - 10 days), solafur (0,1 g 3 times), long-acting sulfonamides are used. Also, courses are treated with furazolidone, furadonin, furagin (0,1 g 4 times a day). It must be emphasized that renal function should be determined before starting treatment. Long-term antibiotic therapy should be carried out with a glomerular filtration rate of at least 30 ml / min or with a residual nitrogen content in the blood serum of not more than 70 mg. An indicator of the effectiveness of the drug after a week of treatment is a decrease in the microbial count to 10 in 000 ml of urine. It is possible to reduce the virulence of microflora and increase the effectiveness of antibacterial agents by changing the reaction of urine every 10-14 days. Alkalinizing food, sodium citrate (10 g per day), alkaline mineral waters help to reduce pH reactions. Some antibacterial action has sodium benzoate (4-6 g per day), which is abundant in cranberries and bearberries. Pathogenetic therapy should be aimed at increasing the body's reactivity, improving urine outflow, and normalizing blood pressure. To activate immunobiological reactivity, α-globulin, autohemotherapy, blood transfusion, vaccine therapy are used (autovaccine treatment is carried out for 30-40 days, 0,1 ml subcutaneously or 0,2-0,3 ml every 2 days), staphylococcal toxoid ( 0,1-0,3-0,5-0,7-1,0-1,2-1,7-2,0 ml every 3 days). Diuretic herbs (bearberry, juniper berries, field horsetail, orthosiphon leaf - kidney tea, lingonberry leaf), antispasmodics (papaverine, no-shpa, etc.) help to normalize the outflow of urine. If there is an obstruction to the flow of urine, surgical treatment is indicated. With concomitant hypertension, rauwolfia preparations are indicated - isobarine, dopegyt, hemiton, saluretics, aldosterone antagonists. Prevention and prognosis. Prevention of pyelonephritis consists of primary and secondary measures. Primary prevention includes, first of all, the treatment of diseases that can lead to the development of pyelonephritis: focal infections, urological diseases (such as urolithiasis, prostate adenoma, as well as any diseases accompanied by a violation of the outflow of urine from the kidney), recreational activities. Table 12 Comparative efficacy of antibacterial drugs in pyelonephritis
Secondary prevention includes the detection of bacteriuria during preventive examinations (for example, pregnant women should conduct a bacteriological analysis of urine at least once a month), the appointment of anti-relapse treatment: the first week of each month - a pause in treatment: rosehip decoction, the second, third week - herbal diuretics and antiseptics, the fourth week - antibacterial agents (nitrofurans, antibiotics, antiseptics, once a year - nevigramon 1 g 1 times during the week and 1,0 g - during the second week, or 4-NOC 2-5 mg 100 times a day 150-4 days). Anti-relapse treatment is carried out for 2-3 years. Dispensary examinations with treatment should be carried out 3-4 times a year or 4-6 times. Forecast. The prognosis depends on the stage of the disease. Spa treatment. Sanatorium-resort treatment is indicated during the period of remission, especially for patients with secondary calculous pyelonephritis after urological operations (Truskavets, Sairme, Zheleznovodsk, Berezovsky mineral waters), where patients take low-mineralized waters. Sanatorium-resort treatment is contraindicated in case of high hypertension, severe anemia and obvious renal failure. Complications of pyelonephritis are varied. In acute pyelonephritis, the progression of the purulent process leads to the fusion of large abscesses and the formation of a carbuncle of the kidney, the communication of purulent cavities with the pelvis (pyonephrosis), the transition of the process to a fibrous capsule (perinephritis) and perinephric tissue (paranephritis). Acute pyelonephritis can be complicated by necrosis of the papillae of the pyramids (papillonekrosis), which develops as a result of the direct toxic effect of bacteria in conditions of urinary stasis. This complication of pyelonephritis occurs in most cases in patients with diabetes. Rarely, pyelonephritis becomes a source of sepsis. With the restriction of the purulent process during the scarring period, abscesses surrounded by a pyogenic membrane (chronic kidney abscess) can form. In chronic pyelonephritis, especially unilateral, it is possible to develop nephrogenic hypertension and arteriolosclerosis in the second (intact) kidney. Bilateral pyelonephritic wrinkling of the kidneys leads to chronic renal failure. The outcome of acute pyelonephritis is usually recovery, but as a result of complications (pyonephrosis, sepsis, papilonecrosis), death may occur. Chronic pyelonephritis with wrinkling of the kidneys often ends with azotemia uremia. With the development of arterial hypertension of renal origin, lethal outcome in chronic pyelonephritis is sometimes associated with the complications that occur in hypertension (cerebral hemorrhage, myocardial infarction, etc.). Author: Mostovaya O.S.
▪ Civil law. Special part. Crib
Artificial leather for touch emulation
15.04.2024 Petgugu Global cat litter
15.04.2024 The attractiveness of caring men
14.04.2024
▪ Cellular cleansing saves from atherosclerosis ▪ High Performance Samsung 950 Pro SSDs ▪ Changing red blood cells to activate the immune system against covid
▪ section of the site Microphones, radio microphones. Article selection ▪ article Topic of the day. Popular expression ▪ article Locksmith-picker. Standard instruction on labor protection ▪ article Introductory device. Encyclopedia of radio electronics and electrical engineering ▪ article Three fountains. physical experiment
Home page | Library | Articles | Website map | Site Reviews www.diagram.com.ua |






 Arabic
Arabic Bengali
Bengali Chinese
Chinese English
English French
French German
German Hebrew
Hebrew Hindi
Hindi Italian
Italian Japanese
Japanese Korean
Korean Malay
Malay Polish
Polish Portuguese
Portuguese Spanish
Spanish Turkish
Turkish Ukrainian
Ukrainian Vietnamese
Vietnamese








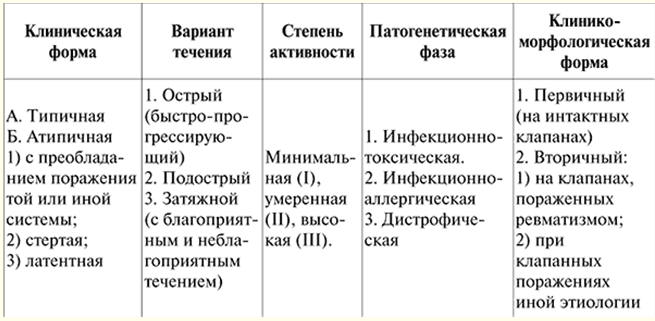








 See other articles Section
See other articles Section 